Acute Biphenotypic Leukemia Explained in Simple Terms

Acute biphenotypic leukemia is a rare type of blood cancer that affects both myeloid and lymphoid cells, which are essential for your immune system and blood function. Unlike other leukemias, it shows characteristics of two cell types, making it harder to diagnose and treat. This condition accounts for only 1% to 5% of all acute leukemias, with an estimated 0.35 cases per million people each year.
Understanding this disease is crucial for you and your caregivers. Its mixed nature can complicate treatment, and relapsed cases often resist therapy. Knowing its features helps you navigate treatment options and manage expectations about outcomes.
Key Takeaways
Acute biphenotypic leukemia is a rare blood cancer. It affects both myeloid and lymphoid cells, making treatment harder.
Symptoms are feeling very tired, getting sick often, and bruising easily. Finding it early helps with better treatment results.
Treatments include chemotherapy, special medicines, and stem cell transplants. Care to ease symptoms is also very important.
Learning about this leukemia helps patients and families handle treatment. It also helps them know what to expect.
Staying informed and joining support groups can help patients. This gives them strength to face this tough disease.
What Is Acute Biphenotypic Leukemia?

A Rare and Complex Type of Leukemia
Acute biphenotypic leukemia is one of the rarest forms of leukemia. It accounts for only a small percentage of all acute leukemia cases. What makes it unique is its ability to display characteristics of both myeloid and lymphoid cells. These are two distinct types of blood cells that normally serve different roles in your body. This dual nature complicates its diagnosis and treatment.
Patients with this condition often show a higher expression of the CD34 antigen, a marker linked to immature blood cells. They also tend to have complex chromosomal abnormalities. These abnormalities can lead to a higher risk of relapse and resistance to therapy. Additionally, extramedullary infiltration, where leukemia spreads outside the bone marrow, occurs more frequently in this type of leukemia.
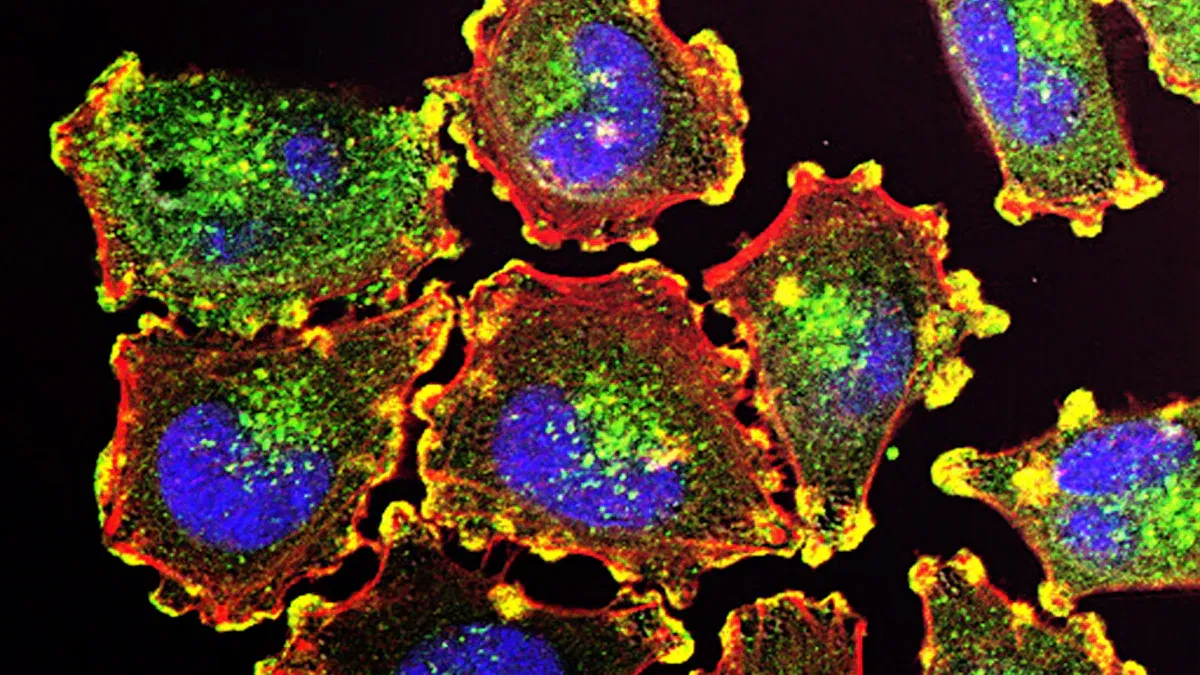
How It Affects Blood and Bone Marrow
Acute biphenotypic leukemia disrupts the normal functioning of your blood and bone marrow. The bone marrow, which produces blood cells, becomes overwhelmed by abnormal cells. This leads to a shortage of healthy red blood cells, white blood cells, and platelets.
