Can a Tumor Be Diagnosed as Cancerous by Visual Inspection
You cannot determine if a tumor is cancerous just by looking at it. While some tumors may appear suspicious, visual inspection often leads to inconsistent results. For example:
A study found a 73% difference in tumor assessments among readers, showing how subjective visual evaluations can be.
Clinical trials revealed that expertise levels significantly influence tumor evaluations, leading to variability in results.
Many lesions are classified as non-measurable, making it harder to rely on visual inspection alone.
These findings highlight the need for further diagnostic tests. A professional medical evaluation ensures accurate diagnosis and effective treatment planning. Can you tell if a tumor is cancerous just by looking at it? The answer is no; further testing is essential for a definitive diagnosis.
Key Takeaways
You can't tell if a tumor is cancerous by looking. Always get more tests to know for sure.
Using tests like biopsies, scans, and lab checks helps find the truth and avoids mistakes.
Finding cancer early makes treatment work better. Regular check-ups are very important.
A group of doctors working together gives a full review and better treatment choices.
Watch for signs like lumps that don't go away or changes in growths. See a doctor if something seems wrong.
Can You Tell If a Tumor Is Cancerous Just by Looking at It?

Why Visual Inspection Is Insufficient
Overlapping features of benign and malignant tumors
You cannot rely on visual inspection alone to determine if a tumor is cancerous. Benign and malignant tumors often share similar appearances, making it difficult to distinguish between them. For example, both types can present as lumps or growths with irregular shapes. Even experienced professionals may struggle to differentiate them without additional tests. A table summarizing key findings highlights these challenges:
Evidence Description | Key Findings |
|---|---|
Variability in detecting new lesions and the impact of non-measurable lesions on adjudication rates. | |
Role of non-target lesions | Non-target lesions accounted for over 10% of adjudications, showing their significance. |
RECIST 1.1 guidelines | Guidelines address some issues but emphasize the need for standardization. |
This variability underscores why visual inspection cannot provide a definitive diagnosis.
Variability in tumor appearance based on location and type
Tumors can look different depending on their location and type. For instance, a tumor in the breast may feel firm and immovable, while one in the skin might appear as a discolored patch. These differences add another layer of complexity. Diagnostic accuracy improves significantly when additional tests are used. For example, high b-value DWI imaging for prostate cancer detection has a sensitivity of 85% and a specificity of 89%. This demonstrates how advanced techniques outperform visual evaluations.
Exceptions in Certain Cases
Skin cancer and the role of clinical examination
In some cases, visual inspection plays a more significant role. Skin cancer, for example, often presents visible signs like asymmetry, irregular borders, or changes in color. Dermatologists use these clues during clinical examinations to identify suspicious lesions. However, even in these cases, biopsies remain essential for confirmation.
Limitations even in visible tumors
Even when tumors are visible, relying solely on appearance can lead to errors. Non-cancerous growths like moles or cysts can mimic cancerous lesions. Without further testing, you risk misdiagnosis. Combining visual inspection with diagnostic tools ensures a more accurate evaluation.
Diagnostic Methods to Confirm If a Tumor Is Cancerous
Biopsy: The Gold Standard
Procedure and analysis
A biopsy involves removing a small sample of tissue from the tumor for laboratory analysis. This procedure can be performed using a needle or through surgery, depending on the tumor's location and size. Pathologists examine the sample under a microscope to identify cancerous cells. They may also perform additional tests to determine the tumor's type and grade. This detailed analysis provides critical information about the tumor's behavior and potential treatment options.
Why biopsies are definitive
Biopsies are considered the most reliable method for diagnosing cancer. Clinical trials have shown high success rates for this technique. For example, needle biopsies detect cancer in 60% to 90% of cases, while surgical biopsies achieve an accuracy rate of 80% to 98%. These statistics highlight why biopsies remain the gold standard for confirming if a tumor is cancerous.
