What is Anaplastic Large Cell Lymphoma and How is it Treated

Anaplastic large cell lymphoma is a rare and aggressive form of non-Hodgkin lymphoma. It accounts for only 1% to 2% of all lymphoma cases. This disease primarily affects T-cells, which are crucial for your immune system. Its symptoms can progress quickly, making early diagnosis essential. Fortunately, modern treatments have improved outcomes significantly. For example, patients with ALK-positive ALCL have a five-year survival rate of up to 80%. Even ALK-negative cases, though more challenging, show improved survival rates with advanced therapies. These advancements offer hope and better quality of life for many individuals.
Key Takeaways
Anaplastic large cell lymphoma (ALCL) is a rare, fast-growing cancer. It mainly affects T-cells. Finding it early helps improve treatment success.
ALK-positive ALCL has a much better chance of survival. About 80% of people live for five years or more. ALK-negative ALCL has lower survival chances.
New treatments like chemotherapy and targeted drugs, such as brentuximab vedotin, help patients live longer and feel better.
Regular doctor visits are important to check if the cancer stays away. Early detection of its return can improve long-term health.
People with textured breast implants should know about the risk of breast implant-associated ALCL (BIA-ALCL). Talk to your doctor and get regular check-ups.
What is Anaplastic Large Cell Lymphoma?
Overview
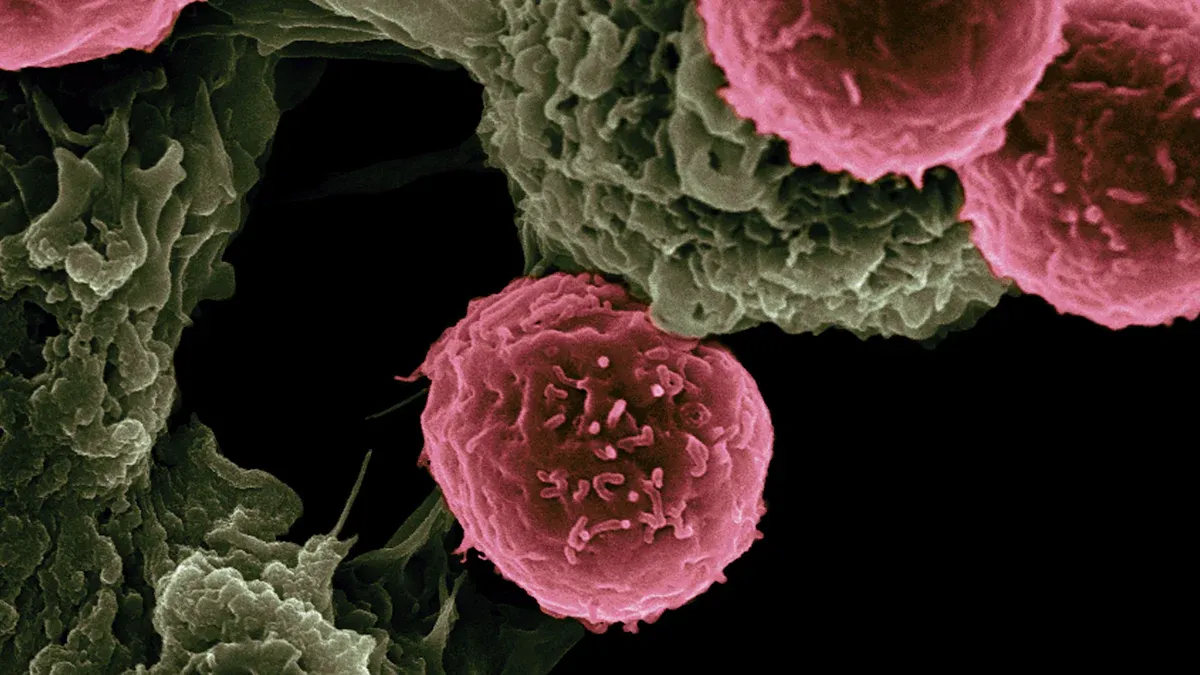
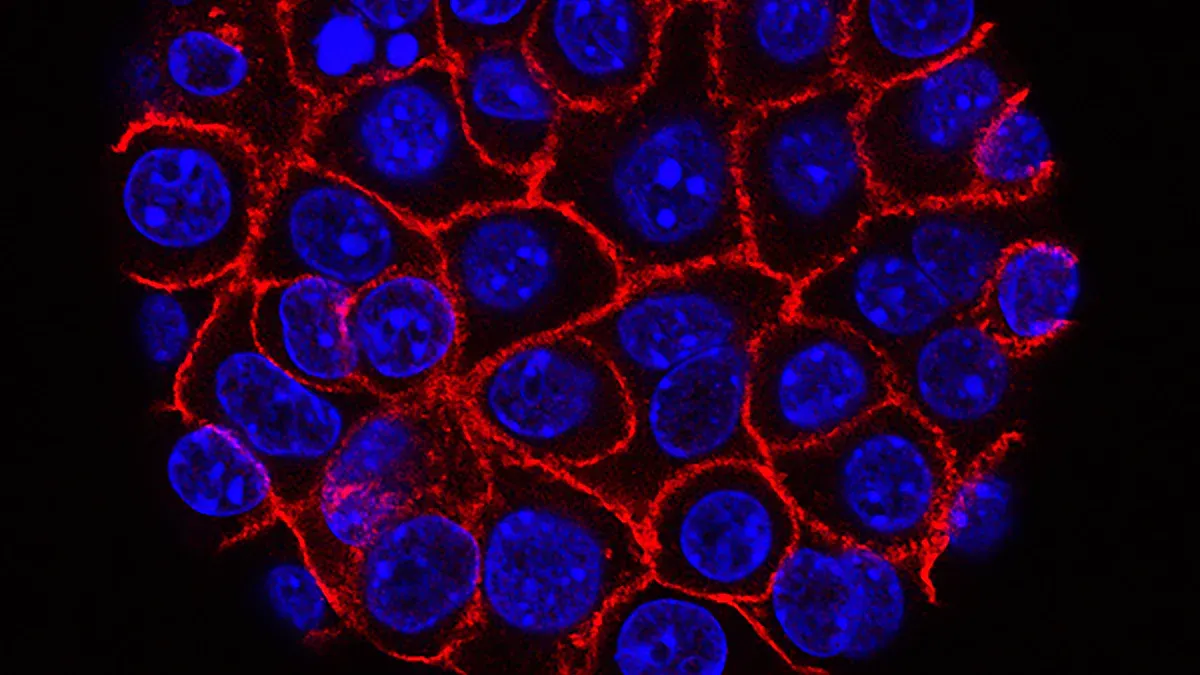
Anaplastic large cell lymphoma is a rare subtype of non-Hodgkin lymphoma that primarily affects T-cells. It accounts for only 1% to 2% of all lymphomas and falls under the category of peripheral T-cell lymphomas. This disease has several defining characteristics that set it apart from other lymphomas:
