Do All Cancer Treatments Lead to Nausea and Vomiting

You may wonder if all cancer treatments cause nausea and vomiting? The answer is no. While some treatments, like chemotherapy and radiation therapy, are more likely to trigger these side effects, others may not. For example, anticipatory nausea affects about 29% of patients undergoing chemotherapy, and anticipatory vomiting occurs in 11%. A clinical study also revealed that delayed vomiting happens in 33% of patients treated with drugs like cisplatin or carboplatin, but only 11% of those receiving other medications. Interestingly, on 79% of study days, patients did not take antiemetics, yet 93% of those days were free from vomiting. These statistics highlight how treatment type and individual responses play a significant role in whether all cancer treatments cause nausea and vomiting.
Key Takeaways
Cancer treatments don’t always cause nausea or vomiting. Knowing the treatment type helps you prepare better.
Medicines for nausea can lower sickness during chemotherapy. Talk to your doctor about ways to prevent it.
Things like age, gender, and stress can affect nausea risk. Adjusting treatment for these can make it work better.
Eating small meals and avoiding strong smells can reduce nausea. Changing your diet can really help.
Drinking water and getting enough sleep can ease nausea. Staying healthy supports recovery during treatment.
Do All Cancer Treatments Cause Nausea and Vomiting?
Treatments Less Likely to Cause Nausea
Not all cancer treatments cause nausea and vomiting. Some therapies are less likely to trigger these side effects, especially when paired with effective preventive measures. For example, antiemetic medications like 5-HT3 receptor antagonists (ondansetron, granisetron, palonosetron) and NK-1 receptor antagonists (aprepitant) have shown success in reducing chemotherapy-induced nausea. These drugs block specific neuroreceptors responsible for triggering nausea.
Clinical studies also highlight the importance of tailoring antiemetic therapy to the emetogenic potential of the treatment. For instance:
Ondansetron and similar drugs are highly effective in preventing nausea.
Guidelines recommend pre-treatment management to minimize symptoms.
By using these strategies, many patients experience fewer or no symptoms, even during intensive treatments.
Treatments More Likely to Cause Nausea
Certain cancer treatments carry a higher risk of nausea and vomiting. Chemotherapy, especially with high-risk drugs like cisplatin, is a common culprit. Radiation therapy targeting the abdomen or brain also increases the likelihood of these side effects. Combination therapies, such as chemotherapy paired with radiation, further elevate the risk.
A comparative study illustrates the prevalence of nausea and vomiting across different treatments:
Study Context | Prevalence of ANV | Prevalence of Anticipatory Vomiting |
|---|---|---|
Adults with 5-HT3 receptor antagonists and corticosteroids | ~33% | 6% to 11% |
Children pre-5-HT3 receptor antagonist era | 29% | 20% |
Children post-5-HT3 receptor antagonist era | 0% to 59% | N/A |
Children (one study) | 26% | 26% |
These statistics show that while some treatments are more likely to cause nausea, advancements in medication have significantly reduced the prevalence.
Variability Among Patients
Your experience with nausea and vomiting depends on several factors. Age, gender, and medical history play a role. For example, younger patients and women are more likely to experience these symptoms. Anxiety and a history of motion sickness can also increase your risk.
Factor | Description |
|---|---|
Age | Younger than 50 years is a risk factor for ANV. |
Gender | Female gender is associated with a higher incidence of ANV. |
Previous N&V | N&V after the last chemotherapy session increases risk. |
Severity of Symptoms | Moderate to severe posttreatment nausea or vomiting correlates with higher risk. |
Anxiety | High-state anxiety reactive to specific situations is a risk factor. |
Motion Sickness | Susceptibility to motion sickness is linked to ANV. |
Understanding these factors can help you and your healthcare provider develop a personalized plan to manage symptoms effectively.
Factors Influencing Nausea and Vomiting
Type of Cancer Treatment
Chemotherapy
Chemotherapy is one of the most common cancer treatments associated with nausea and vomiting. The likelihood depends on the specific drugs used. For instance, high-risk drugs like cisplatin can cause nausea in up to 90% of patients. Moderate-risk drugs have a lower incidence but still pose a significant challenge.
