What to Know About Basaloid Squamous Cell Lung Carcinoma
Basaloid squamous cell lung carcinoma represents a rare and aggressive form of lung cancer. It accounts for approximately 3.9% to 6.3% of all lung cancer cases, as observed in studies involving non-small cell lung cancer patients. This subtype is distinguished by its unique histological structure, with less than 50% squamous cell components, and a high tendency for metastasis. Its poor prognosis stems from intrinsic resistance to chemotherapy and rapid disease progression. Understanding its clinical features and behavior is crucial for improving early detection and management strategies.
Key Takeaways
Basaloid squamous cell lung carcinoma is a rare, fast-growing lung cancer. It makes up about 3.9% to 6.3% of cases.
Symptoms include a long-lasting cough, trouble breathing, and chest pain. These make it hard to find early.
Doctors use CT scans and biopsies to diagnose it. Special tests help tell it apart from other lung cancers.
People with this cancer have lower survival rates than others. This shows why finding and treating it early is important.
New treatments, like immunotherapy, may help patients live longer with this tough cancer.
Clinical Characteristics of Basaloid Squamous Cell Lung Carcinoma
Symptoms and Presentation
Common symptoms
Patients with basaloid squamous cell lung carcinoma often experience respiratory symptoms. These include persistent cough, shortness of breath (dyspnea), and chest pain. The table below highlights the frequency of common symptoms observed in patients:
Symptom | Number of Patients |
|---|---|
Cough | 3 |
Dyspnea | 2 |
How the disease typically presents in patients
This carcinoma tends to present with more severe respiratory symptoms compared to other lung cancers. Patients often exhibit signs of endobronchial tumor growth, obstructive pneumonia, or atelectasis on imaging. Unlike other subtypes, cavitation is absent, and internal necrosis is less frequent. The disease progresses rapidly, with earlier distant metastasis contributing to its poor prognosis.
Pathological Features
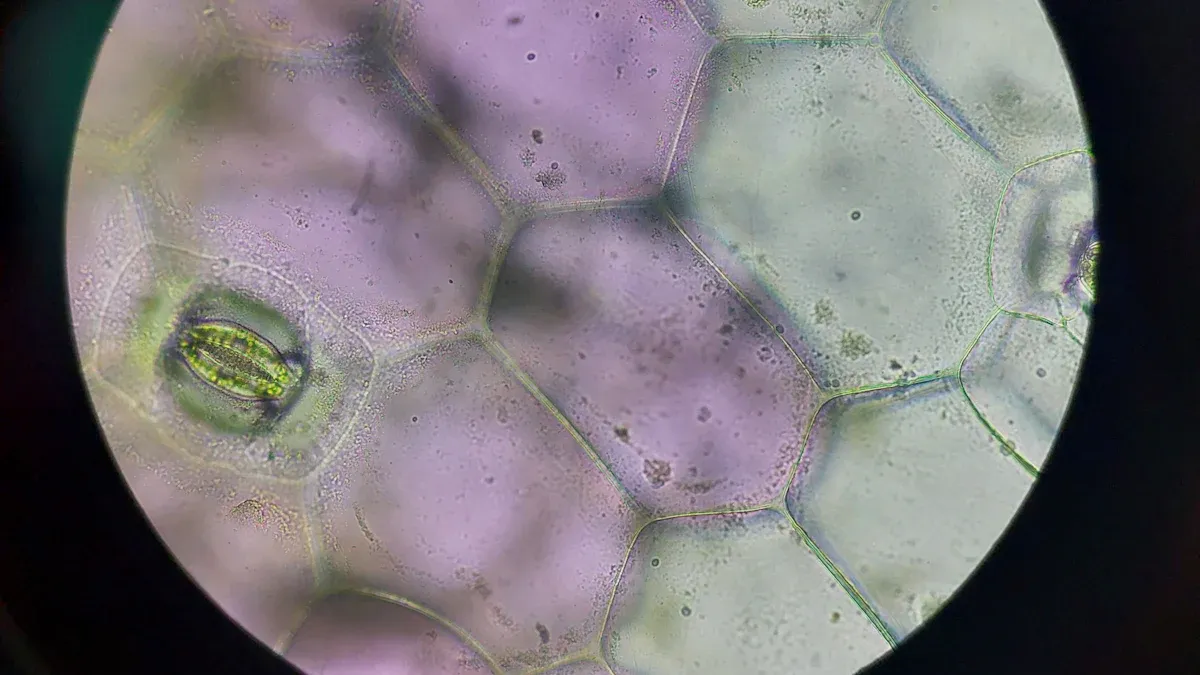
Description of basaloid squamous cell carcinoma under the microscope
Under microscopic examination, basaloid squamous cell lung carcinoma displays unique features:
Small cells arranged in a lobular growth pattern with peripheral palisading.
