Why Not Every Cancer Screening Is Risk-Free
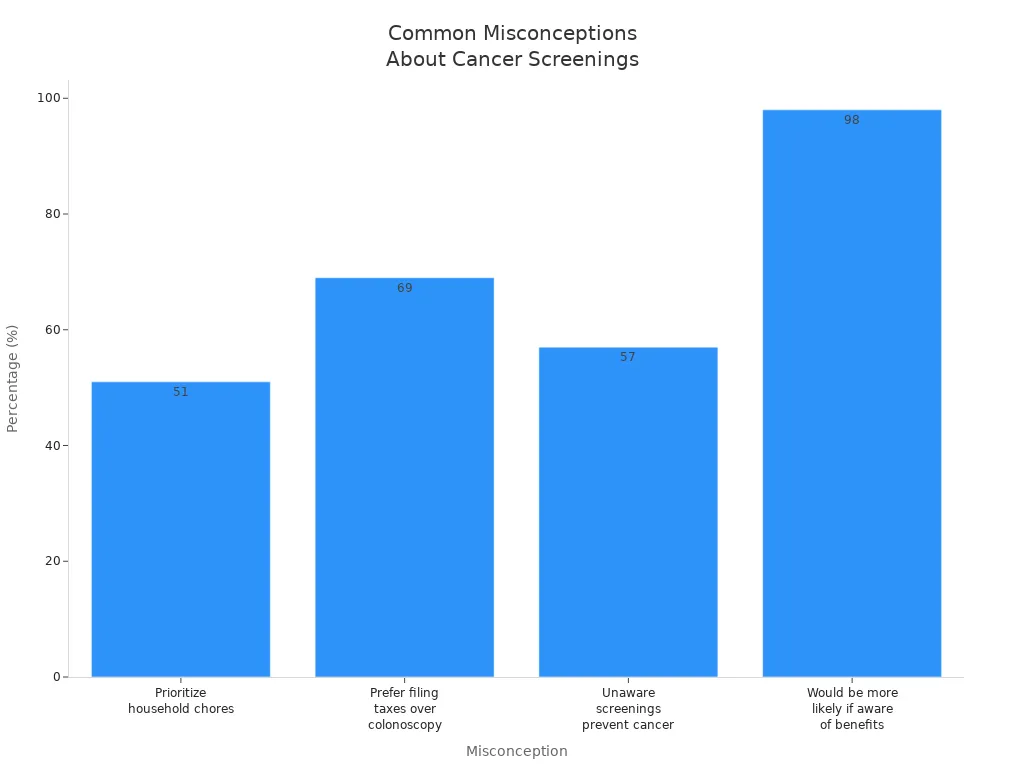
Have you ever wondered if cancer screenings are always safe? Many people feel nervous about these tests, and some even say they would rather file taxes than get a colonoscopy. Take a look at this chart showing how common these feelings are:
You might believe that Are All Cancer Screenings Risk-Free? Understanding the Realities is simple, but not every screening is completely without risk. Before you make a decision, talk with your doctor and learn about both the benefits and the possible risks.
Key Takeaways
Not all cancer screenings are risk-free. Understand both the benefits and potential harms before deciding.
False positives and negatives can lead to unnecessary stress and treatments. Always discuss results with your doctor.
Screening guidelines vary by age and health. Consult your doctor to determine the right screenings for you.
Early detection can save lives, but some screenings may not improve outcomes. Weigh the risks and benefits carefully.
Open communication with your doctor is key. Ask questions to make informed decisions about your health.
Are All Cancer Screenings Risk-Free? Understanding the Realities
Common Misconceptions
Many people believe that cancer screenings are always safe and only bring benefits. You might hear that early detection always saves lives or that more testing is always better. These ideas sound comforting, but they do not tell the whole story. Are All Cancer Screenings Risk-Free? Understanding the Realities means looking at both the good and the bad.
Note: Not every screening test is right for everyone. Some tests can cause more harm than good if used in the wrong group.
You may think that a test will always find cancer if it is there, or that a normal result means you are completely safe. In reality, no test is perfect. Some people get results that are not correct. This can lead to worry, more tests, or even treatments you do not need.
Why Risks Exist
Screenings can help find cancer early, but they also come with risks. Are All Cancer Screenings Risk-Free? Understanding the Realities requires you to know about these possible harms. Here is a table that shows some main risks:
Risk Type | Description |
|---|---|
False Negative | Screening can miss cancers, leading to a false sense of security. |
False Positive | Abnormal results can occur when no cancer is present, causing unnecessary worry and follow-up tests. |
Overdiagnosis | Harmless cancers may be detected that would not cause problems, leading to unnecessary treatment. |
Side Effects | Some tests may cause pain, discomfort, or light bleeding. |
You might be surprised to learn how often these problems happen. For example:
For some groups, like female smokers or pregnant women, the chance of a false positive can be as high as 88%.
These numbers show that Are All Cancer Screenings Risk-Free? Understanding the Realities is not as simple as it seems. A false positive can lead to more tests, which may be stressful or even risky. A false negative can make you think you are healthy when you are not.