Biopsy Method | Cancer Detection Rate (%) |
|---|---|
Needle Biopsies | 60% - 90% |
Surgical Biopsies | 80% - 98% |
Imaging Techniques
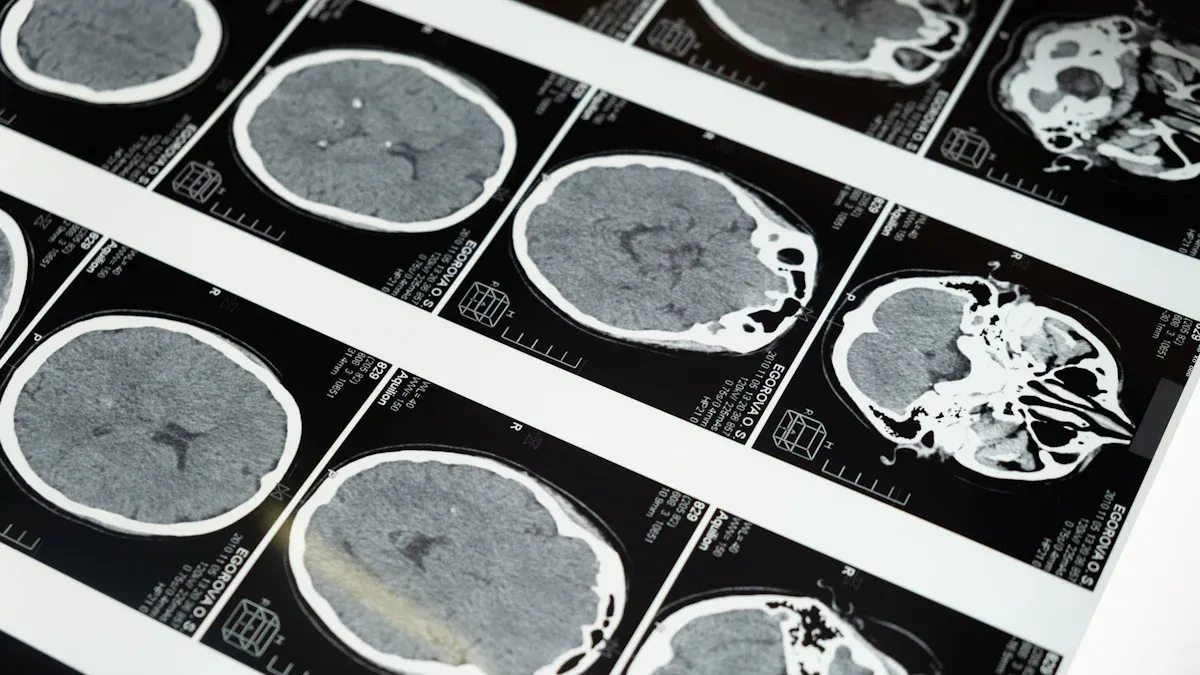
CT scans, MRIs, and ultrasounds
Imaging techniques like CT scans, MRIs, and ultrasounds play a vital role in diagnosing cancer. CT scans provide detailed images of internal organs, helping doctors locate tumors. MRIs are particularly effective for detecting soft tissue tumors, offering high-resolution images. Ultrasounds use sound waves to create images, often used for breast or abdominal tumors. These methods allow doctors to assess the tumor's size, shape, and location.
How imaging supports diagnosis but has limitations
While imaging techniques are valuable, they have limitations. For instance, MRIs excel at detecting soft tissue tumors but may not work well for blood or bone cancers. CT scans are quick and effective but expose patients to radiation. Combining imaging with other diagnostic methods improves accuracy. Studies show that pooled sensitivity and specificity metrics from combined approaches outperform visual inspection alone. Positive likelihood ratios (PLR) and diagnostic odds ratios (DOR) further confirm the superiority of these methods.
Imaging Technique | Strengths | Limitations |
|---|---|---|
MRI | Effective in detecting soft tissue tumors, detailed images, useful for staging cancer | Not effective for blood or bone cancers, possible false negatives |
CT Scan | Good for visualizing tumors in various organs, quick imaging | May not provide as detailed images of soft tissue as MRIs, potential radiation exposure |
Molecular and Genetic Testing
Identifying cancer markers
Molecular and genetic testing identifies specific mutations or markers in cancer cells. These tests analyze the tumor's DNA to detect abnormalities that drive cancer growth. For example, in non-small cell lung cancer, testing for EGFR mutations has led to targeted therapies that improve survival rates. Similarly, identifying the HER2 gene in breast cancer has enabled the use of effective treatments like trastuzumab.
Role in personalized treatment planning
These tests play a crucial role in personalized treatment planning. By understanding the tumor's genetic profile, doctors can recommend therapies tailored to your specific condition. Advances in immunotherapy, such as checkpoint inhibitors and CAR T-cell therapy, have further enhanced treatment options. Molecular profiling ensures that you receive the most effective and targeted care, improving outcomes and reducing unnecessary treatments.
Molecular profiling enables tailored therapies, improving treatment outcomes.
Genetic testing for EGFR mutations in lung cancer has led to targeted therapies like erlotinib.
HER2 identification in breast cancer allows for effective treatments like trastuzumab.
Immunotherapy advancements, including CAR T-cell therapy, show promise in various cancers.
The Importance of Combining Diagnostic Approaches
Enhancing Diagnostic Accuracy
Benefits of integrating biopsy, imaging, and molecular tests
Combining diagnostic methods like biopsies, imaging, and molecular testing significantly improves accuracy. Each approach provides unique insights into the tumor's characteristics. For example, a biopsy confirms the presence of cancerous cells, while imaging reveals the tumor's size and location. Molecular testing identifies genetic markers that guide treatment. Together, these methods create a complete picture of the tumor, reducing uncertainty. This integration strengthens diagnostic systems and ensures timely and precise results. Surveillance of diagnostic processes also helps identify and correct errors, improving outcomes over time.
Reducing the risk of misdiagnosis
Using multiple diagnostic tools minimizes the chances of misdiagnosis. A single method may miss critical details, but combining approaches fills these gaps. For instance, imaging might detect a suspicious mass, but only a biopsy can confirm if it is cancerous. Diagnostic stewardship, which involves evidence-based testing, further enhances accuracy. Collaboration with laboratory professionals has been shown to reduce misdiagnosis rates by up to 50%, particularly in complex cases. This approach ensures you receive the right diagnosis and appropriate care.