Cells with anaplastic cytology
Constant expression of the CD30 antigen on the cell membrane
Frequent involvement of the skin and other extranodal sites
A tendency to affect younger individuals, with a higher prevalence in males
The CD30 antigen plays a crucial role in identifying this type of lymphoma. Its presence on the surface of ALCL cells helps doctors diagnose and classify the disease accurately.
Types of ALCL
ALK-positive and ALK-negative ALCL
The World Health Organization classifies systemic anaplastic large cell lymphoma into two main subtypes: ALK-positive and ALK-negative. The ALK gene determines this classification through specific chromosomal translocations. These translocations create the NPM-ALK fusion protein, which acts as a continuously active tyrosine kinase. This protein drives tumor growth and is linked to a better prognosis in ALK-positive cases. ALK-positive ALCL is the most common subtype and generally responds well to treatment. ALK-negative ALCL lacks this fusion protein and often presents a more challenging prognosis.
Primary Cutaneous ALCL
Primary cutaneous ALCL primarily affects the skin. It often appears as red or purple lesions that may ulcerate. This subtype tends to remain localized to the skin and has a more favorable outcome compared to systemic forms. You might notice these lesions on your trunk, arms, or legs.
Breast Implant-Associated ALCL (BIA-ALCL)
BIA-ALCL is a rare subtype linked to textured breast implants. It typically develops in the scar tissue or fluid surrounding the implant. Symptoms may include swelling, pain, or fluid buildup around the implant. Studies show that the lifetime prevalence of BIA-ALCL in individuals with textured implants is approximately 33 per million. The incidence rate ranges from 4.5 to 31.1 cases per 100 million annually, depending on the type of implant and other factors.