Some screening tests can also cause physical problems. You might feel pain, discomfort, or even have light bleeding after certain tests. Sometimes, finding a cancer does not help you live longer or feel better, especially if the cancer would never have caused problems.
Not every person should get every screening. Guidelines exist to help you and your doctor decide what is best for you. For example:
Cervical cancer screening should start at age 25. People younger than 25 do not need this test.
Lung cancer screening is for people aged 50-80 who have smoked a lot.
Breast cancer screening is usually for women aged 50 and older.
Prostate cancer screening should be a choice you make with your doctor, starting at age 50.
Colon cancer screening is recommended up to age 75. After that, you should talk to your doctor about whether to continue.
Tip: Always ask your doctor if a screening test is right for you. Are All Cancer Screenings Risk-Free? Understanding the Realities means knowing when a test can help and when it might cause harm.
Medical groups also say that people with serious health problems or a short life expectancy may not benefit from screening. For these people, the risks may be greater than the benefits.
Are All Cancer Screenings Risk-Free? Understanding the Realities helps you make smart choices. You should always weigh the possible benefits and risks before deciding on a screening test.
Cancer Screening Basics
What Is Screening
Cancer screening means you get tested for cancer before you have any symptoms. You do not wait until you feel sick. Health experts say screening is a way to find cancer early, sometimes even before it causes problems. You might hear your doctor talk about screening as a preventive healthcare service. The goal is to spot precancerous changes or small tumors that you cannot see or feel.
Screening uses simple tests on people who feel healthy.
You do not need to have symptoms to get screened.
Doctors use screening to catch cancer in its early, hidden stage.
Screening helps lower the number of people who die from cancer. It can also find abnormal cells before they turn into cancer.
Benefits
You may wonder why screening matters. The main benefit is early detection. When doctors find cancer early, treatment often works better. You have a higher chance of beating cancer if you start treatment before it spreads. Screening can also find changes in your body that could become cancer. Treating these changes can stop cancer before it starts.
Here are some important benefits:
Early diagnosis reduces late-stage cancer cases.
Screening programs for breast, cervical, and colorectal cancers save lives.
Early detection increases the chance of successful treatment.
Screening lowers the number of deaths from cancer.
A study found that screening cut lung cancer deaths by 39% in high-risk patients. Breast cancer deaths in the U.S. dropped from 48 to 27 per 100,000 women, with screening playing a big role. Colorectal cancer deaths also fell by almost half because of screening. Are All Cancer Screenings Risk-Free? Understanding the Realities means knowing that not every screening improves your outcome, but many do when used the right way.
Screening works best when you follow expert guidelines and talk with your doctor about your risks.
Risks of Cancer Screening

False Positives
You might think a positive test always means cancer, but that is not true. Sometimes, a screening test says you have cancer when you do not. This is called a false positive. False positives can cause stress, more tests, and even unnecessary treatments. For example, mammograms have a single test false-positive rate of 11%. Over ten years, the risk rises to 50–60%. PSA tests for prostate cancer can have a false-positive rate as high as 75%. Colonoscopies have a lower rate, between 2–8%.
Screening Type | Single Test False-Positive Rate | 10-Year Cumulative Risk |
|---|---|---|
Mammogram | 11% | 50–60% |
PSA Test | Up to 75% | 60.4% (after 14 tests) |
Colonoscopy | 2–8% | Not applicable* |
A false positive can lead you to worry about your health and go through more procedures that you may not need.
False Negatives
A false negative happens when a test misses cancer that is actually there. You may feel safe after a normal result, but sometimes cancer goes undetected. This can delay treatment and lower your chances of a good outcome. False negatives in breast and cervical cancer screening can lead to late detection. Some people may lose trust in screening programs because of this. Most people do not feel long-term distress from false negatives, but high-risk groups may feel more stress.
They may reduce trust in screening programs.
Overdiagnosis
Screening sometimes finds cancers that would never cause problems. Doctors call this overdiagnosis. You might get treatment for a cancer that would not have harmed you. In breast cancer screening, about 15.4% of cases are overdiagnosed. This means you could face surgery, radiation, or medication you do not need.
Type of Cancer | Overdiagnosis Rate |
|---|---|
Breast Cancer | 15.4% |
Overdiagnosis can lead to unnecessary treatments and side effects.
Physical Complications
Screening tests can cause physical harm. You may feel discomfort or bruising after a test. Some procedures, like colonoscopies, can cause serious harm such as a tear in the colon. Tests that use radiation, like some scans, can damage healthy cells. Are All Cancer Screenings Risk-Free? Understanding the Realities means knowing that even a simple test can have risks.
Type of Complication | Description |
|---|---|
Minor Physical Harm | Screening tests can cause minor physical harm like bruising or discomfort. |
Serious Physical Harm | Serious physical harm can occur, such as tearing the colon during colon cancer screening. |
Radiation Exposure | Some screening tests use low doses of radiation that can damage healthy cells. |
Always talk with your doctor about the risks and benefits before you decide on a screening test.
Screening Guidelines
Who Should Be Screened
You might wonder if everyone needs cancer screening. The answer depends on your age, health, and risk factors. Doctors use guidelines to help decide who should get screened and when to start.