Type of Treatment | Incidence of Nausea (%) | Incidence of Vomiting (%) |
|---|---|---|
Chemotherapy (ANV) | 29 | 11 |
Moderate/High-risk Chemo | 30-90 | N/A |
Radiation Therapy
Radiation therapy can also lead to nausea, especially when targeting sensitive areas like the abdomen or pelvis. Radiation-induced nausea and vomiting (RINV) occurs in about 80% of patients receiving treatment to the lower abdomen.
Immunotherapy and Targeted Therapy
Immunotherapy and targeted therapies generally have a lower risk of nausea compared to chemotherapy. However, some patients may still experience mild symptoms depending on the specific drug and dosage.
Surgery
Surgical procedures, particularly those requiring anesthesia, can trigger postoperative nausea and vomiting (PONV). Factors like the duration of anesthesia and the use of opioids for pain management increase this risk.
Dosage and Treatment Schedule
The dosage and schedule of your treatment significantly influence the likelihood of nausea. Higher doses of chemotherapy or radiation increase the risk. Clinical trials show that antiemetic drugs like ondansetron and aprepitant can reduce nausea when administered before treatment.
Treatment | Dosage | Schedule | Control Rate |
|---|---|---|---|
Ondansetron | 8 mg | Regardless | 40% vs. 57% |
Aprepitant | 125 mg before chemo | 5-7 days | 57.9%-72.5% |
Individual Patient Factors
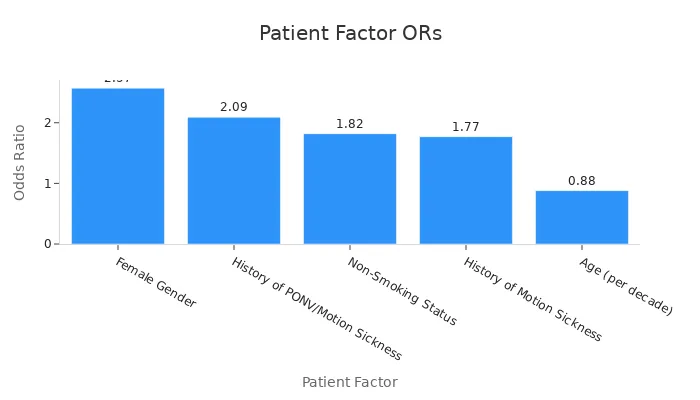
Age and Gender
Younger patients, especially those under 50, are more prone to nausea. Women are also at a higher risk, with studies showing an odds ratio (OR) of 2.57 for female patients.
Medical History and Pre-existing Conditions
A history of motion sickness or prior nausea during treatment increases your risk. Non-smokers and those with fluid imbalances or certain medications are also more susceptible.
Psychological Factors (e.g., anxiety)
Anxiety can amplify nausea. High levels of stress or anticipation before treatment often worsen symptoms.
Understanding these factors can help you and your healthcare provider create a personalized plan to manage symptoms effectively.
Cancer Treatments with Higher Risk

Chemotherapy Drugs
High-risk drugs (e.g., cisplatin, cyclophosphamide)
Some chemotherapy drugs are more likely to cause nausea and vomiting. High-risk drugs, such as cisplatin, cyclophosphamide, doxorubicin, and ifosfamide, have been documented to induce emesis in over 90% of patients. These medications are often used to treat aggressive cancers, but their emetogenic potential makes them challenging for patients.
To manage these side effects, your healthcare provider may prescribe antiemetic medications before and after treatment. This approach can significantly reduce the severity of symptoms, allowing you to better tolerate the therapy.
Moderate-risk drugs
Moderate-risk chemotherapy drugs, including carboplatin and oxaliplatin, cause nausea and vomiting in 30% to 90% of patients. While the risk is lower than with high-risk drugs, it still requires careful management. Preventive strategies, such as pre-treatment antiemetics and hydration, can help minimize discomfort.
Risk Category | Description |
|---|---|
High Risk | Emesis has been documented in >90% of patients. |
Moderate Risk | Emesis has been documented in 30%–90% of patients. |
Low Risk | Emesis has been documented in 10%–30% of patients. |
Minimal Risk | Emesis has been documented in <10% of patients. |
Radiation Therapy
Areas of the body treated (e.g., abdomen, brain)
Radiation therapy can also lead to nausea and vomiting, especially when targeting sensitive areas like the abdomen, liver, or brain. For example, radiation to the upper abdomen causes nausea in up to 80% of patients. Total body irradiation carries the highest risk, with nearly all patients experiencing some degree of nausea.
