How AI Algorithms Are Revolutionizing Cancer Detection
AI algorithms are changing how you detect cancer by making the process faster and more accurate. These tools analyze medical images, such as mammograms and CT scans, with precision that often surpasses human capabilities. For example:
AI software has increased cancer detection rates in general practices from 58.7% to 66%.
It improves accuracy in mammography and lung cancer detection, enabling earlier diagnoses.
AI systems also reduce misdiagnoses by balancing sensitivity and specificity. They identify small abnormalities in scans, helping doctors catch cancer at its earliest stages.
How AI Algorithms Identify Cancerous Cells Faster and More Accurately is a critical step toward saving lives and improving healthcare outcomes.
Key Takeaways
AI tools help find cancer better, raising accuracy from 58.7% to 66%. This helps doctors find cancer sooner and treat it faster.
Machine learning and deep learning spot cancer cells in images. This helps doctors notice problems they might not see on their own.
AI reduces mistakes in medical images by double-checking them. It works like an extra pair of eyes to catch missed problems.
AI brings healthcare to areas with fewer doctors. It gives people in these places better tools to detect cancer.
Doctors and AI work together to find cancer more accurately. This teamwork makes finding cancer quicker and more trustworthy.
How AI Algorithms Identify Cancerous Cells Faster and More Accurately
Machine Learning and Deep Learning in Cancer Detection
Neural networks for image analysis
Neural networks play a vital role in analyzing medical images. These AI models mimic the human brain's structure to identify patterns in X-rays, MRIs, and CT scans. For example, deep learning algorithms can detect subtle abnormalities in mammograms that might go unnoticed by the human eye. A study comparing AI and traditional methods found that computer-assisted detection (CAD) systems significantly improved diagnostic accuracy. These tools act as reliable assistants, especially for less experienced professionals.
Training algorithms with diverse datasets
AI algorithms rely on diverse datasets to improve their accuracy. By training on a wide range of medical images and patient demographics, these models learn to recognize cancerous cells across different populations. This reduces the risk of bias and ensures fairer outcomes. For instance, machine learning models trained on global datasets have achieved an AUC (Area Under the Curve) score of 0.86, outperforming some deep learning models. This highlights the importance of robust training data in enhancing AI's performance.
Key Technologies Driving AI in Oncology
Computer vision for medical imaging
Computer vision enables AI to analyze medical images with remarkable precision. It extracts critical features from scans, such as tumor size and shape, to assist in diagnosis. Radiomics, a subset of computer vision, goes a step further by quantifying these features to predict tumor behavior. This technology has reshaped cancer management by integrating large datasets and high-performance computing, leading to better treatment decisions.
Radiomic analysis for tumor characterization
Radiomic analysis uses advanced algorithms to extract data from medical images. This approach helps you understand tumor characteristics, such as texture and density, which are crucial for diagnosis and treatment planning. Radiomics also aids in predicting tumor burden and guiding therapy decisions, making it an indispensable tool in oncology.
Data Sources Powering AI Models
Medical imaging data (e.g., X-rays, MRIs, CT scans)
Medical imaging data forms the backbone of AI in cancer detection. AI models analyze thousands of images to identify patterns linked to cancer. For example, radiomics extracts features from CT scans to diagnose lung cancer early. These insights help doctors make informed decisions, improving patient outcomes.
Genomic and molecular data integration
Integrating genomic and molecular data with imaging data enhances AI's diagnostic capabilities. This multi-omics approach allows AI to analyze genetic mutations and molecular markers alongside medical images. By combining these data sources, AI can provide a comprehensive view of a patient's condition, paving the way for personalized treatment plans.
Real-World Applications of AI in Cancer Detection
AI in Breast Cancer Screening
Enhancing mammography accuracy
AI has significantly improved the accuracy of mammography, helping you detect breast cancer earlier. Tools like MammoScreen analyze breast regions to highlight areas that need further examination. This reduces the chances of missing abnormalities. Similarly, MammoRisk evaluates factors such as age and family history to assess your risk of developing invasive breast cancer. These tools provide tailored reports, enabling doctors to make informed decisions.
One study demonstrated the effectiveness of AI in breast cancer detection using ultrasound images. Researchers trained an advanced AI system on over 5 million images from nearly 300,000 exams. When compared to ten board-certified radiologists, the AI system showed remarkable accuracy. By combining AI predictions with radiologist assessments, this hybrid model improved diagnostic precision.
Case studies of AI-assisted breast cancer diagnoses
AI tools like Mammography Intelligent Assessment (MIA) have transformed breast cancer screening. MIA detects signs of cancer that radiologists might miss, increasing cancer identification rates by 12%. It also reduces the workload of healthcare professionals by 30%. Additionally, AI-assisted mammography screening has been shown to enhance cancer detection rates while maintaining or lowering recall rates.