Most adults aged 50 to 75 should get screened for colorectal cancer.
Some groups may need to start earlier. Black adults may begin at 45. If you have a family history, you may start at 40.
The American Cancer Society suggests starting at 45 for all adults.
Women aged 40 to 74 should have mammograms every one or two years.
Screening should match your health, life expectancy, and personal values.
Screening guidelines can look different in other countries. Here is a quick comparison:
Country/Region | Recommended Screening Age | Screening Methods | Screening Intervals |
|---|---|---|---|
United States | 40-74 years | Mammography | Annual or biennial |
Developed Countries | 40-74 years | Mammography, MRI | Annual or biennial |
Japan/South Korea | 40-45 years | Mammography | Varies |
Your doctor will help you decide when to start based on your health and family history.
When to Stop Screening
You do not need to continue cancer screening forever. Doctors look at your health, life expectancy, and how much you might benefit from more tests.
Factor | What It Means for You |
|---|---|
Health Status | Good health may mean you keep screening longer. Poor health may mean stopping sooner. |
Life Expectancy | If you are not likely to live 10 more years, screening may not help you. |
Physician Advice | Your doctor can help you weigh the risks and benefits. |
Personal Beliefs | You may choose to stop if you feel the burdens outweigh the benefits. |
Screening tests can have risks right away, like pain or complications. The benefits, such as preventing cancer deaths, often take years to appear. For example, it takes about 10 years for mammograms or stool tests to save one life out of 1,000 people screened.
The U.S. Preventive Services Task Force says women can stop cervical cancer screening after age 65 if they have had regular, normal results.
For adults over 75, screening should be a personal choice. After age 85, most people can stop.
Always talk with your doctor about when to stop screening. Your health and wishes matter most.
Making Informed Choices
Weighing Benefits and Risks
You face many choices when it comes to cancer screening. Tools like cancer risk assessment calculators can help you understand your personal risk and learn more about possible side effects. These tools work best when you use them with support from your doctor. Sometimes, you may find it hard to understand your own risk or what side effects mean for you. Many tools do not include genetic testing information, so you may need extra help to get a full picture.
Here is a table showing how experts use frameworks to guide screening decisions:
Framework Description | Key Findings |
|---|---|
Optimization framework for risk-based cancer screening | Identifies thresholds for screening intervals based on risk, potentially reducing advanced cancer incidence by targeting high-risk individuals. |
Cancer screening decisions should match your health needs and personal values. You can use these tools to make choices that fit you best.
Talking to Your Doctor
You should always talk with your doctor before starting or stopping any cancer screening. Shared decision-making helps you get involved in your care. This approach improves your knowledge about screening options and helps you understand both risks and benefits. You and your doctor can work together to make choices that match your values and preferences. This teamwork can also reduce confusion and improve communication.
Here are some questions you can ask your doctor:
What cancer screening tests do you recommend for me?
Why do you recommend those tests?
Do I need these tests right away?
Can you do those tests or should I see a specialist?
Are there screening tests that I can do at home?
How often should I get the screening tests?
Asking questions helps you feel confident and informed about your health decisions.
Finding Reliable Information
You need trustworthy sources to learn about cancer screening. Many people prefer online research, while others like materials from their doctor's office or print publications. Most patients rely on their doctors to help them judge which tests are backed by strong evidence.
Source | Description |
|---|---|
American College of Obstetricians and Gynecologists (ACOG) | Offers guidelines on breast cancer screening and stresses shared decision-making. |
U.S. Preventive Services Task Force | Recommends screening intervals and methods based on population data. |
American Cancer Society (ACS) | Shares guidelines that include patient values and preferences. |
National Comprehensive Cancer Network | Reviews evidence for screening recommendations. |
Reliable information helps you make smart choices and avoid unnecessary risks.
You need to know both the benefits and risks before choosing a cancer screening. Screening can save lives, but it may also cause stress or lead to unnecessary tests. Open talks with your doctor help you make the best choices for your health. Good communication and clear information support your decisions.
Many people do not realize that cancer screening is complex. You should always ask questions and seek advice.
Trusted resources for more information:
FAQ
What should you do if you get a false positive result?
You should stay calm and talk with your doctor. Your doctor may order more tests to check your health. False positives happen often, so do not panic. Ask questions and follow your doctor’s advice.
Can cancer screening cause pain or side effects?
Some tests may cause mild pain or discomfort. You might feel sore or notice light bleeding. Most side effects go away quickly. Tell your doctor if you feel worried or have strong pain.
How do you know which screening tests you need?
Your doctor looks at your age, health, and family history. You should ask which tests fit your needs. Guidelines help doctors choose the best tests for you.
Is it safe to skip a recommended screening?
Skipping a screening can raise your risk of missing cancer early. You should talk with your doctor before making this choice. Your doctor can explain the risks and benefits.
See Also
An In-Depth Overview of Various Cancer Types
Understanding Lung Adenocarcinoma: Causes and Risk Elements
Recognizing Esophageal Cancer: Symptoms and Underlying Causes