Symptoms of Anaplastic Large Cell Lymphoma
General Symptoms
Anaplastic large cell lymphoma often presents with symptoms that can affect your entire body. These symptoms, known as systemic symptoms, may include:
Swollen lymph nodes: This is often the first noticeable sign. It occurs due to the accumulation of lymphoma cells in the lymphatic system.
Fever: Persistent, unexplained fevers are common and are categorized as B symptoms.
Night sweats: You may experience heavy sweating during the night, which can disrupt your sleep.
Weight loss: Unexplained weight loss of 10% or more of your body weight within six months is another B symptom.
Fatigue: This can result from the body's response to the disease or anemia caused by the lymphoma.
These symptoms may overlap with other illnesses, so consulting a healthcare provider is crucial for an accurate diagnosis.
Symptoms by Subtype
The symptoms of anaplastic large cell lymphoma can vary depending on the subtype. Below is a breakdown of the key differences:
ALCL Subtype | Symptoms |
|---|---|
Primary Cutaneous ALCL | - Skin lesions, often appearing as single, raised, discolored nodules. |
- Typically located on the head, neck, arms, or legs. | |
- Lesions may itch but are usually painless. | |
- In some cases, they can ulcerate and bleed. | |
- These lesions usually do not resolve without treatment. | |
Breast Implant-Associated ALCL | |
- Pain or discomfort near the implant. | |
- Rarely, a palpable lump or capsular contracture may develop. |
If you notice skin lesions or swelling near a breast implant, it is essential to seek medical advice. Early detection can significantly improve outcomes.
Causes and Risk Factors of ALCL
Causes
Genetic mutations and chromosomal abnormalities
Genetic mutations play a significant role in the development of anaplastic large cell lymphoma. Specific mutations, such as those in the TP53 and STAT3 genes, are more common in certain subtypes. For example, TP53 mutations occur in 11% of ALK-positive cases and 23% of ALK-negative cases. The STAT3 mutation, however, is found in 26% of ALK-negative cases but is absent in ALK-positive ones. Below is a table summarizing the prevalence of key genetic mutations:
Gene | Prevalence in ALK+ ALCL | Prevalence in ALK− ALCL | Overall Prevalence |
|---|---|---|---|
TP53 | 11% | 23% | 16% |
STAT3 | 0% | 26% | 24% |
JAK1 | 0% | 26% | 16% |
EPHA5 | N/A | N/A | 16% |
PRDM1 | N/A | N/A | 13.5% |
LRP1B | N/A | N/A | 11% |
KMT2D | N/A | N/A | 11% |
These mutations disrupt normal cell functions, leading to uncontrolled growth and tumor formation.
Role of the ALK gene in ALK-positive ALCL
The ALK gene plays a critical role in ALK-positive anaplastic large cell lymphoma. Chromosomal translocations involving the ALK gene result in the creation of fusion proteins, such as the NPM-ALK fusion protein. This protein acts as a continuously active tyrosine kinase, driving tumor growth. The translocation occurs between chromosomes 2 and 5, leading to the expression of this abnormal protein. This process is essential for the development of ALK-positive ALCL and contributes to its distinct behavior and better prognosis compared to ALK-negative cases.
Risk Factors
Age and gender
Your age and gender can influence your risk of developing anaplastic large cell lymphoma. ALK-positive cases are more common in males under 30 years old and tend to have a better prognosis. In contrast, ALK-negative cases typically affect individuals over 60 years old, regardless of gender, and often have a less favorable outcome. The table below highlights these demographic factors:
Demographic Factor | Description | Prognosis |
|---|---|---|
Age < 30 years | More common in males with ALK+ ALCL | More favorable |
Age > 60 years | Affects both genders with ALK− ALCL | Less favorable |
Breast implants and BIA-ALCL
Breast implants, particularly textured ones, increase the risk of developing breast implant-associated ALCL (BIA-ALCL). This risk is higher for individuals with Biocell textured implants from Allergan. These implants have a unique surface texture linked to a higher incidence of the disease. Researchers believe the rough surface may cause chronic inflammation, which could trigger lymphoma in susceptible individuals. Key points include:
Textured implants pose a greater risk than smooth ones.
Chronic inflammation caused by the implant surface may contribute to lymphoma development.
