What is Cancer Immunotherapy and How Does it Work
Cancer immunotherapy uses your immune system to fight cancer. It trains your body’s natural defenses to recognize and destroy harmful cancer cells. Unlike traditional treatments, immunotherapy boosts your immune system’s ability to target cancer more effectively.
Recent breakthroughs highlight its success in improving survival rates. For example:
In advanced melanoma, immunotherapy increases five-year survival rates to 30-40%, compared to less than one year with chemotherapy.
For lung cancer, pembrolizumab extends survival to 30 months, while chemotherapy offers only 10-12 months.
In triple-negative breast cancer, combining immunotherapy with chemotherapy improves survival to 25 months in PD-L1-positive tumors.
Exploring Immunotherapy: The New Frontier in Cancer Treatment has opened doors to more personalized and effective cancer care.
Key Takeaways
Cancer immunotherapy helps your body fight cancer using its immune system. It is more focused than older treatments.
Medicines like checkpoint inhibitors and CAR T-cell therapy work well. They have helped many people live longer with different cancers.
Immunotherapy can teach your immune system to remember cancer cells. This helps stop cancer from coming back for a long time.
Even though immunotherapy has good results, it may cause side effects. Talk to your doctor to see if it’s right for you.
Scientists are working to make immunotherapy help more people. They also want to make it easier for everyone to get these treatments.
How the Immune System Interacts with Cancer
The Role of the Immune System in Fighting Cancer
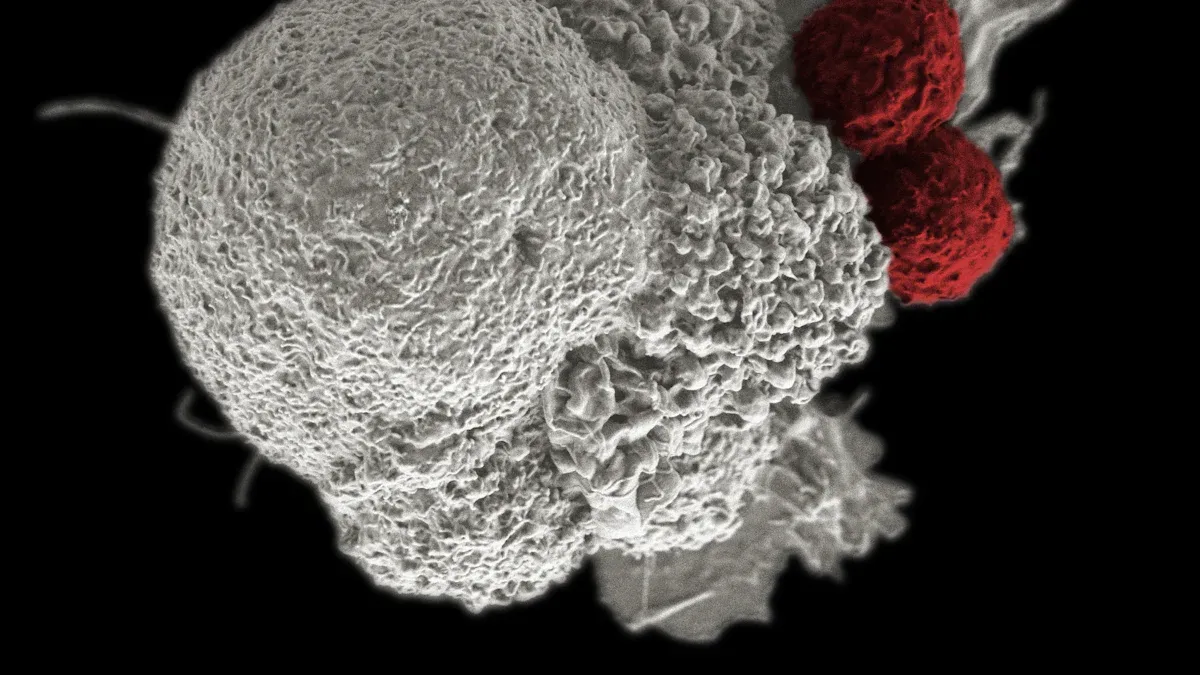
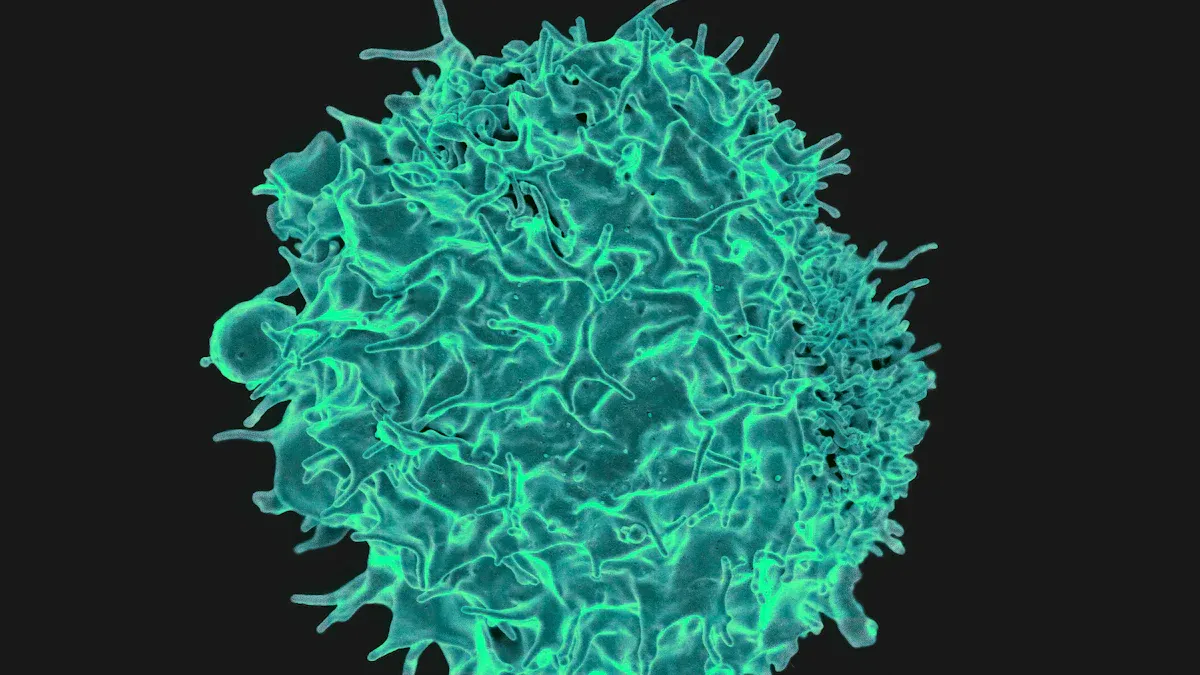