Evidence Description | Impact on Nausea | Body Region |
|---|---|---|
Radiation therapy is a significant cause of nausea and vomiting in cancer patients. | 80% of patients experience some degree of nausea and vomiting. | Various regions, particularly upper abdomen and total body. |
Radiation induces nausea and vomiting in 50% to 80% of patients. | Severity varies with treatment area. | Upper abdomen has high risk; total body radiation has the highest likelihood. |
Nausea and vomiting are more common with radiation to the abdomen, liver, or brain. | Increased risk with total body irradiation. | Specific body regions are more affected. |
If you are undergoing radiation therapy, your care team may recommend anti-nausea medications or dietary adjustments to help manage these symptoms.
Combination Therapies
Chemotherapy and radiation together
When chemotherapy and radiation are combined, the risk of nausea and vomiting increases significantly. This is because the emetogenic potential of both treatments adds up, creating a cumulative effect. For example:
Moderate- or high-risk chemotherapy drugs can cause nausea in 30% to 90% of patients.
Combining these drugs with radiation therapy further elevates the risk.
Factors such as the dose, treatment schedule, and specific drugs used also influence the severity of symptoms. High doses of drugs with low emetogenic potential can still lead to significant nausea when combined with radiation. Your healthcare provider will carefully consider these factors to create a treatment plan that minimizes side effects.
While not all cancer treatments cause nausea and vomiting, combination therapies often carry a higher risk. Understanding these risks can help you prepare and manage symptoms effectively.
Other Factors
Use of anesthesia during surgery
Anesthesia plays a critical role in making surgeries pain-free, but it can also increase the risk of nausea and vomiting afterward. Postoperative nausea and vomiting (PONV) often occur due to the type of anesthesia used, the duration of the procedure, and the medications given for pain relief. If you undergo surgery as part of your cancer treatment, understanding these factors can help you prepare for potential side effects.
Volatile anesthetics, commonly used during surgeries, are a significant contributor to PONV. Studies show that these anesthetics increase the odds of nausea by 82%. Nitrous oxide, another anesthetic option, raises the risk by 45%. The longer the anesthesia lasts, the higher the likelihood of experiencing nausea. For every additional hour of anesthesia, the odds increase by 46%. Postoperative opioid use for pain management further adds to the risk, with a 39% increase in nausea likelihood.
Factor | Odds Ratio (OR) | 95% Confidence Interval |
|---|---|---|
Use of volatile anesthetics | 1.82 | 1.56 - 2.13 |
Duration of anesthesia | 1.46 h(-1) | 1.30 - 1.63 |
Postoperative opioid use | 1.39 | 1.20 - 1.60 |
Nitrous oxide | 1.45 | 1.06 - 1.98 |
Your healthcare team can take steps to reduce these risks. They may use alternative anesthetics or limit the use of opioids after surgery. Preventive medications, such as antiemetics, can also help manage nausea. By discussing these options with your doctor, you can create a plan to minimize discomfort and recover more comfortably after surgery.
Tip: Let your care team know if you have experienced nausea after previous surgeries. This information can guide them in tailoring your anesthesia plan.
Prevention and Management Strategies

Medications for Nausea and Vomiting
Antiemetics (e.g., ondansetron, dexamethasone)
Medications called antiemetics can effectively prevent and manage nausea and vomiting during cancer treatments. Drugs like ondansetron, granisetron, and dexamethasone work by blocking the brain's nausea signals. Clinical trials have shown their effectiveness in reducing symptoms, especially for chemotherapy-induced nausea.
Study Description | Findings |
|---|---|
Aprepitant, granisetron, and dexamethasone for prevention of chemotherapy-induced nausea and vomiting after high-dose melphalan in autologous transplantation for multiple myeloma | |
Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting | A randomized phase III trial showing olanzapine's effectiveness in controlling both nausea and vomiting. |
Your healthcare provider may prescribe these medications before or after treatment to minimize discomfort. Following their recommendations can help you feel more in control of your symptoms.