You might experience symptoms like fatigue and frequent infections due to low red and white blood cell counts. Bruising and prolonged bleeding are also common because of reduced platelet levels. Severe anemia often requires blood transfusions, while persistent fever and infections can result in dangerous complications.
Why It Is Called "Biphenotypic"
The term "biphenotypic" reflects the condition's unique biological nature. It arises from multipotent progenitor cells, which can develop into both myeloid and lymphoid cells. These leukemia cells coexpress markers from both lineages, making them distinct from other types of leukemia. For example, you might see a mix of B-lymphoid and myeloid markers in the same patient. This dual identity is what gives the disease its name and contributes to its complexity.
How Acute Biphenotypic Leukemia Differs From Other Types of Leukemia
Comparison With Acute Myeloid Leukemia (AML)
Acute biphenotypic leukemia and acute myeloid leukemia (AML) share some similarities, but they differ in key ways. The table below highlights these differences:
Feature | Acute Biphenotypic Leukemia (BAL) | Acute Myeloid Leukemia (AML) |
|---|---|---|
CD34 Positive Rates | Higher incidence | Lower incidence |
Karyotype Abnormalities | More complex abnormalities | Fewer abnormalities |
t(9;22) Incidence | Significant presence | Rare occurrence |
Extramedullary Infiltration | More frequent | Less frequent |
Treatment Resistance | Higher resistance after relapse | Lower resistance |
These differences make acute biphenotypic leukemia more challenging to treat. For example, its higher resistance to therapy after relapse often requires more aggressive treatment strategies.
Comparison With Acute Lymphoblastic Leukemia (ALL)
Acute biphenotypic leukemia also differs from acute lymphoblastic leukemia (ALL) in terms of symptoms and progression. While both conditions can cause fatigue, infections, and bruising, acute biphenotypic leukemia tends to have a poorer prognosis. This is due to its higher expression of the CD34 antigen, more complex chromosomal abnormalities, and increased rates of relapse. Additionally, extramedullary infiltration, where the disease spreads beyond the bone marrow, occurs more frequently in acute biphenotypic leukemia. These factors contribute to its more aggressive nature compared to ALL.
Key Features That Set It Apart
What makes acute biphenotypic leukemia truly unique is its dual identity. Unlike AML or ALL, this condition involves cells that display markers from both myeloid and lymphoid lineages. This mixed nature complicates diagnosis and treatment, as therapies must target both cell types. The disease also shows a higher likelihood of chromosomal abnormalities, such as the t(9;22) translocation, which is rare in other leukemias. These features make it one of the most complex forms of leukemia to manage.
Symptoms and Diagnosis of Acute Biphenotypic Leukemia
Common Symptoms
Acute biphenotypic leukemia can cause a wide range of symptoms. These symptoms often result from the disruption of normal blood cell production. You may experience:
Lightheadedness or dizziness
Shortness of breath
Easy bruising or prolonged bleeding
Fever and night sweats
Frequent or severe infections
Enlarged lymph nodes, liver, or spleen
Swollen gums
Joint pain or headaches
Other symptoms, such as nausea, vomiting, or loss of appetite, may also occur. These signs can vary depending on how the disease progresses. If you notice any of these symptoms, consult a healthcare provider promptly.
Diagnostic Tests
Diagnosing acute biphenotypic leukemia involves several steps. Doctors use advanced tests to confirm the condition and understand its complexity.
