Cancer is caused by stress? Find out why

Cancer is caused by stress? While stress doesn’t directly cause cancer, it can create conditions that make your body more susceptible. Chronic stress weakens your immune system, making it harder to combat illnesses. Additionally, it triggers inflammation, which can lead to cellular damage over time. Studies have explored this connection. For instance:
A 2008 meta-analysis suggested stress might be linked to a higher risk of lung cancer.
A 2019 review indicated that work-related stress could increase the likelihood of lung, colorectal, and esophageal cancers.
Understanding how stress impacts your body can empower you to take steps to protect your health and reduce potential risks.
Key Takeaways
Long-term stress makes your immune system weaker. This makes it harder to fight sickness, including cancer.
Reducing stress with things like exercise or mindfulness helps your health and lowers cancer risk.
Stress can cause bad habits like smoking or overeating, which raise cancer risk.
Knowing how stress affects your body helps you make healthier choices.
Get help if stress impacts your life. Good coping skills can make you feel better.
What is stress, and how does it affect the body?

Defining stress
Stress is your body’s natural response to challenges or demands. It can arise from various situations, such as work deadlines, personal conflicts, or unexpected events. Scientific literature defines stress in multiple ways, often distinguishing between acute stressors (short-term) and subjective stress (how you perceive a situation). This lack of a consistent definition makes it challenging to compare research findings. However, most agree that stress triggers physical, emotional, and behavioral changes aimed at helping you adapt to the situation.
Acute stress vs. chronic stress
Acute stress occurs over a short period and usually resolves quickly. For example, you might feel acute stress before a big presentation or during a sudden emergency. This type of stress activates your body’s “fight or flight” response, which prepares you to handle immediate threats. Chronic stress, on the other hand, persists over time. It can result from ongoing issues like financial problems or caregiving responsibilities. Unlike acute stress, chronic stress keeps your body in a heightened state of alert, which can lead to long-term health problems. Research shows that chronic stress affects cardiovascular and neuroendocrine systems differently than acute stress, as highlighted in studies by Chida and Hamer (2008) and Matthews et al. (2001).
Study | Findings |
|---|---|
Chida, Y. & Hamer, M. (2008) | Chronic stress impacts physiological responses over time. |
Matthews, K. A., Gump, B. B. & Owens, J. F. (2001) | Chronic stress alters cardiovascular and neuroendocrine responses. |
Physiological effects of chronic stress
Chronic stress affects your body through several mechanisms. The autonomic nervous system (ANS) plays a key role, with the sympathetic nervous system (SNS) preparing your body for emergencies and the parasympathetic nervous system (PNS) helping it recover. Prolonged activation of the ANS due to chronic stress causes wear-and-tear on your body. Cortisol, a hormone released during stress, regulates blood pressure and impacts systems like reproduction and digestion. The hypothalamic-pituitary-adrenal (HPA) axis also becomes overactive, increasing cortisol levels. This can disrupt gut-brain communication, leading to gastrointestinal discomfort. Over time, these physiological changes may contribute to conditions that increase cancer risk, raising the question: Cancer is caused by stress? While stress doesn’t directly cause cancer, its effects on your body can create an environment where cancer is more likely to develop.
Key physiological effects of chronic stress include:
Prolonged activation of the autonomic nervous system.
Increased cortisol production through the HPA axis.
Disruption of gut-brain communication.
Cancer is caused by stress? Exploring the biological mechanisms
Immune system suppression
Your immune system plays a crucial role in protecting your body from harmful invaders, including cancer cells. Chronic stress weakens this defense system, making it harder for your body to detect and destroy abnormal cells. Studies show that higher stress levels correlate with a significant increase in illness risk. For example, individuals with stress scores above 300 experience a 90% higher incidence of illness compared to those with lower scores. Stress also disrupts immune surveillance, which is essential for identifying and eliminating cancerous cells.
Stress-related hormones like norepinephrine and glucocorticoids further impair immune function. Norepinephrine promotes angiogenesis, the formation of new blood vessels that feed tumors, while glucocorticoids inhibit apoptosis, or programmed cell death. This creates an environment where cancer cells can grow and spread more easily.