Preventive medications before treatment
Taking preventive medications before starting treatment can significantly reduce the risk of nausea. Drugs like aprepitant are often given before chemotherapy to block nausea triggers. This proactive approach ensures that you experience fewer side effects, allowing you to focus on recovery.
Dietary and Lifestyle Adjustments
Eating small, frequent meals
Adjusting your eating habits can make a big difference. Eating small, frequent meals helps reduce the strain on your stomach, making it easier to manage nausea. Staying hydrated is equally important, as dehydration can worsen symptoms.
Choose bland, easy-to-digest foods like crackers or toast.
Avoid skipping meals, as an empty stomach can trigger nausea.
Avoiding strong smells and greasy foods
Certain smells and foods can make nausea worse. Strong odors, greasy meals, or spicy dishes often act as triggers. Identifying and avoiding these can help you feel more comfortable. Consulting a dietitian can also provide personalized advice to meet your nutritional needs during treatment.
Complementary Therapies
Acupuncture
Acupuncture is a complementary therapy that some patients find helpful for managing nausea. While studies suggest it may reduce symptoms, the evidence is not strong enough to make a definitive recommendation. If you choose acupuncture, ensure you visit a qualified practitioner to minimize risks.
Relaxation techniques (e.g., meditation, deep breathing)
Relaxation techniques like meditation and deep breathing can help you manage nausea by reducing stress and anxiety. These methods are non-invasive and easy to practice at home. Incorporating them into your daily routine can improve your overall well-being during treatment.
Tip: Combining dietary changes, medications, and complementary therapies can provide a comprehensive approach to managing nausea. Always discuss these options with your healthcare provider to find what works best for you.
Staying Hydrated and Rested
Staying hydrated and getting enough rest play a vital role in managing nausea during cancer treatment. When your body lacks water, it can slow down bowel movements, leading to discomfort and nausea. Vomiting or diarrhea caused by treatment can also dehydrate you, making it harder to recover and leaving you feeling drained. Drinking enough fluids helps prevent these issues and keeps your energy levels stable.
Evidence | Description |
|---|---|
Staying Hydrated | Staying adequately hydrated is essential to prevent nausea during cancer treatment. |
Dehydration Effects | Lack of water can slow down bowel movements, leading to nausea and discomfort. |
To maintain hydration, choose fluids that are gentle on your stomach. Water is the best option, but you can also drink decaffeinated tea, juices, or milk. Avoid caffeinated or sugary drinks, as they may worsen dehydration. Sipping fluids throughout the day, rather than drinking large amounts at once, can make it easier for your body to absorb them.
Evidence | Description |
|---|---|
Hydration Importance | Diarrhea and vomiting can lead to dehydration, which depletes energy and can cause nausea. |
Recommended Fluids | Drinking water, decaffeinated tea, juices, and milk is advised to maintain hydration. |
Rest is equally important for managing nausea and fatigue. Cancer treatments often leave you feeling tired, and adequate sleep helps your body recover. Practicing good sleep hygiene, such as maintaining a consistent bedtime and creating a relaxing sleep environment, can improve the quality of your rest. Discussing your sleep patterns with your healthcare provider can also help address any issues.
Evidence | Description |
|---|---|
Importance of Rest | Adequate rest and sleep are crucial for managing fatigue, a common side effect of cancer treatment. |
Sleep Hygiene | Discussing sleep patterns and encouraging good sleep hygiene can help improve rest. |
By staying hydrated and well-rested, you can better manage the side effects of your treatment and support your overall recovery. These simple steps can make a big difference in how you feel each day.
When to Contact Your Healthcare Provider
Persistent or Severe Symptoms
Vomiting that lasts more than 24 hours
You should contact your healthcare provider if vomiting persists for more than 24 hours. Prolonged vomiting can lead to dehydration and other complications. It may also indicate that your treatment plan needs adjustment. Persistent symptoms often require medical intervention to prevent further health issues.
Inability to keep food or liquids down
If you cannot keep food or liquids down, it’s essential to seek medical advice. This condition can quickly lead to dehydration and malnutrition, both of which can weaken your body. Your doctor may recommend intravenous fluids or medications to help manage these symptoms.
