Why Cancer Returns After Remission Explained
Cancer recurrence can feel overwhelming, but understanding why it happens can help you navigate this challenge. Sometimes, treatments leave behind residual cancer cells that later grow into new tumors. For example:
Ovarian cancer has an 85% recurrence rate.
Bladder cancer returns in about 50% of cases after surgery.
Cancer might come back because the original treatment didn’t eliminate all cancer cells. These cells can remain dormant or resist treatment, leading to recurrence.
By learning about recurrence, you can feel more prepared to ask questions and make informed decisions. Can cancer come back after remission? Understanding recurrence is key to managing your health.
Key Takeaways
Cancer can come back after remission if some cells survive treatment. Regular doctor visits help check for signs of it returning.
Sleeping cancer cells can wake up and cause it to return. Reducing stress with mindfulness might help keep these cells asleep.
Learning about your cancer type can help you plan better with your doctor for follow-up care.
Follow-up care, like check-ups and scans, helps find returning cancer early. Early detection can lead to better treatments.
Living healthy with good food and exercise can boost your immune system. This might lower the chance of cancer coming back.
Can Cancer Come Back After Remission? Understanding Recurrence
Residual Cancer Cells
Cancer treatments aim to destroy all cancer cells, but some may survive. These residual cells are often microscopic and undetectable during follow-up tests. Over time, they can grow and form new tumors. For example, microscopic cancer cells left behind after surgery or chemotherapy may remain dormant for months or years before becoming active again. This is one reason why regular follow-up care is essential after remission.
The likelihood of recurrence depends on the cancer stage at diagnosis. Early-stage cancers have a lower recurrence rate compared to advanced stages. For instance:
Cancer Stage | Recurrence Rate |
|---|---|
Stage 1 | 5% |
Stage 2 | 12% |
Stage 3 | 33% |
Understanding the role of residual cancer cells helps you stay informed and proactive about your health.
Dormant Cancer Cells and Reactivation
Dormant cancer cells are another factor in recurrence. These cells enter a state of inactivity, where they stop dividing but remain alive. Dormancy allows them to evade treatments like chemotherapy, which targets actively dividing cells. Over time, certain triggers can reactivate these dormant cells, causing them to grow and spread.
Scientists are still studying what causes reactivation. Factors like changes in the surrounding tissue or the immune system may play a role. By understanding dormancy, researchers hope to develop treatments that prevent these cells from waking up.
The Role of Stress Hormones in Recurrence
Stress can impact your body in many ways, including cancer recurrence. Studies show that stress hormones like norepinephrine may reactivate dormant cancer cells. Research involving lung cancer patients found that higher levels of stress-related proteins, such as S100A8/A9, correlated with a greater risk of recurrence. Experiments on mice also revealed that stress hormones could stimulate tumor growth.
Managing stress is not just about emotional well-being; it may also reduce the risk of cancer returning. Techniques like mindfulness, exercise, and counseling can help you maintain a balanced state of mind. Some studies even suggest that medications like beta-blockers could block the effects of stress hormones, offering another layer of protection.
Biological Reasons for Cancer Recurrence