Centrilobular foci of necrosis.
Evidence of squamous differentiation, such as intercellular bridges and keratin production.
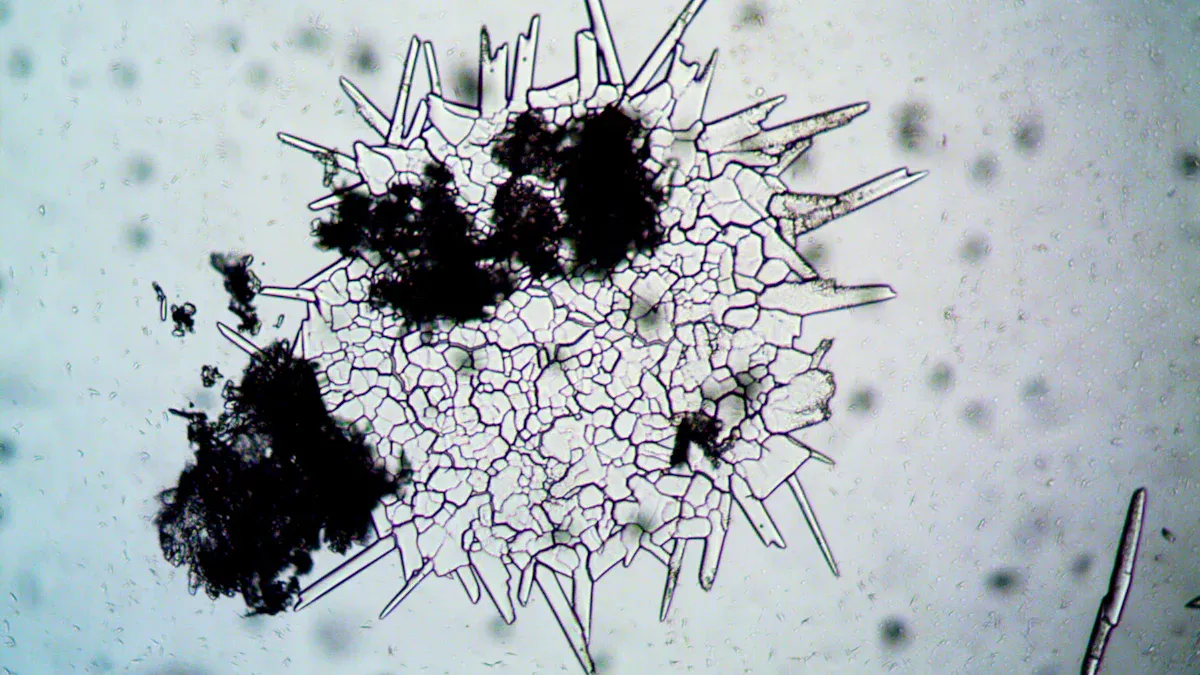
Key differences from other types of lung cancer
This carcinoma differs from other lung cancer subtypes due to its distinct histopathological characteristics:
A combination of squamous and basal cell carcinoma features, with squamous components comprising less than 50%.
A lobular growth pattern with peripheral palisading, which limits significant necrosis.
A higher rate of metastasis and mortality compared to other lung cancers.
Risk Factors and Causes
Smoking and other environmental risk factors
Tobacco smoking is a major environmental factor linked to basaloid squamous cell lung carcinoma. Heavy smokers show a significantly higher prevalence of this disease.
Genetic predispositions and other potential causes
While smoking remains the primary risk factor, genetic predispositions may also play a role. Research into specific genetic mutations associated with this carcinoma is ongoing.