Stress Source | Immune Function Impact | Cancer Biology Impact |
|---|---|---|
Daily Stress | Disrupts overall immune response | Increases angiopoietins, promoting tumor growth |
Social Isolation | Suppresses immune function | Down-regulates natural killer cells |
Chronic inflammation
Chronic stress triggers prolonged inflammation, which can damage healthy tissues and create conditions that support cancer development. Inflammation is your body’s natural response to injury or infection, but when it becomes chronic, it can lead to cellular damage and mutations. Research highlights that prolonged inflammatory responses are linked to tumorigenesis, particularly in hepatocellular carcinoma (HCC). Stress-related mediators, such as cytokines, play a significant role in this process.
Inflammation also affects the tumor microenvironment, making it more conducive to cancer progression. For instance, stress-induced inflammation can activate neutrophils, a type of white blood cell, which may inadvertently aid tumor growth. This connection underscores the importance of managing stress to reduce inflammation and its potential impact on cancer risk.
Hormonal changes and cancer risk
Stress alters your body’s hormonal balance, which can increase cancer risk. The release of stress hormones like cortisol and norepinephrine affects various biological processes. Cortisol, for instance, regulates blood sugar and immune responses, but chronic stress leads to its overproduction. This can suppress your immune system and promote cancer cell survival.
Norepinephrine, another stress hormone, stimulates angiogenesis and metastasis, enabling tumors to grow and spread. Additionally, glucocorticoids released during stress inhibit apoptosis, allowing cancer cells to evade destruction. These hormonal changes create a biological environment that supports tumor progression and resistance to treatment.
Chronic stress doesn’t directly cause cancer, but its effects on your immune system, inflammation, and hormones can significantly increase your risk. Understanding these mechanisms can help you take proactive steps to manage stress and protect your health.
What does research reveal about stress and cancer?
Evidence supporting the link
Research has shown that stress can influence cancer risk through various mechanisms. A recent study from the China Kadoorie Biobank analyzed data from nearly half a million participants. It found that individuals who experienced stressful life events had significantly higher odds of developing cancer. For example, those who reported one stressful event had an odds ratio of 1.80, while those with two or more events had an odds ratio of 3.05. Specific events, such as the loss of income or major family conflicts, were particularly associated with increased cancer prevalence.
Stressful Life Events | Odds Ratio (OR) | 95% Confidence Interval (CI) |
|---|---|---|
1 Event | 1.80 | 1.58–2.05 |
2 or More Events | 3.05 | 2.18–4.28 |
Loss of Income | 2.64 | 1.81–3.86 |
Major Family Conflict | 1.73 | 1.20–2.50 |
Death of Family Member | 2.36 | 2.05–2.72 |
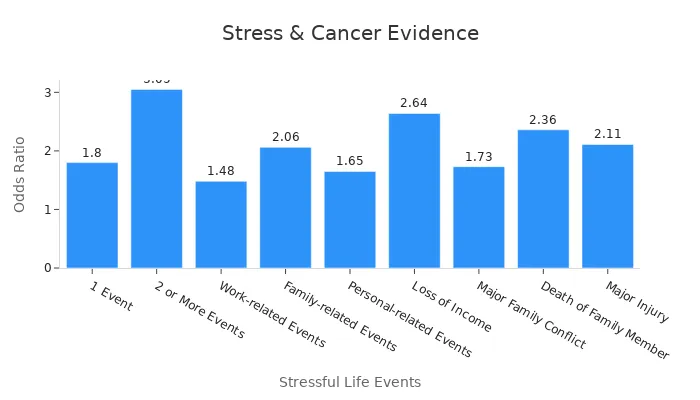
Other studies also support this connection. For instance, a 2008 meta-analysis of 142 prospective studies found a link between stress and a higher incidence of lung cancer. Similarly, a 2019 meta-analysis of nine observational studies indicated that work-related stress increases the risks of lung, colorectal, and esophageal cancers.
Evidence against a direct causal link
While stress appears to influence cancer risk, not all studies agree on a direct causal relationship. A study involving over 100,000 UK women found no link between perceived stress levels or adverse life events in the past five years and breast cancer risk. Additionally, while some research suggests that stress may correlate with decreased survival rates in cancer patients, the overall evidence for a direct impact of stress on survival remains weak.
These findings highlight the complexity of the relationship between stress and cancer. Stress may act as a contributing factor rather than a direct cause, making it essential to consider other variables, such as lifestyle and genetic predisposition.
The role of lifestyle factors
Lifestyle factors often mediate the relationship between stress and cancer risk. Chronic stress can lead to unhealthy behaviors, such as smoking, overeating, or alcohol consumption, which directly increase cancer risk.