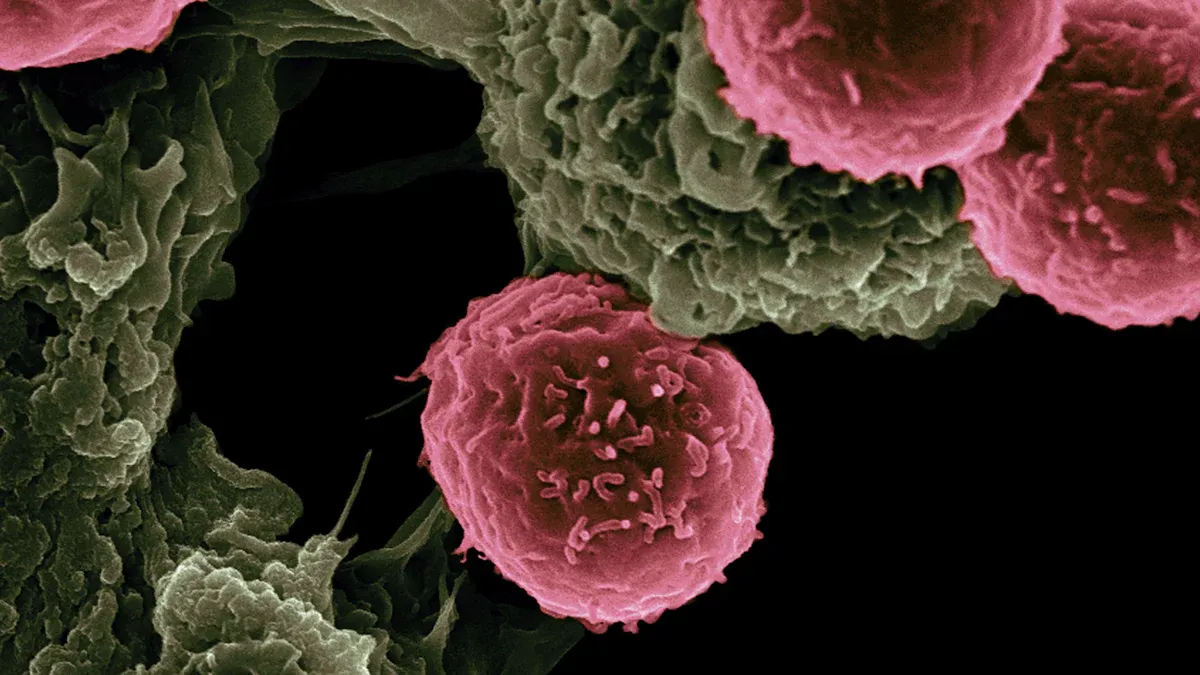
Micrometastases
Micrometastases are tiny clusters of cancer cells that spread from the original tumor to other parts of your body. These cells are often too small to detect during initial diagnosis or treatment. Over time, they can grow into new tumors, leading to recurrence. Research shows that women under 50 with locally advanced breast cancer or hormone receptor-negative breast cancer face higher risks of distant recurrence. This highlights the importance of understanding micrometastases and their role in cancer returning.
Doctors use advanced imaging and blood tests to monitor for micrometastases, but these methods have limitations. Regular follow-up care helps detect recurrence early, giving you a better chance of managing it effectively.
Cancer Cell Mutations and Aggressiveness
Cancer cells constantly change. Mutations can make them more aggressive, allowing them to resist treatments and spread faster. These changes often occur during treatment, as cancer cells adapt to survive. For example, some mutations enable cells to evade chemotherapy or radiation, making recurrence more likely.
Statistical analyses using models like the Fine–Gray method show that biological factors, including mutations, significantly impact cancer recurrence. By studying these mutations, researchers aim to develop targeted therapies that stop aggressive cancer cells from returning.
Understanding how mutations affect cancer can help you ask informed questions about your treatment options. Staying proactive about your health ensures you receive the best care possible.
Tumor Characteristics and Their Impact on Recurrence
The type of tumor you have plays a major role in recurrence rates. Tumors with certain features, like high-grade or poorly differentiated cells, are more likely to return. For example, glioblastoma has a nearly 100% recurrence rate, while ovarian cancer recurs in 85% of cases. On the other hand, cancers like estrogen receptor-positive breast cancer have lower recurrence rates, ranging from 5% to 9%.
Cancer Type | Recurrence Rate (%) |
|---|---|
Glioblastoma | Nearly 100 |
Ovarian Cancer | 85 |
Soft Tissue Sarcomas | 50 |
Bladder Cancer | 50 |
Pancreatic Cancer | 36 to 46 |
Estrogen Receptor-Positive Breast Cancer | 5 to 9 |
Knowing your tumor’s characteristics helps you understand your risk of recurrence. This knowledge empowers you to work closely with your care team to create a personalized follow-up plan.
Treatment-Related Factors
Incomplete Removal During Surgery
Surgery aims to remove all visible cancer cells, but microscopic cells can remain undetected. These residual cells may grow into new tumors over time. Factors like tumor grade and hormone receptor status influence the likelihood of recurrence. Clinical data shows that staging systems incorporating these factors provide better survival estimates than anatomical staging alone.
You can reduce the risk of recurrence by discussing surgical options thoroughly with your care team. Surgeons often use advanced imaging techniques to identify and remove as much of the tumor as possible. However, follow-up treatments like chemotherapy or radiation may still be necessary to target any remaining cells.
Limitations of Chemotherapy and Radiotherapy
Chemotherapy and radiotherapy are powerful tools, but they have limitations. Not all cancer cells divide simultaneously, so some may survive chemotherapy. Radiotherapy damages DNA in cancer cells, but if even a few cells recover, they can regrow. Dormant cancer cells also evade these treatments, later becoming active and contributing to recurrence.