Diagnosis of Basaloid Squamous Cell Lung Carcinoma
Diagnostic Methods
Imaging techniques (e.g., CT scans, X-rays)
Imaging plays a critical role in diagnosing basaloid squamous cell lung carcinoma. Among the available techniques, CT scans are the most effective. They provide detailed insights into tumor size, location, and enhancement characteristics. Specific findings, such as irregular tumor margins and the presence of necrosis, help differentiate this carcinoma from other lung cancers. X-rays, while less detailed, can reveal abnormalities like lung masses or atelectasis, prompting further investigation. These imaging tools are essential for initial detection and staging.
Role of biopsy and histopathological analysis
A definitive diagnosis of basaloid squamous cell lung carcinoma requires biopsy and histopathological analysis. Pathologists often face challenges due to the tumor's morphological similarities with other lung cancers. Immunohistochemistry (IHC) is crucial for accurate identification. It highlights specific markers, such as p40 positivity and TTF1 negativity, which distinguish this carcinoma from other subtypes. In some cases, features resembling small cell carcinoma may appear, but thorough histopathological examination confirms the diagnosis. This process underscores the importance of combining imaging with tissue analysis for reliable results.
Challenges in Diagnosis
Overlap with other lung cancer subtypes
Basaloid squamous cell lung carcinoma shares several morphological features with other aggressive lung cancers, such as poorly differentiated squamous cell carcinoma, small cell lung carcinoma, and large cell neuroendocrine carcinoma. These similarities complicate diagnosis, especially when using small biopsy samples. Immunohistochemistry aids in differentiation, but overlapping patterns can still pose significant challenges. For instance, hypercellularity and small, hyperchromatic cells are common in multiple subtypes, making precise identification difficult.
Difficulty in early detection due to nonspecific symptoms
Early detection of basaloid squamous cell lung carcinoma remains challenging. Symptoms like persistent cough and chest pain are nonspecific and often attributed to other conditions. Small biopsy specimens frequently provide limited cellular material, further complicating diagnosis. Additionally, the tumor's rapid progression and tendency for early metastasis reduce the window for early intervention. These factors highlight the need for advanced diagnostic tools and increased awareness among healthcare providers.
Prognosis of Basaloid Squamous Cell Lung Carcinoma
Survival Rates and Outcomes
Typical survival rates for basaloid squamous cell lung carcinoma
The survival rates for basaloid squamous cell lung carcinoma remain significantly lower compared to other lung cancer subtypes. The table below outlines survival rates over time:
Survival Time | Survival Rate |
|---|---|
1 year | Not specified |
3 years | Good agreement with actual rates |
5 years | Good agreement with actual rates |
These figures highlight the aggressive nature of this carcinoma and its poor long-term outcomes.
Comparison with other lung cancer subtypes
Basaloid squamous cell lung carcinoma often exhibits worse survival outcomes than other lung cancer subtypes. Key differences include:
Lower survival rates at earlier stages (I and II).
Earlier distant metastasis, which contributes to reduced survival.
A clinical study revealed that the median survival time for basaloid carcinoma was 29 months, compared to 49 months for non-small cell lung cancer (NSCLC). The 5-year survival rate for basaloid carcinoma was 27%, significantly lower than the 44% observed in NSCLC.
Factors Influencing Prognosis
Impact of cancer stage at diagnosis
The stage of cancer at diagnosis plays a critical role in determining prognosis. The table below illustrates how different stages influence survival outcomes:
Evidence Type | Description |
|---|---|
T stage | Higher T stages correlate with worse prognoses (P < 0.001). |
N stage | Higher N stages are associated with poorer survival outcomes (P = 0.009). |
M stage | Advanced M stages significantly impact overall survival (P < 0.001). |
Surgical Intervention | Lobectomy leads to better survival rates compared to sublobar resection (OR 0.389). |
Patients diagnosed at earlier stages generally experience better outcomes, emphasizing the importance of early detection.
Role of treatment options and patient health
Treatment options and overall patient health significantly influence survival. Lobectomy, a surgical procedure, has been shown to improve outcomes compared to sublobar resection. Additionally, factors such as age, cancer stage, and overall health status directly impact prognosis. Patients in good health and those who receive aggressive treatment tend to achieve better survival rates.