Group | Cancer Detection Rate (CDR) | Recall Rate (RR) | |
|---|---|---|---|
With AI | 140 (0.57%) | 5.70‰ | N/A |
Without AI | 123 (0.57%) | 5.01‰ | N/A |
p-value | N/A | <0.001 | 0.564 |
AI in Lung Cancer Detection
Early detection through CT scan analysis
AI excels in analyzing CT scans to identify early signs of lung cancer. Tools like Sybil predict your lung cancer risk based on a single low-dose CT (LDCT) scan. This approach enables earlier diagnosis and treatment, which is crucial for improving survival rates. AI also enhances sensitivity in detecting lung nodules, making it an invaluable tool in lung cancer screening.
Reducing false positives in lung cancer screening
False positives can lead to unnecessary stress and procedures. AI minimizes this issue by accurately classifying nodules and predicting their growth. For instance, AI systems have shown potential in reducing false-positive rates while maintaining high sensitivity. This ensures that you receive precise and reliable results during screenings.
Aspect | Findings |
|---|---|
Nodule Detection Sensitivity | AI significantly improves sensitivity in detecting nodules. |
False-Positive Rates | AI reduces the rates of false positives in lung cancer screening. |
Nodule Classification | AI aids in the classification of nodules, crucial for diagnosis. |
Prognosis | AI shows potential in predicting nodule growth and genetic typing. |
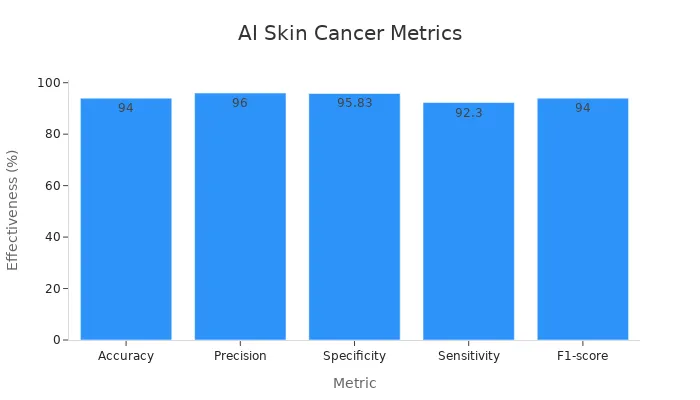
AI in Skin Cancer Detection
Identifying melanoma through image recognition
AI-powered image recognition systems have revolutionized skin cancer detection. These systems analyze images of skin lesions to identify melanoma with high accuracy. Studies show that AI achieves a diagnostic accuracy of 94%, outperforming many dermatologists.
Metric | Value |
|---|---|
Accuracy | 94% |
Precision | 96% |
Specificity | 95.83% |
Sensitivity | 92.30% |
F1-score | 0.94 |
Smartphone apps for skin cancer screening
AI has made skin cancer screening more accessible through smartphone apps. These apps allow you to take pictures of suspicious moles and receive instant feedback. While not a replacement for professional diagnosis, they serve as a convenient first step in identifying potential issues.