Missed radiation therapy sessions increase the risk of recurrence by allowing remaining cancer cells to divide faster. Local treatments like surgery and radiation may not address cancer cells that spread beyond the treatment area. These limitations highlight the importance of combining therapies and maintaining consistent treatment schedules.
Chemotherapy targets dividing cells but leaves dormant ones untouched.
Radiotherapy can fail to kill all cancer cells, allowing regrowth.
Cancer cells outside the treatment area may escape local therapies.
Understanding these challenges helps you stay proactive about your treatment plan.
The Role of the Immune System in Preventing Recurrence
Your immune system plays a critical role in preventing cancer recurrence. Tumor-reactive immune cells protect against metastatic tumors and keep dormant cancer cells inactive. Chronic inflammation, however, can trigger DNA mutations and epigenetic changes, increasing the risk of recurrence.
Certain markers, like CRP and IL-6, help predict recurrence and survival outcomes. High levels of inflammatory cytokines correlate with recurrence in breast cancer patients. CD8+ T cells also exert a cytostatic effect, maintaining cancer cells in a dormant state.
Evidence Type | Findings |
|---|---|
Tumor-reactive immune cells | Protect against metastatic tumors and induce immunoediting of dormant cells. |
Serum inflammatory cytokines | High levels correlate with recurrence in breast cancer patients. |
CRP and IL-6 | Serve as prognostic markers for recurrence and survival. |
Chronic inflammation | Induces DNA mutations and epigenetic changes, facilitating carcinogenesis. |
CD8+ T cells | Maintain cancer cells in a dormant state. |
Strengthening your immune system through a healthy lifestyle and targeted therapies can reduce recurrence risks. Discuss immunotherapy options with your doctor to explore how your immune system can fight cancer effectively.
Types of Cancer Recurrence
Local Recurrence
Local recurrence happens when cancer returns to the same area where it was first detected. This type of recurrence often occurs because some cancer cells remain in the original site after treatment. These cells may grow over time, forming a new tumor. For example, bladder cancer has a 50% recurrence rate after cystectomy, while breast cancer recurrence ranges from 5% to 30%, depending on the treatment used.
Cancer Type | Recurrence Rate |
|---|---|
Bladder | 50% after cystectomy |
Breast | 30% overall, 5% to 9% with letrozole or placebo |
Colorectal | 17% after curative surgical resection |
Glioblastoma | Nearly 100% |
Hodgkin lymphoma | 10% to 13% after primary treatment, 20% to 50% after second-line treatment |
Kidney | 13% after complete response to tyrosine kinase inhibitor therapy |
11%-12% local recurrence | |
Prostate | 24% low-risk disease, 40% intermediate-risk disease, 48% high-risk disease |
Thyroid | Up to 30% for differentiated thyroid carcinoma |
Regular follow-up care and imaging tests can help detect local recurrence early. Early detection improves the chances of successful treatment.
Regional Recurrence
Regional recurrence occurs when cancer spreads to nearby lymph nodes or tissues close to the original tumor. This type of recurrence often signals that cancer cells have moved beyond the initial site but remain within the same general area. Studies show that recurrence rates were higher in older studies with longer follow-up periods, but modern treatments have improved outcomes.
Evidence Type | Findings |
|---|---|
Recurrence Rates | Higher in studies from before 2000, especially with 5-9 years follow-up |
Treatment Improvements | Recent studies show better outcomes due to evidence-based treatment guidelines |
Regional Variations | Lower recurrence in regions with early diagnosis and better treatment access |
Ethnic Disparities | African-American women have a higher risk of recurrence compared to other populations |
You can reduce the risk of regional recurrence by following your doctor’s treatment plan and attending regular check-ups. Early diagnosis and access to advanced treatments also play a significant role in improving outcomes.
Distant Recurrence (Metastasis)
Distant recurrence, also known as metastasis, happens when cancer spreads to other parts of the body, such as the lungs, liver, or bones. This type of recurrence is more challenging to treat and often occurs years after the initial diagnosis. Research shows that 22.2% of women experienced distant recurrence within 14 years of follow-up, while pooled estimates suggest a 23.3% rate after 10 years. Younger women with locally advanced or hormone receptor-negative breast cancer face higher risks.
Study | Findings |
|---|---|
Australian Study | 22.2% of women had distant recurrence within 14 years of follow-up. |
Pooled Estimate | 23.3% observed after 10 years median follow-up. |
Incidence Decline | Distant recurrence incidence declined over time with new adjuvant therapies. |
Higher Proportions | Higher rates in women diagnosed under 50, with locally advanced disease, and HR negative breast cancer. |
Understanding the risk factors for distant recurrence can help you make informed decisions about long-term care. Advances in treatment, such as targeted therapies, offer hope for managing metastatic cancer effectively.