Treatment and Management of Basaloid Squamous Cell Lung Carcinoma
Current Treatment Approaches
Surgery, chemotherapy, and radiation therapy
The treatment of basaloid squamous cell lung carcinoma typically follows standard protocols for squamous cell carcinoma. Surgery remains the primary option for patients with localized disease, offering the best chance for long-term survival. Lobectomy, which involves removing a lobe of the lung, is often preferred over sublobar resection due to its superior outcomes. For advanced stages, chemotherapy and radiation therapy are commonly employed. These treatments aim to reduce tumor size, alleviate symptoms, and slow disease progression. However, the aggressive nature of this carcinoma often limits the effectiveness of traditional therapies.
Palliative care for advanced cases
In advanced cases, where curative treatment is not feasible, palliative care plays a crucial role. This approach focuses on improving the quality of life by managing symptoms such as pain, breathlessness, and fatigue. Techniques like targeted radiation therapy can help relieve specific symptoms, while supportive care addresses the emotional and psychological needs of patients. Palliative care ensures that individuals with advanced basaloid squamous cell lung carcinoma receive compassionate and comprehensive support.
Emerging Therapies and Research
Advances in immunotherapy and targeted treatments
Recent advances in immunotherapy have shown promise for treating basaloid squamous cell lung carcinoma. PD-1/PD-L1 inhibitors, such as nivolumab, have demonstrated significant clinical responses in patients with this subtype. In one case, a patient treated with nivolumab experienced a marked improvement, highlighting the potential of these therapies. Tumors expressing PD-L1 and infiltrated by CD8+ T cells appear to respond particularly well to immunotherapy. These findings suggest that immunotherapy may offer longer progression-free survival compared to traditional treatments.
Ongoing clinical trials and future directions
Ongoing clinical trials continue to explore innovative approaches for managing basaloid squamous cell lung carcinoma. Researchers are investigating targeted therapies that focus on specific genetic mutations associated with this subtype. Additionally, combination therapies involving immunotherapy and chemotherapy are being evaluated for their potential to enhance treatment outcomes. These efforts aim to develop more effective strategies for combating this aggressive cancer, offering hope for improved survival rates in the future.
Basaloid squamous cell lung carcinoma stands out as an aggressive lung cancer subtype with a poor prognosis. Its high-grade nature and early metastasis make it challenging to diagnose, especially when using small biopsy samples. Morphological similarities with other high-grade carcinomas further complicate identification, even with advanced techniques like immunohistochemistry. Despite these challenges, recent advancements in research offer hope. Immunotherapy, particularly PD-1/PD-L1 inhibitors like nivolumab, has shown promise in improving outcomes. The exploration of biomarkers such as PD-L1 expression continues to pave the way for more targeted and effective treatments, offering optimism for the future.
FAQ
What makes basaloid squamous cell lung carcinoma different from other lung cancers?
Basaloid squamous cell lung carcinoma exhibits unique histological features, such as lobular growth patterns and peripheral palisading. It also has a higher rate of metastasis and worse survival outcomes compared to other lung cancer subtypes.
Can basaloid squamous cell lung carcinoma be prevented?
Reducing tobacco use significantly lowers the risk of developing this carcinoma. Avoiding exposure to environmental carcinogens and maintaining regular health check-ups may also help in early detection and prevention.
How is basaloid squamous cell lung carcinoma diagnosed?
Doctors use imaging techniques like CT scans and X-rays to identify abnormalities. A biopsy followed by histopathological analysis confirms the diagnosis. Immunohistochemistry helps differentiate it from other lung cancer subtypes.
Are there any promising treatments for this carcinoma?
Emerging therapies, such as immunotherapy with PD-1/PD-L1 inhibitors, show promise. These treatments target specific tumor markers, offering hope for improved outcomes. Ongoing clinical trials continue to explore innovative approaches.
What should patients expect during treatment?
Treatment often involves surgery, chemotherapy, or radiation therapy. In advanced cases, palliative care focuses on symptom management and quality of life. Patients should discuss options with their healthcare team to understand potential outcomes.
See Also
Essential Information on Symptoms of Adrenocortical Carcinoma
Understanding Anaplastic Large Cell Lymphoma Treatment Options
An In-Depth Overview of Various Cancer Types Available