Lifestyle Factor | Impact on Cancer Risk |
|---|---|
Chronic Stress | May lead to unhealthy behaviors (smoking, overeating) |
Unhealthy Behaviors | Directly associated with increased cancer risks |
For example, a breast cancer surgeon observed that many patients diagnosed with breast cancer had experienced significant stressors, such as divorce or the death of a parent. These stressors often triggered lifestyle changes that contributed to cancer development. Managing stress effectively can help you avoid these behaviors and reduce your overall risk.
Can managing stress reduce cancer risk?
Benefits of stress management
Managing stress can significantly improve your overall health and reduce cancer risk. Stress management techniques enhance immune function, which helps your body detect and eliminate abnormal cells. For example, research shows that pre-surgery stress management improves mood and boosts immune responses after surgery. In breast cancer patients, cognitive behavioral therapy (CBT) for stress management has been shown to improve emotional well-being and immune cell function.
Stress management also reduces inflammation, a key factor in cancer development. Studies reveal that experienced meditators have lower cortisol and immune responses to stress, which helps minimize inflammation. By managing stress effectively, you create a healthier environment in your body, making it less susceptible to cancer-related risks.
Practical stress management tips
You can adopt several strategies to manage stress and protect your health. Here are some practical tips:
Practice mindfulness or meditation: Regular meditation reduces stress hormones and promotes relaxation.
Engage in physical activity: Exercise releases endorphins, which improve mood and reduce stress.
Maintain a healthy diet: Eating nutrient-rich foods supports your immune system and overall well-being.
Prioritize sleep: Aim for 7-8 hours of quality sleep each night to help your body recover from daily stress.
Connect with others: Building strong social support networks can help you cope with stressful situations.
These strategies not only lower stress but also promote healthier behaviors, reducing your overall cancer risk.
When to seek professional help
Sometimes, managing stress on your own may not be enough. Chronic stress can increase cortisol levels, impair DNA repair, and weaken your immune system, raising your risk of cancers like breast and rectal cancer. If you experience persistent stress that affects your daily life, consider seeking professional help. Therapists trained in CBT can teach you effective coping mechanisms. Additionally, stress management programs tailored to your needs can enhance your emotional and physical health.
Recognizing when to seek help is crucial. Professional guidance can empower you to manage stress effectively, improving your quality of life and reducing cancer-related risks.
Stress does not directly cause cancer, but it creates conditions that may increase your risk. Chronic stress weakens your immune system, promotes inflammation, and disrupts hormonal balance. These changes can make your body more vulnerable to cancer progression. Managing stress plays a vital role in reducing these risks and improving your overall health.
Take proactive steps to manage stress effectively. Practice mindfulness, maintain a healthy lifestyle, and seek professional help when needed. By doing so, you empower yourself to protect your health. If you ever wonder, "Cancer is caused by stress?" remember that managing stress is key to prevention.
FAQ
Can stress alone cause cancer?
Stress alone cannot cause cancer. However, chronic stress weakens your immune system, promotes inflammation, and disrupts hormonal balance. These changes create conditions that may increase your risk of developing cancer. Managing stress effectively can help reduce this risk.
How does stress affect cancer treatment?
Chronic stress may reduce the effectiveness of cancer treatments. Stress hormones can promote tumor growth and spread, making it harder for treatments to work. Practicing stress management techniques, like mindfulness or therapy, can improve your emotional well-being and support your treatment journey.
Are all types of stress harmful?
Not all stress is harmful. Acute stress, like preparing for an exam, can motivate you and improve focus. Chronic stress, however, harms your body over time. It disrupts your immune system and increases inflammation, which may contribute to cancer risk. Learning to manage stress is essential for your health.
What are some quick ways to reduce stress?
You can reduce stress by practicing deep breathing, taking short walks, or listening to calming music. These activities help lower cortisol levels and promote relaxation. Regular exercise, mindfulness, and connecting with loved ones also provide long-term stress relief.
Should I consult a doctor about stress-related health concerns?
Yes, you should consult a doctor if stress affects your daily life or physical health. Persistent stress can lead to serious issues, including increased cancer risk. A healthcare professional can guide you toward effective stress management strategies and provide personalized advice.
See Also
Key Signs and Risk Factors of Stomach Cancer
Recognizing Symptoms and Triggers of Esophageal Cancer
Identifying Symptoms and Origins of Laryngeal Cancer