If you have textured implants, regular check-ups can help detect any early signs of BIA-ALCL.
Diagnosis of Anaplastic Large Cell Lymphoma
Diagnostic Methods
Physical examination and biopsy
Diagnosing anaplastic large cell lymphoma begins with a thorough physical examination. Your doctor will check for swollen lymph nodes, skin lesions, or other abnormalities. If they suspect lymphoma, they will recommend a biopsy. This procedure involves removing a small sample of tissue or fluid for analysis. Biopsies can be performed surgically or with a needle, depending on the location of the suspected lymphoma.
The biopsy is essential for identifying cancer cells. Pathologists use advanced techniques like immunohistochemistry to detect specific proteins, such as CD30, on the surface of lymphoma cells. This step helps confirm the diagnosis and classify the lymphoma subtype. Accurate diagnosis ensures you receive the most effective treatment plan.
Laboratory and imaging tests (e.g., PET and CT scans)
After the biopsy, laboratory and imaging tests help determine the extent of the disease. Blood tests, including complete blood counts, evaluate your overall health and detect any abnormalities in blood cell production. Imaging tests play a crucial role in locating tumors and assessing their spread.
Here are some common imaging techniques used in diagnosing anaplastic large cell lymphoma:
CT scan: Identifies enlarged lymph nodes and evaluates organ involvement.
PET scan: Detects active lymphoma lesions by highlighting areas of increased metabolic activity.
MRI: Assesses lymphoma in the central nervous system or musculoskeletal system.
Ultrasound: Examines superficial lymph nodes and evaluates their size and characteristics.
Bone scans: Detect abnormal bone activity when bone involvement is suspected.
Chest X-ray: Checks for abnormalities in the chest, such as enlarged lymph nodes or lung involvement.
Molecular diagnostic techniques, such as cytogenetics and RT-PCR, are also vital. These methods detect genetic changes, like ALK gene translocations, that are specific to certain subtypes of anaplastic large cell lymphoma. Combining these diagnostic tools ensures a comprehensive evaluation, guiding your treatment plan effectively.
Treatment Options for Anaplastic Large Cell Lymphoma
Standard Treatments
Chemotherapy and radiation therapy
Chemotherapy remains the cornerstone of treatment for systemic anaplastic large cell lymphoma. The most commonly used regimen is the CHOP protocol, which combines cyclophosphamide, doxorubicin, vincristine, and prednisone. For younger patients with ALK-positive ALCL, adding etoposide to the CHOP regimen (CHOEP) has shown significant improvements in event-free survival. Another option, the B-CHP regimen, incorporates brentuximab vedotin, a targeted therapy, alongside chemotherapy agents.
Radiation therapy is often used in early-stage cases or to target specific lymph node clusters. External beam radiation delivers precise doses to affected areas, helping to eliminate residual cancer cells after chemotherapy. This combination of treatments increases the likelihood of remission and long-term survival.
Targeted Therapies
ALK inhibitors and Brentuximab vedotin
Targeted therapies have revolutionized the treatment of anaplastic large cell lymphoma. Brentuximab vedotin, an FDA-approved drug, targets the CD30 protein found on ALCL cells. In the ECHELON-2 trial, combining brentuximab vedotin with CHP chemotherapy significantly improved progression-free survival (48.2 months vs. 20.8 months) and overall survival compared to CHOP. This therapy is well-tolerated and effective for both pediatric and adult patients.
For ALK-positive ALCL, ALK inhibitors like crizotinib offer another powerful option. Crizotinib is FDA-approved for pediatric patients with relapsed or refractory ALK-positive ALCL. Clinical studies report an overall response rate of 88%, with 81% achieving complete remission. These therapies provide hope for patients with challenging cases.
Advanced Approaches
Stem cell transplantation
Stem cell transplantation is a promising option for patients whose lymphoma returns after initial treatment. This procedure involves replacing damaged bone marrow with healthy stem cells, either from your own body (autologous) or a donor (allogeneic). It helps restore normal blood cell production and offers a chance for long-term remission.
Clinical trials
Clinical trials explore innovative treatments for advanced ALCL. For example, a Phase III trial is comparing vinblastine and vincristine in chemotherapy for newly diagnosed advanced-stage ALCL. These trials provide access to cutting-edge therapies and contribute to medical advancements.