Multidisciplinary Collaboration
Role of oncologists, radiologists, and pathologists
A team of specialists plays a vital role in diagnosing cancer. Oncologists focus on cancer treatment, radiologists interpret imaging results, and pathologists analyze biopsy samples. These experts work together to share findings and develop a comprehensive diagnosis. This collaboration ensures no detail is overlooked, leading to better treatment decisions. By pooling their expertise, they enhance the reliability of the diagnostic process.
Comprehensive evaluation for effective treatment
A multidisciplinary approach ensures a thorough evaluation of your condition. Each specialist contributes their knowledge to create a personalized treatment plan. For example, radiologists may identify the tumor's location, while pathologists determine its type. Oncologists then use this information to recommend targeted therapies. This teamwork improves your chances of successful treatment and recovery. Multidisciplinary collaboration also emphasizes diagnostic safety, helping healthcare teams learn from mistakes and refine their processes.
When to Seek Medical Attention
Recognizing Warning Signs
Persistent lumps or growths
You should pay attention to any lump or growth that does not go away. Hard lumps that appear suddenly or grow over time could indicate a serious issue. These lumps may feel firm or immovable, which often raises concern. If you notice a lump that persists for more than two weeks, it is essential to consult a doctor. Early evaluation can help determine whether the growth is benign or requires further investigation.
Changes in size, shape, or color of a tumor
Tumors that change in size, shape, or color may signal a problem. For example, a mole that becomes asymmetrical, develops irregular borders, or changes color could indicate skin cancer. These changes often occur gradually, so monitoring your body for any noticeable differences is crucial. If you observe such changes, seek medical advice promptly to rule out potential risks.
Other warning signs that should prompt immediate attention include:
Unexplained weight loss or unusual bleeding.
Changes in bowel or bladder habits.
Symptoms like sharp chest pain, trouble breathing, or drenching night sweats.
Importance of Early Detection
How early diagnosis improves outcomes
Detecting cancer early can save lives. Studies show that early diagnosis significantly improves survival rates. When cancer is caught in its initial stages, treatment is often more effective and less invasive. Early intervention can also prevent the disease from spreading, reducing its lethality. The World Health Organization emphasizes that early diagnosis leads to better outcomes and improved quality of life for patients.
Encouraging regular screenings and check-ups
Regular screenings play a vital role in catching cancer early. Many cancers, such as breast, cervical, and colorectal, can be detected through routine tests. These screenings allow doctors to identify abnormalities before symptoms appear. Programs promoting early detection have reduced mortality rates and improved access to timely care. By scheduling regular check-ups, you take an active step toward protecting your health and ensuring better treatment options if needed.
Tip: Pay attention to your body and schedule regular screenings. Early action can make a significant difference in your health outcomes.
You cannot rely on visual inspection alone to determine if a tumor is cancerous. Accurate diagnosis requires advanced tools like biopsies, imaging, and molecular testing. Each method provides unique insights, and combining them ensures reliability while reducing errors. The diagnostic process often spans multiple settings, from home to healthcare facilities, emphasizing the need for a comprehensive approach. Collaboration among specialists, such as oncologists and radiologists, plays a vital role in achieving diagnostic accuracy. Early detection through professional evaluation improves outcomes and ensures you receive the most effective treatment.
Note: A multidisciplinary approach enhances diagnostic precision and supports better care.
FAQ
What are the common signs that a tumor might be cancerous?
Cancerous tumors often grow quickly, feel firm, and may cause pain or discomfort. You might notice changes in size, shape, or color. Symptoms like unexplained weight loss, fatigue, or persistent cough could also indicate cancer. Always consult a doctor for proper evaluation.
Can imaging tests alone confirm if a tumor is cancerous?
No, imaging tests like CT scans or MRIs can only suggest if a tumor looks suspicious. You need a biopsy to confirm if it is cancerous. Imaging helps locate and assess the tumor but cannot provide a definitive diagnosis.
How long does it take to get biopsy results?
Biopsy results usually take a few days to a week. The exact time depends on the type of biopsy and the complexity of the analysis. Your doctor will inform you about the expected timeline and next steps.
Are all tumors cancerous?
No, not all tumors are cancerous. Many are benign, meaning they do not spread or pose a serious threat. However, only a medical evaluation can determine if a tumor is benign or malignant. Always seek professional advice if you notice unusual growths.
Is early detection of cancer always possible?
Early detection is possible for many cancers through regular screenings and check-ups. However, some cancers may not show symptoms until later stages. Paying attention to warning signs and scheduling routine tests can improve your chances of early diagnosis.
Tip: Stay proactive about your health. Regular screenings and prompt medical attention can make a significant difference.
See Also
Exploring Bone Cancer: Malignant Fibrous Histiocytoma and Osteosarcoma
Recognizing Endodermal Sinus Tumors: Key Symptoms and Diagnosis
Conjunctival Melanoma: Symptoms You Should Be Aware Of
Anal Cancer: Key Symptoms and Causes You Need To Know
Carcinoid Tumors: Essential Information You Need To Understand