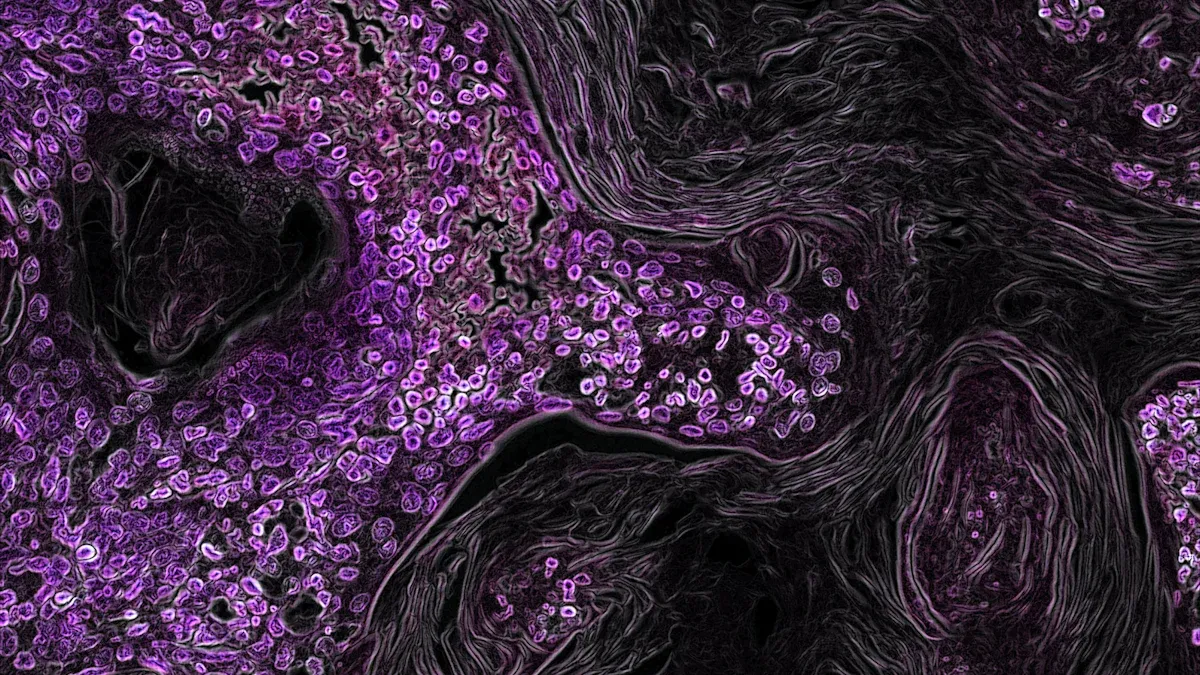
AI in Pathology and Tissue Analysis
Automating tissue sample analysis
AI has transformed how you analyze tissue samples in pathology. Traditional methods often require hours of manual examination under a microscope. AI-powered tools now automate this process, saving time and reducing the risk of human error. These systems use advanced algorithms to scan and interpret digital slides with remarkable precision. For example, AI can identify cancerous cells in tissue samples by detecting subtle patterns that might escape the human eye.
One of the most significant advantages of automation is its ability to handle large volumes of data. AI systems can process thousands of slides in a fraction of the time it would take a pathologist. This efficiency ensures that you receive faster results, which is critical for timely treatment. Additionally, AI tools can highlight areas of concern on a slide, guiding pathologists to focus on the most relevant regions. This collaboration between AI and human expertise enhances the overall diagnostic process.
Improving diagnostic consistency
AI plays a crucial role in improving diagnostic consistency in pathology. Variations in slide preparation and imaging can sometimes lead to inconsistent results. AI algorithms address this challenge by analyzing complex imaging data with a level of detail that exceeds human capabilities. These tools recognize intricate patterns in tissue samples, providing insights that enhance diagnostic accuracy.
External validation is essential for ensuring AI tools perform reliably across different clinical settings. Well-constructed test datasets that reflect real-world diversity help assess the accuracy and generalizability of these algorithms. Without proper validation, AI tools may struggle to deliver consistent results. By standardizing the diagnostic process, AI ensures that you receive accurate and reliable diagnoses, regardless of where you seek care.
AI in pathology not only improves efficiency but also ensures that every patient benefits from the same high standard of care.
Benefits of AI in Cancer Detection
Enhanced Diagnostic Precision
Reducing human error in medical imaging
AI significantly reduces human error in medical imaging by acting as a second set of eyes. Tools like Mammography Intelligent Assessment (MIA) have helped doctors identify 12% more cancers while reducing radiologists' workload by 30%. These systems analyze medical images with remarkable accuracy, ensuring fewer missed diagnoses. By minimizing variability in interpretations, AI ensures consistent and reliable results across different healthcare settings.
Identifying subtle patterns in data
AI excels at identifying subtle patterns in medical data that might go unnoticed by the human eye. For instance, AI tools classify tumor types and predict their behavior by analyzing intricate patterns in imaging and genomic data. This capability enhances precision medicine, allowing doctors to tailor treatments based on genetic variations. AI also tracks genetic changes over time, enabling dynamic adjustments to treatment plans and improving recovery rates.
Faster and Earlier Detection
Detecting cancer at earlier stages
AI accelerates cancer detection by analyzing vast amounts of data in a fraction of the time it takes traditional methods. From August 2021 to July 2022, FDA-approved AI tools like Lunit INSIGHT MMG demonstrated high accuracy in identifying breast cancer. These tools increased sensitivity by 12 percentage points for cancers with mass and 40 percentage points for asymmetrical or distorted cancers. Early detection improves treatment outcomes and saves lives.
Increasing survival rates through timely intervention
AI-driven technologies enable timely interventions by detecting cancer at its earliest stages. A study analyzing 382 records found that AI approaches significantly improved diagnostic accuracy compared to traditional methods. Early diagnosis allows doctors to recommend therapies faster, increasing survival rates. For example, AI-assisted workflows at NYU Langone Health reduced false positives and improved sensitivity, leading to earlier diagnoses and better patient outcomes.