Managing Cancer Recurrence
Medical Treatment Options
When cancer returns, medical treatments focus on controlling its spread and improving your quality of life. Options include surgery, chemotherapy, radiation, and targeted therapies. Each treatment depends on the type of cancer and its recurrence pattern. For example, bladder cancer has a 50% recurrence rate after cystectomy, while ovarian cancer recurs in 85% of cases. Understanding these rates helps you make informed decisions about your care.
Cancer Type | Recurrence Rate |
|---|---|
Bladder | 50% after cystectomy |
Breast | 30% overall, 5% to 9% with letrozole or placebo |
Glioblastoma | Nearly 100% |
Ovarian | 85% |
Soft Tissue Sarcoma | 50% after adjuvant chemotherapy, nearly 100% for advanced disease |
Advances in targeted therapies and immunotherapy offer hope for managing recurrence. These treatments focus on specific cancer cells, reducing side effects and improving outcomes. Discussing these options with your doctor ensures you receive the most effective care.
Emotional Coping Strategies
Facing cancer recurrence can feel overwhelming. Emotional coping strategies help you manage stress and maintain a positive outlook. Studies show that tailored psychotherapy significantly reduces depression symptoms in patients with advanced cancer. Mindfulness-based cognitive therapy also improves quality of life and reduces psychological distress.
A clinical trial found that psychotherapy tailored to cancer patients lowered depression symptoms.
Another study showed mindfulness-based therapy reduced distress and improved well-being.
Incorporating techniques like meditation, journaling, or joining support groups can provide emotional relief. These strategies not only improve your mental health but may also enhance your ability to cope with treatment.
The Importance of Follow-Up Care
Follow-up care plays a vital role in detecting recurrence early. Regular appointments, including physical exams and imaging tests, increase the chances of successful treatment. Screening programs and early detection campaigns have shifted cancer stages, allowing for more curative treatments and better survival rates.
Regular follow-ups with imaging tests improve early detection and treatment success.
Screening programs have increased curative treatment opportunities, enhancing survival rates.
Staying consistent with follow-up care ensures that any signs of recurrence are addressed promptly. This proactive approach gives you the best chance of managing your health effectively.
Cancer recurrence can feel overwhelming, but understanding its causes helps you prepare for the journey ahead. Advances in treatment and follow-up care offer hope for managing recurrence more effectively. Emotional support plays a critical role in this process:
About 7% of patients experience severe fear of recurrence, leading to intrusive thoughts.
Discussing recurrence risks with your care team can ease fears and improve your quality of life.
A strong support system and proactive care empower you to face challenges with confidence and resilience.
FAQ
What are the chances of cancer coming back after remission?
The chances depend on the type and stage of cancer. For example, early-stage cancers have lower recurrence rates, while advanced stages or aggressive cancers like glioblastoma have higher rates. Regular follow-ups and personalized care plans help you monitor and manage these risks effectively.
Can lifestyle changes reduce the risk of recurrence?
Yes, adopting healthy habits can help. Eating a balanced diet, exercising regularly, and managing stress strengthen your immune system. These changes may lower inflammation and improve your overall health, reducing the likelihood of cancer returning.
Tip: Consult your doctor before making significant lifestyle changes to ensure they align with your treatment plan.
How does stress affect cancer recurrence?
Stress hormones like norepinephrine can reactivate dormant cancer cells. Chronic stress weakens your immune system, making it harder to fight off recurrence. Practicing mindfulness, exercising, or seeking therapy can help you manage stress and maintain emotional balance.
Is recurrence always more aggressive than the original cancer?
Not always. Some recurrences may grow slowly, while others become more aggressive due to mutations. Your doctor will assess the recurrence's characteristics and recommend treatments tailored to your situation.
What should you do if you suspect cancer has returned?
Contact your doctor immediately if you notice unusual symptoms like persistent pain, unexplained weight loss, or fatigue. Early detection improves treatment outcomes. Regular follow-ups and open communication with your care team are essential for managing your health proactively.
Note: Never ignore symptoms, even if they seem minor. Early action can make a significant difference.
See Also
Understanding Carcinoid Tumors: Essential Information You Need
Key Characteristics of Glioblastoma: A Comprehensive Overview
Exploring Hemangioblastoma: Important Features You Should Know
Recognizing Duodenal Cancer: Symptoms and Treatment Options Explained