Blood Tests
Doctors often begin with blood tests. A complete blood count (CBC) checks for abnormal levels of red blood cells, white blood cells, and platelets. A blood smear examines the shape and size of these cells under a microscope. These tests can reveal the presence of immature or abnormal cells, which may indicate leukemia.
Bone Marrow Biopsy
If blood tests suggest leukemia, a bone marrow biopsy is the next step. During this procedure, a small sample of bone marrow is removed, usually from your hip bone. This sample is analyzed to identify cancerous cells, known as blasts. The biopsy helps confirm the diagnosis and provides more details about the leukemia type.
Immunophenotyping and Genetic Testing
Immunophenotyping plays a crucial role in diagnosing acute biphenotypic leukemia. This test uses flow cytometry to analyze the markers on leukemia cells. It helps distinguish between myeloid and lymphoid lineages. Genetic testing further identifies chromosomal abnormalities, such as the t(9;22) translocation or MLL gene rearrangements. These tests provide critical information for tailoring your treatment plan.
Diagnosing acute biphenotypic leukemia can be challenging due to its rarity and complexity. However, advanced techniques like immunophenotyping and genetic analysis improve accuracy and help guide effective treatment strategies.
Treatment Options for Acute Biphenotypic Leukemia
Chemotherapy
Chemotherapy plays a central role in treating acute biphenotypic leukemia. Doctors often use regimens designed for either acute myeloid leukemia (AML) or acute lymphoblastic leukemia (ALL). The choice of regimen depends on the specific characteristics of your leukemia. Studies show that chemotherapy can lead to complete remission in some cases. For example, in a study involving ten patients, eight received chemotherapy, and five achieved complete remission. Four of these patients responded to ALL-specific chemotherapy, while one responded to AML-specific treatment.
However, chemotherapy comes with challenges. Relapse rates remain high, and the chances of achieving remission after relapse are low. Side effects can also be severe. Some patients experience complications that may even become life-threatening. Despite these difficulties, chemotherapy remains a critical first step in managing this complex disease.
Targeted Therapy
Targeted therapy offers a more precise approach by focusing on specific markers or mutations in leukemia cells. This method can improve remission rates and reduce damage to healthy cells. For instance, in a study of 21 patients with acute biphenotypic leukemia, 71.4% achieved complete remission after targeted therapy. However, maintaining remission remains a challenge due to high relapse rates.
Your doctor may recommend targeted therapy as part of a combination treatment plan. This approach aims to address the disease's complexity by targeting both myeloid and lymphoid markers. While targeted therapy shows promise, ongoing research seeks to improve its long-term effectiveness.
Stem Cell Transplant
Stem cell transplantation offers a potential cure for acute biphenotypic leukemia, especially for high-risk cases. Experts often recommend an allogeneic stem cell transplant after achieving remission through chemotherapy. This procedure replaces your damaged bone marrow with healthy stem cells from a donor.
Studies highlight its effectiveness. A retrospective study found that patients who underwent stem cell transplants between 2000 and 2014 had a three-year survival rate of about 56%. However, eligibility criteria are strict. You must meet specific requirements, such as being in remission and having adequate organ function. While the procedure carries risks, it remains one of the most effective options for improving long-term outcomes.
Stem cell transplantation offers hope for patients with acute biphenotypic leukemia. Discuss this option with your healthcare team to determine if it suits your condition.
Supportive Care
Supportive care plays a vital role in managing acute biphenotypic leukemia. It focuses on improving your quality of life and addressing complications caused by the disease or its treatment. While it doesn’t target the leukemia itself, supportive care helps you stay stronger during treatment.
Key Components of Supportive Care
Managing Infections: Your immune system may weaken due to low white blood cell counts. Doctors often prescribe antibiotics or antifungal medications to prevent or treat infections. Staying vigilant about hygiene and avoiding crowded places can also reduce your risk.
Blood Transfusions: Low red blood cell or platelet levels can cause fatigue, anemia, or excessive bleeding. Blood transfusions help restore these levels, improving your energy and reducing complications.