Your immune system acts as your body’s defense mechanism. It identifies and destroys harmful invaders like bacteria, viruses, and abnormal cells, including cancer cells. Specialized immune cells, such as T-cells and natural killer (NK) cells, play a critical role in this process. They patrol your body, searching for cells that appear abnormal or foreign. When they detect cancer cells, they attack and destroy them to prevent further growth.
Historical observations also highlight the immune system’s potential in fighting cancer. In the late 19th century, William B. Coley injected bacteria into cancer patients and observed tumor shrinkage in some cases. This discovery demonstrated how activating the immune system could help combat cancer.
Challenges the Immune System Faces with Cancer
Cancer cells often create unique challenges for your immune system. They can alter their surface proteins, making it harder for immune cells to recognize them. Some cancer cells release substances that suppress immune responses, effectively hiding from detection. These mechanisms allow tumors to grow unchecked.
Research shows that tumor mutations can sometimes work in your favor. Mutated proteins on cancer cells can make them appear foreign, helping immune cells identify and attack them. This is why patients with highly mutated tumors often respond better to immunotherapy. However, not all tumors exhibit these mutations, which complicates treatment.
How Cancer Evades Immune Detection
Cancer cells have developed clever ways to evade your immune system. They can disguise themselves by changing their surface markers, which are essential for immune recognition. Some tumors even produce chemicals that weaken immune cells or block their activity. These tactics allow cancer to grow and spread without interference.