Recommendation | Description |
|---|---|
If nausea does not improve over a few days | |
Intermittent nausea | If nausea occurs intermittently |
Severe symptoms | If nausea is severe and may indicate a heart attack |
Ongoing nausea and vomiting | Contact your doctor if nausea and vomiting persist |
Worsening vomiting | If vomiting is getting worse |
Duration of vomiting | If vomiting lasts longer than 2 days |
Signs of Dehydration
Dizziness, dry mouth, or dark urine
Dehydration can occur when your body loses more fluids than it takes in. Symptoms like dizziness, dry mouth, or dark urine signal that your body needs immediate hydration. If these signs persist, you should consult your healthcare provider. Severe dehydration can lead to complications, including kidney problems and electrolyte imbalances.
Concerns About Medications
Ineffectiveness of prescribed anti-nausea drugs
If your prescribed anti-nausea medications are not working, let your doctor know. Many patients still experience nausea and vomiting despite taking these drugs. Adjusting your medication or dosage may improve your symptoms.
Side effects from anti-nausea medications
Anti-nausea medications can sometimes cause side effects. Common issues include headache, constipation, and fatigue. Less frequent side effects, such as dry mouth or changes in liver function, may also occur. Rarely, medications like ondansetron can lead to QTc prolongation or extrapyramidal symptoms (EPS). If you experience any of these, inform your healthcare provider immediately.
Side Effect | Description |
|---|---|
Headache | Can be treated with mild analgesics. |
Constipation | Commonly reported side effect. |
Fatigue | Patients may experience increased tiredness. |
Dry Mouth | A frequent complaint among users. |
Liver Function | Transient elevations in liver function tests may occur. |
Thrombocytopenia | Rarely implicated in case studies. |
QTc Prolongation | Rare electrocardiogram changes may occur. |
EPS | Possible but unclear association with ondansetron. |
Many patients still experience N&V despite prophylaxis. |
Tip: Keep track of your symptoms and side effects. Sharing this information with your doctor can help them tailor your treatment plan effectively.
Not all cancer treatments cause nausea and vomiting. Some therapies, like low-emetogenic agents, rarely require preventive measures. Clinical studies show that 73% of pediatric patients receiving highly emetogenic chemotherapy achieved complete vomiting control with olanzapine, compared to 48% with a placebo. Children also experience fewer delayed symptoms than adults, highlighting variability in treatment effects.
Study Focus | Findings |
|---|---|
Pediatric patients receiving highly emetogenic chemotherapy | 73% in olanzapine group had complete control of vomiting in delayed phase vs. 48% in placebo group (P = .005) |
Children receiving low emetogenicity agents | Routine prophylaxis not required during delayed phase |
Comparison of delayed N&V prevalence | Delayed N&V may be less prevalent in children than adults, indicating lower emetogenic potential in many regimens. |
Effective strategies, including medications and lifestyle changes, can help manage symptoms. Always consult your healthcare provider if symptoms persist or worsen.
FAQ
What should you do if nausea persists despite taking medications?
You should contact your healthcare provider immediately. Persistent nausea may indicate that your treatment plan needs adjustment. Your doctor might prescribe alternative antiemetics or suggest additional strategies to manage symptoms effectively.
Can you prevent nausea before starting cancer treatment?
Yes, preventive medications like antiemetics can reduce nausea risks. Your doctor may recommend taking these drugs before treatment begins. This proactive approach helps block nausea triggers and improves your overall comfort during therapy.
Are natural remedies like ginger effective for nausea?
Ginger may help reduce mild nausea for some people. You can try ginger tea, candies, or supplements. However, always consult your doctor before using natural remedies to ensure they won’t interfere with your treatment.
Does everyone experience nausea during chemotherapy?
No, not everyone experiences nausea during chemotherapy. The likelihood depends on the specific drugs, dosage, and your individual risk factors. Preventive measures, such as antiemetics, can significantly reduce the chances of nausea.
How can you manage nausea at home?
You can eat small, bland meals, stay hydrated, and avoid strong smells. Relaxation techniques like deep breathing or meditation may also help. Always follow your doctor’s advice for managing symptoms effectively.
Tip: Keep a symptom diary to track what triggers your nausea. Share this with your healthcare provider for personalized guidance.
See Also
Identifying Symptoms and Causes of Head and Neck Cancer
Exploring Symptoms and Treatment Options for Duodenal Cancer
An In-Depth Overview of Various Types of Cancer