Nutritional Support: Eating well can be challenging during treatment. A dietitian may recommend high-calorie, nutrient-rich foods or supplements to maintain your strength. In some cases, intravenous nutrition may be necessary.
Pain Management: Bone pain or discomfort from treatments can affect your daily life. Your healthcare team may suggest medications, physical therapy, or relaxation techniques to ease the pain.
Tip: Keep a journal of your symptoms and side effects. Sharing this with your doctor helps them adjust your care plan to meet your needs.
Emotional and Psychological Support
Coping with a leukemia diagnosis can feel overwhelming. Supportive care includes mental health resources like counseling or support groups. Talking to others who understand your experience can provide comfort and reduce stress.
By focusing on these supportive measures, you can better manage the challenges of acute biphenotypic leukemia and maintain a higher quality of life throughout your treatment journey.
Prognosis and Living With Acute Biphenotypic Leukemia
Factors Influencing Prognosis
Several factors can influence your prognosis if you have acute biphenotypic leukemia. These include genetic abnormalities, white blood cell counts, and how well you respond to initial treatment. The table below highlights key factors and their impact:
Factor | Influence on Prognosis |
|---|---|
Genetic abnormalities | Poor prognosis |
White blood cell count | High count indicates worse outlook |
Extramedullary infiltration | Associated with poor outcomes |
Primary induction treatment | Affects overall prognosis |
Complete remission after induction | Critical for better prognosis |
Genetic abnormalities, such as chromosomal changes, often indicate a more aggressive disease. A very high white blood cell count at diagnosis can also signal a worse outlook. Achieving complete remission after initial treatment significantly improves your chances of long-term survival.
Importance of Early Diagnosis
Early diagnosis plays a critical role in improving outcomes. Identifying acute biphenotypic leukemia quickly allows doctors to start treatment sooner. This is especially important because the disease progresses rapidly. Proper classification of the leukemia type ensures you receive the most effective therapy. Studies show that timely chemotherapy and stem cell transplantation after remission can improve survival rates.
Coping With Challenges
Living with acute biphenotypic leukemia can feel overwhelming, but there are ways to manage the challenges. Focus on maintaining your physical and emotional health. Support groups and counseling can help you cope with the emotional toll of the disease. Staying informed about your condition empowers you to make better decisions about your care.
You may also face physical challenges, such as fatigue or side effects from treatment. Work closely with your healthcare team to address these issues. They can adjust your treatment plan or recommend supportive care options to improve your quality of life.
Tip: Keep a positive mindset and lean on your support network. Small steps can make a big difference in managing this complex disease.
Acute biphenotypic leukemia is a rare and complex blood cancer that affects both myeloid and lymphoid cells. Its symptoms, such as fatigue, infections, and bruising, can disrupt daily life. Early diagnosis and personalized treatment improve outcomes, even though the disease often resists therapy. While the prognosis can be challenging, advancements in treatment offer hope. Staying informed and working closely with your healthcare team can make a significant difference. Remember, you are not alone—support networks and medical teams are here to guide you through this journey.
FAQ
What makes acute biphenotypic leukemia different from other leukemias?
Acute biphenotypic leukemia involves cells with both myeloid and lymphoid markers. This dual nature makes it harder to diagnose and treat compared to other leukemias like AML or ALL, which involve only one cell type.
Can acute biphenotypic leukemia be cured?
Treatment can lead to remission, but a cure depends on factors like early diagnosis and response to therapy. Stem cell transplants offer the best chance for long-term survival in eligible patients.
How is acute biphenotypic leukemia diagnosed?
Doctors use blood tests, bone marrow biopsies, and immunophenotyping. These tests identify abnormal cells and their markers, helping confirm the diagnosis and guide treatment.
What are the main treatment options?
Treatment includes chemotherapy, targeted therapy, and stem cell transplants. Supportive care helps manage symptoms and side effects, improving your quality of life during treatment.
Is acute biphenotypic leukemia hereditary?
No, it is not typically inherited. Genetic mutations in blood cells cause the disease, but these mutations usually occur randomly rather than being passed down from parents.
Tip: Always consult your doctor for personalized advice and treatment plans tailored to your condition.