Advanced research has provided tools to study these interactions. A 3D co-culture model, for example, helps scientists analyze how immune cells infiltrate tumors and impact their growth. This model enhances our understanding of immune-tumor dynamics and aids in designing better immunotherapies.
Exploring Immunotherapy: The New Frontier in Cancer Treatment
Checkpoint Inhibitors
Checkpoint inhibitors help your immune system recognize and attack cancer cells. Normally, your immune system uses checkpoints to avoid attacking healthy cells. Cancer cells exploit these checkpoints to hide from immune attacks. Checkpoint inhibitors block this process, allowing your immune cells to target cancer effectively.
For example, pembrolizumab, a checkpoint inhibitor, has transformed survival rates for advanced non-small cell lung cancer (NSCLC). In a clinical trial, 23% of patients lived for five or more years, compared to the historical survival rate of just 5%. This demonstrates how checkpoint inhibitors can significantly improve outcomes for cancers with poor prognoses.
CAR T-Cell Therapy
CAR T-cell therapy is a groundbreaking treatment that uses your own immune cells to fight cancer. Doctors collect your T-cells, modify them in a lab to better recognize cancer, and then return them to your body. These enhanced T-cells actively seek and destroy cancer cells.
This therapy has shown remarkable success in treating blood cancers. For instance, tisagenlecleucel, the first FDA-approved CAR T-cell therapy, achieved remission rates of over 80% in patients with B-cell acute lymphoblastic leukemia. Similarly, axicabtagene ciloleucel improved survival rates for patients with large B-cell lymphoma. These results highlight the potential of CAR T-cell therapy to revolutionize cancer treatment.
Monoclonal Antibodies
Monoclonal antibodies are lab-made proteins designed to target specific markers on cancer cells. They act like homing missiles, flagging cancer cells for destruction by your immune system. This precision makes them highly effective in treating certain cancers.
One example is dinutuximab, which targets the GD2 protein found on neuroblastoma cells. By binding to this protein, it helps your immune system eliminate cancer cells. This approach has extended the lives of many children with high-risk neuroblastoma, showcasing the power of monoclonal antibodies in improving outcomes for difficult-to-treat cancers.
Cancer Vaccines
Cancer vaccines train your immune system to recognize and attack cancer cells. Unlike traditional vaccines that prevent diseases, these vaccines treat existing cancers or reduce the risk of recurrence. They work by introducing antigens—proteins found on cancer cells—into your body. This triggers an immune response, helping your immune system target and destroy cancer cells more effectively.
Recent advancements in mRNA-based cancer vaccines have shown promising results. These vaccines can be tailored to your tumor’s unique profile, making them highly personalized. They also address tumor heterogeneity by inducing responses to multiple targets. Rapid production allows for timely updates based on tumor monitoring, ensuring the vaccine remains effective as your cancer evolves.
Here are some key findings from recent studies:
Study Focus | Vaccine Type | Outcome |
|---|---|---|
Pancreatic Cancer | mRNA-based | 50% of patients showed immune response; no signs of cancer at 18-month follow-up. |
Metastatic Melanoma | mRNA-based + ICI | 44% reduction in cancer recurrence or death compared to standard treatment. |
General Cancer Types | mRNA-based | Early studies show encouraging results for various cancers, indicating potential effectiveness. |
These results highlight the growing potential of cancer vaccines in modern therapeutics. By combining vaccines with other immunotherapies, such as checkpoint inhibitors, researchers are exploring immunotherapy: the new frontier in cancer treatment.
Cytokine Therapy
Cytokine therapy uses proteins called cytokines to boost your immune system’s ability to fight cancer. Cytokines act as messengers, helping immune cells communicate and coordinate their attack on cancer cells. This therapy enhances the activity of T-cells and natural killer (NK) cells, which are crucial for destroying tumors.
Two common types of cytokines used in cancer treatment are interleukins and interferons. Interleukins stimulate the growth and activity of immune cells, while interferons slow cancer cell growth and enhance immune responses. For example, interleukin-2 (IL-2) has been effective in treating advanced melanoma and kidney cancer. It activates T-cells, enabling them to target and kill cancer cells more efficiently.