Expanding Access to Healthcare
Providing diagnostic tools in underserved areas
AI expands access to healthcare by bringing diagnostic tools to underserved regions. Mobile health applications powered by AI allow you to screen for cancer without traveling long distances. Telemedicine platforms enhanced by AI provide expert diagnostic support remotely, ensuring that even rural communities receive quality care.
Reducing disparities in cancer care
AI helps reduce disparities in cancer care by identifying and addressing gaps in healthcare access. Predictive analytics forecast healthcare needs in underserved populations, enabling targeted interventions. AI also supports personalized medicine, tailoring treatments to individual patients, which is especially beneficial in low-resource settings.
With AI, you gain access to advanced diagnostic tools, regardless of location, ensuring equitable healthcare for all.
Challenges and Ethical Considerations
Data Privacy and Security
Protecting patient information in AI systems
AI systems rely on vast amounts of sensitive medical data, including imaging and genetic information. Protecting this data is essential to maintain your privacy and trust. Robust encryption methods and secure storage protocols help safeguard patient information from unauthorized access. For example, genetic data used in cancer risk prediction must be handled carefully to prevent misuse, such as genetic discrimination. Without strong security measures, patients could face challenges like denial of insurance or employment opportunities.
Ensuring informed consent is another critical step. You should have a clear understanding of how your data will be used and stored. Transparent communication builds trust and promotes ethical AI practices.
Addressing concerns about data breaches
Data breaches pose a significant threat to healthcare systems. Hackers targeting AI databases could expose sensitive patient information, leading to severe consequences. To address this, healthcare providers must implement advanced cybersecurity measures. Regular audits and compliance with data protection regulations, such as HIPAA, ensure that your information remains secure. By prioritizing these safeguards, AI systems can operate ethically and responsibly.
Algorithm Bias and Fairness
Ensuring diverse and representative training data
AI algorithms must be trained on diverse datasets to avoid bias. If training data disproportionately represents certain populations, the AI may fail to provide accurate diagnoses for others. For instance, many existing models are trained primarily on data from white patients, which can lead to disparities in care for underrepresented groups. Using inclusive datasets ensures that AI tools work effectively for everyone, regardless of race or ethnicity.
Diverse datasets reduce healthcare disparities.
Fairness-aware machine learning identifies and corrects biases.
Transparency in AI decision-making promotes accountability.
Avoiding disparities in AI-driven diagnoses
Bias in AI systems can worsen existing healthcare inequalities. Diseases often present differently across populations, and algorithms trained on limited data may overlook these variations. Involving ethicists and representatives from marginalized communities during AI development helps address these issues. Transparent and interpretable AI systems also allow you to understand how decisions are made, ensuring fairness in diagnoses.
Integration into Clinical Practice
Overcoming resistance from healthcare professionals
Introducing AI into clinical settings often meets resistance from healthcare professionals. You may wonder if AI will replace human expertise. However, AI is designed to assist, not replace, doctors. Training programs that teach clinicians how to use AI tools effectively can ease this transition. A multidisciplinary approach, involving both medical and technical experts, ensures that AI integrates smoothly into workflows.
Ensuring regulatory compliance
Regulatory compliance is crucial for the safe use of AI in healthcare. AI-based medical devices must meet strict standards to ensure reliability. Testing these tools on local datasets improves their accuracy in specific contexts. Policymakers play a vital role in establishing ethical guidelines and addressing concerns like data privacy and algorithmic transparency. By adhering to these regulations, AI can provide equitable and effective cancer care.
Successful integration of AI into clinical practice requires collaboration, transparency, and a commitment to ethical standards.
The Future of AI in Oncology
Advancements in AI Technology
Predictive analytics for personalized treatment
AI is transforming cancer care by enabling predictive analytics for personalized treatment. These systems analyze your genetic, environmental, and lifestyle factors to tailor treatment plans. For example:
AI predicts how tumors will respond to specific therapies, helping doctors choose the most effective options.
It mines genomic data to uncover deep-level insights, ensuring treatments align with your unique biology.
Multi-omics data integration enhances cancer detection, screening, and classification, paving the way for precision medicine.
By leveraging these capabilities, AI ensures you receive care that is both effective and customized to your needs. This approach not only improves outcomes but also minimizes unnecessary treatments.
Integration of AI with wearable health devices
Wearable health devices are becoming a vital part of cancer care. AI integrates with these devices to monitor your health in real time. For instance, smartwatches equipped with AI algorithms can track vital signs and detect anomalies that may indicate early cancer symptoms. These devices provide continuous data, allowing doctors to intervene promptly when needed.