Prognosis and Outlook for ALCL
Prognostic Factors
ALK-positive vs. ALK-negative outcomes
Your prognosis for anaplastic large cell lymphoma depends significantly on whether the disease is ALK-positive or ALK-negative. ALK-positive cases generally have better outcomes due to the presence of the ALK fusion protein, which makes the disease more responsive to treatment. In contrast, ALK-negative cases often show poorer survival rates.
ALK Status | |
|---|---|
ALK-positive | 70-80% |
ALK-negative | 15-45% |
Additionally, ALK-negative lymphomas have a higher likelihood of relapse and long-term survival rates below 50%. This makes early and aggressive treatment crucial for improving outcomes.
Disease stage at diagnosis
The stage of the disease at diagnosis also plays a critical role in your prognosis. Advanced stages (III/IV) correlate with poorer outcomes and higher treatment failure rates. Early-stage detection improves the chances of successful treatment and long-term remission.
Advanced clinical stages often lead to worse outcomes.
Stage III/IV disease is associated with higher rates of treatment failure.
Long-Term Outlook
Survival rates and remission
Survival rates vary based on ALK status and treatment response. For ALK-positive patients, the 3-year overall survival rate reaches nearly 90%, while ALK-negative cases show a lower rate of 62%. Long-term remission is more likely in ALK-positive cases, but ALK-negative patients face a higher risk of relapse within five years.
ALK Status | 3-Year Overall Survival | 5-Year Overall Survival |
|---|---|---|
ALK-positive | 89.8% | 58% |
ALK-negative | 62% | 36% |
Importance of follow-up care
Follow-up care plays a vital role in maintaining remission and detecting relapses early. Regular check-ups, imaging tests, and blood work help monitor your condition. For cutaneous ALCL, localized cases often have a favorable outlook, though around 40% may relapse. Systemic ALCL and BIA-ALCL also show promising outcomes with appropriate treatment and follow-up.
Tip: Staying consistent with follow-up appointments can significantly improve your long-term prognosis.
Anaplastic large cell lymphoma (ALCL) is a rare but treatable condition. You’ve learned about its symptoms, causes, and the advanced therapies available today. Treatments like chemotherapy, targeted drugs, and stem cell transplants have significantly improved outcomes, especially for ALK-positive cases. For BIA-ALCL, surgery often removes the implants and scar tissue, with additional treatments like radiation or chemotherapy if needed.
If you suspect symptoms or need guidance, professional resources can help. Explore treatment guidelines and support at ThePSF.org/PROFILE or PlasticSurgery.org/ALCL. Early action ensures the best care and outcomes.
Note: Always consult a healthcare provider for personalized advice tailored to your needs.
FAQ
What is the difference between ALK-positive and ALK-negative ALCL?
ALK-positive ALCL has a genetic mutation involving the ALK gene, which improves treatment response and prognosis. ALK-negative ALCL lacks this mutation and often has a poorer outcome. Doctors use this classification to guide treatment decisions and predict survival rates.
Can ALCL spread to other parts of the body?
Yes, systemic ALCL can spread to lymph nodes, skin, lungs, liver, or bones. Early diagnosis and treatment reduce the risk of widespread disease. Regular follow-ups help monitor for any signs of progression or relapse.
Is breast implant-associated ALCL (BIA-ALCL) a type of breast cancer?
No, BIA-ALCL is not breast cancer. It is a rare lymphoma that develops in the scar tissue or fluid around textured breast implants. Removing the implant and surrounding tissue often resolves the condition, but additional treatments may be necessary.
Are there any lifestyle changes that can help during ALCL treatment?
Yes, maintaining a healthy diet, staying physically active, and managing stress can support your overall well-being during treatment. Always consult your doctor before making significant lifestyle changes to ensure they align with your treatment plan.
How can I reduce my risk of developing BIA-ALCL?
Choosing smooth breast implants instead of textured ones may lower your risk. Regular check-ups with your doctor can help detect early signs of BIA-ALCL. If you notice swelling or pain near an implant, seek medical advice immediately.
See Also
Exploring Treatment Options For Acute Myeloid Dendritic Cell Leukemia
Understanding Acute Lymphoblastic Leukemia: Symptoms And Overview
Adamantinoma: Understanding Its Impact On The Human Body
Adrenocortical Adenoma: Symptoms And Treatment Insights Explained