Cytokine therapy often works best when combined with other treatments. Researchers are exploring immunotherapy: the new frontier in cancer treatment, to determine how cytokines can enhance the effectiveness of therapies like CAR T-cell therapy and monoclonal antibodies. While cytokine therapy shows promise, it can cause side effects such as flu-like symptoms or fatigue. Your doctor will carefully evaluate your suitability for this treatment.
Benefits and Risks of Cancer Immunotherapy
Advantages Over Traditional Cancer Treatments
Cancer immunotherapy offers several advantages compared to traditional treatments like chemotherapy and radiation. It can work across various cancer types and provides a more tailored approach by enabling your immune system to specifically target cancer cells. This precision often results in fewer side effects than chemotherapy, which affects both healthy and cancerous cells.
Immunotherapy also holds the potential for long-term remission. It trains your immune system to "remember" cancer cells, reducing the chances of recurrence. For example, clinical studies show that responses to immunotherapy can persist even after treatment ends. Additionally, immunotherapy has proven effective in treating cancers resistant to conventional therapies, such as melanoma.
Here’s a comparison of immunotherapy and chemotherapy:
Treatment Type | Success Rates | Common Side Effects | Cost Range |
|---|---|---|---|
Chemotherapy | 10-20% response for advanced melanoma; less than one year median survival | Nausea, hair loss, immune suppression, fatigue | $10,000 - $50,000 |
Immunotherapy | 30-40% response for advanced melanoma; five-year survival rates of 30-40% | Fatigue, skin reactions, autoimmune responses | $100,000 - $200,000 |
Common Side Effects of Immunotherapy
While immunotherapy offers many benefits, it can cause side effects. Common reactions include fatigue, skin irritation, and flu-like symptoms. Some patients experience more severe effects, such as autoimmune responses where the immune system attacks healthy tissues.
CAR T-cell therapy may lead to cytokine release syndrome, causing fever, low blood pressure, and rash. Neurological symptoms like confusion or tremors can also occur. Statistically, gastrointestinal side effects often appear within six weeks of treatment, while liver-related issues may last up to five weeks.
Cancer Type | P-value (Chemotherapy) | P-value (Targeted Therapy) |
|---|---|---|
Head and Neck | < 0.0001 | < 0.0001 |
Melanoma | < 0.0001 | N/A |
Renal Cancer | < 0.0001 | < 0.0001 |
Determining Suitability for Immunotherapy
Not everyone is a candidate for immunotherapy. Doctors evaluate several factors to determine if it’s right for you. These include the type and stage of your cancer, previous treatments, and specific biomarkers like PD-L1 protein. Tests on your cancer cells or blood samples help predict how well you might respond to treatment.
Criteria | Description |
|---|---|
Biomarkers | Presence of specific biomarkers like PD-L1 protein to assess response to immunotherapy. |
Type of Cancer | The specific type of cancer being treated influences the suitability for immunotherapy. |
Stage of Cancer | The extent to which cancer has spread is a critical factor in determining treatment options. |
By considering these factors, your doctor can recommend the most effective treatment plan for your condition.
Current Research and Future Potential
Emerging Therapies and Innovations
Cancer immunotherapy continues to evolve with groundbreaking advancements. Researchers are developing new therapies to improve treatment outcomes and address limitations. Some of the most promising innovations include:
Adoptive Cell Therapy (ACT): Scientists are engineering T cells with T-cell receptors (TCRs) to target mutations in cancer-driving genes like KRAS. This approach enhances the immune system's ability to attack tumors more effectively.
Combination Therapies: Integrating immunotherapy with molecularly targeted therapy or radiotherapy is showing promise in overcoming tumor resistance. These combinations aim to enhance the effectiveness of treatments while reducing the likelihood of cancer recurrence.
mRNA-Based Cancer Vaccines: Building on the success of COVID-19 vaccines, researchers are creating mRNA vaccines tailored to specific tumors. These vaccines train your immune system to recognize and destroy cancer cells, offering a personalized approach to treatment.