AI-powered wearables also empower you to take charge of your health. By offering insights into your daily habits and their impact on your well-being, these tools encourage proactive healthcare management. This integration represents a significant step toward more accessible and personalized cancer care.
Collaboration Between AI and Healthcare Professionals
Augmenting, not replacing, human expertise
AI enhances, rather than replaces, the expertise of healthcare professionals. It acts as a reliable assistant, analyzing vast amounts of data to identify patterns that might escape the human eye. For example, AI tools in radiology and pathology already support over 80% of approved AI devices in cancer diagnostics. These systems streamline workflows, allowing doctors to focus on complex decision-making and patient care.
By combining AI's analytical power with your doctor’s clinical judgment, you benefit from a more accurate and comprehensive diagnosis. This collaboration ensures that technology complements, rather than competes with, human expertise.
Training clinicians to work with AI tools
To maximize AI's potential, healthcare professionals need proper training. Learning to interpret AI-generated insights and integrate them into clinical practice is essential. Training programs help doctors understand how to use these tools effectively, ensuring seamless adoption.
When clinicians and AI work together, the result is a more efficient and patient-centered healthcare system. This partnership not only improves diagnostic accuracy but also builds trust in AI-driven solutions.
Expanding Global Impact
Scaling AI solutions for global cancer care
AI has the potential to revolutionize cancer care worldwide. For example:
AI models for breast cancer screening have outperformed radiologists in detecting cancer from mammograms.
Tools like the Artemisia model demonstrate professional-level performance in breast density categorization, even in resource-limited settings.
AI optimizes resource allocation, extending healthcare reach to underserved areas.
By scaling these solutions, you can access advanced diagnostic tools regardless of your location. This inclusivity ensures that everyone benefits from cutting-edge cancer care.
Bridging gaps in healthcare infrastructure
AI addresses disparities in healthcare by bridging gaps in infrastructure. It enhances diagnostic accuracy, which is crucial for early cancer detection. Additionally, AI ensures efficient use of resources, making healthcare more accessible in underserved regions.
By overcoming barriers caused by socioeconomic and geographical factors, AI creates a more equitable healthcare system. This technology empowers you to receive timely and accurate diagnoses, no matter where you live.
The future of AI in oncology holds immense promise. With advancements in technology and global collaboration, AI is set to transform cancer care for the better.
AI algorithms are transforming cancer detection by improving speed, accuracy, and accessibility. These tools detect malignant tumors with precision, often outperforming traditional methods. Technologies like CAD systems and machine learning provide reliable support, especially for less experienced professionals. You benefit from earlier diagnoses and better outcomes, which increase survival rates.
While challenges like data privacy and algorithm bias remain, advancements in AI and collaboration with healthcare professionals will unlock its full potential. The future of AI in oncology holds immense promise, offering hope for equitable and effective cancer care worldwide.
FAQ
What types of cancer can AI help detect?
AI can assist in detecting various cancers, including breast, lung, skin, and colorectal cancers. It analyzes medical images, genomic data, and other diagnostic inputs to identify abnormalities. These tools improve early detection and diagnostic accuracy, offering you better chances for successful treatment.
How accurate are AI algorithms in cancer detection?
AI algorithms often achieve accuracy rates exceeding 90% in specific applications, such as skin cancer detection or mammography analysis. These systems identify subtle patterns that human eyes might miss, ensuring reliable results. However, their performance depends on the quality of training data and clinical validation.
Can AI replace doctors in cancer diagnosis?
No, AI complements doctors rather than replacing them. It acts as a decision-support tool, analyzing data and providing insights. Your doctor uses these insights to make informed decisions. This collaboration ensures accurate diagnoses while maintaining the human touch in patient care.
Are AI-based cancer detection tools available worldwide?
AI tools are expanding globally but remain limited in some regions due to infrastructure challenges. Mobile apps and telemedicine platforms powered by AI aim to bridge this gap. These innovations bring advanced diagnostic capabilities to underserved areas, improving access to cancer care.
Is my data safe when using AI in cancer detection?
AI systems prioritize data security through encryption and compliance with regulations like HIPAA. Your data remains protected during analysis and storage. Always choose healthcare providers that follow strict privacy protocols to ensure your information stays confidential and secure.
See Also
How AI is Transforming Cancer Diagnosis and Treatment in 2025
Recognizing Symptoms and Treatments for Duodenal Cancer
Exploring Large-Cell Lung Carcinoma and Its Categories
Identifying Symptoms and Treatment Options for Conjunctival Melanoma