These innovations highlight the potential of immunotherapy to transform cancer care, making treatments more precise and effective.
Expanding Applications Across Cancer Types
Immunotherapy is no longer limited to a few cancer types. Its applications are expanding rapidly, offering hope to patients with various forms of cancer. The table below illustrates its effectiveness compared to chemotherapy and targeted therapy across different cancers:
Cancer Type | Chemotherapy P-value | Targeted Therapy P-value |
|---|---|---|
Head and Neck Cancers | < 0.0001 | |
Melanoma | < 0.0001 | N/A |
Renal Cancer | < 0.0001 | < 0.0001 |
Lung Cancer | < 0.0001 | < 0.0001 |
Basal Cell Carcinoma | < 0.0001 | N/A |
Squamous Cell Carcinoma | < 0.0001 | 0.0396 |
Brain Cancer | 0.0005 | 0.0027 |
These statistics demonstrate the growing impact of immunotherapy across diverse cancer types. However, you should be aware that immunotherapy may increase the risk of autoimmune side effects compared to other treatments.
Challenges in Advancing Immunotherapy
Despite its potential, immunotherapy faces significant challenges. Access to treatment remains a major issue due to socioeconomic and geographic disparities. For example:
Patients with lower income or education levels are less likely to receive immunotherapy for advanced-stage cancers.
Many states lack clinical trial openings for CAR T-cell therapy, particularly in regions with higher Black populations.
Underrepresentation in clinical trials is another concern. Only 2-5% of participants in pivotal CAR T-cell therapy trials for acute lymphoblastic leukemia (ALL) were Black.
Additionally, biomarkers like PD-L1, used to predict treatment responses, can vary over time, complicating treatment decisions. High costs and the need for specialized healthcare facilities further limit access. Addressing these barriers is essential to ensure equitable access to life-saving therapies.
Cancer immunotherapy is revolutionizing how you fight cancer. It offers hope where traditional treatments fall short. For example:
Atezolizumab and pembrolizumab achieve response rates of 15-25% in advanced bladder cancer.
Responders can experience survival rates of up to 21 months, as shown in studies like Powles et al. (2018).
Ongoing research ensures these breakthroughs benefit everyone. Disparities in access and tumor mutational differences across ancestries highlight the need for further studies.
Evidence Type | Description |
|---|---|
Disparities in Research | Evaluating safety and efficacy across diverse populations remains critical. |
Barriers to Access | Socioeconomic factors limit equitable access to life-saving therapies. |
Your support for research fuels the promise of better outcomes for all.
FAQ
What types of cancer can immunotherapy treat?
Immunotherapy treats many cancers, including melanoma, lung, bladder, and kidney cancers. Researchers are expanding its use to other types, such as breast and pancreatic cancers. Your doctor will determine if immunotherapy suits your specific cancer type.
How long does immunotherapy take to work?
The time varies. Some patients see results within weeks, while others may take months. Your response depends on factors like cancer type, treatment method, and overall health. Regular monitoring helps track progress.
Can immunotherapy cure cancer?
Immunotherapy can lead to long-term remission in some cases, but it doesn’t guarantee a cure. It works best for certain cancers and may reduce recurrence risks. Your doctor will discuss realistic expectations based on your condition.
Is immunotherapy safe for everyone?
Not everyone qualifies for immunotherapy. Doctors evaluate factors like cancer type, stage, and biomarkers. Some patients may experience severe side effects, so suitability depends on your overall health and medical history.
How much does immunotherapy cost?
Immunotherapy costs range from $100,000 to $200,000 per year. Insurance may cover part of the expense, but coverage varies. Financial assistance programs can help reduce costs. Discuss options with your healthcare provider.
💡 Tip: Ask your doctor about clinical trials. They often provide access to cutting-edge treatments at reduced costs.
See Also
Understanding Choriocarcinoma: Symptoms and Treatment Options
Recognizing Angioimmunoblastic T-Cell Lymphoma Symptoms and Signs
Anaplastic Large Cell Lymphoma: Overview and Treatment Approaches
Exploring Cancer Types Associated with AIDS: A Comprehensive Guide

