What is Cerebellar Astrocytoma and Its Symptoms

Cerebellar astrocytoma is a brain tumor that forms in the cerebellum, the part of your brain that controls balance and coordination. This condition arises from astrocytes, which are cells that support and protect neurons. It is most common in children, where it accounts for 15 to 25 percent of all brain tumors. In adults, however, it occurs far less frequently. Early signs you should watch for include persistent headaches, nausea, dizziness, and difficulty with coordination. In infants, symptoms like a large head size or a twisted neck may appear.
Key Takeaways
Cerebellar astrocytoma is a brain tumor mostly found in kids. It can cause headaches, feeling sick, and trouble with balance.
Finding it early is very important. If headaches or balance problems don’t go away, see a doctor quickly for better treatment chances.
Surgery is usually the first step. Doctors try to take out as much of the tumor as they can while keeping the brain safe.
Radiation and chemotherapy might be needed after surgery, especially for tough tumors. Talk to your doctor about all the treatments you can try.
Staying healthy helps you get better. Eat good food, stay active, and manage stress to feel stronger.
What is Cerebellar Astrocytoma?
Overview of Cerebellar Astrocytoma
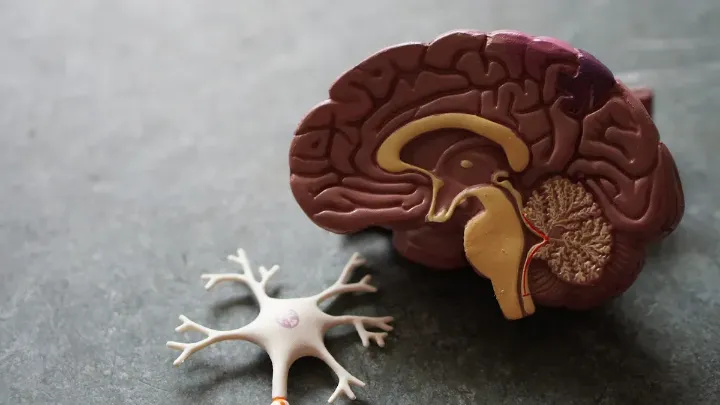
Location and function of the cerebellum
The cerebellum sits at the back of your brain, just above the brainstem. It plays a key role in controlling balance, coordination, and fine motor skills. When this area is affected by a tumor, you may notice clumsiness, difficulty walking, or trouble performing precise movements.
Role of astrocytes in the brain
Astrocytes are star-shaped cells that support and protect neurons in your brain. They help maintain the blood-brain barrier, regulate nutrients, and repair damage. However, when these cells grow abnormally, they can form tumors like cerebellar astrocytomas, which disrupt normal brain functions.
Types of Cerebellar Astrocytomas
Pilocytic astrocytoma (common in children)
Pilocytic astrocytomas are the most common type of cerebellar astrocytoma in children. These tumors grow slowly and are often low-grade, meaning they are less aggressive. With proper treatment, such as surgical removal, the prognosis is excellent.
Diffuse astrocytoma (more aggressive)
Diffuse astrocytomas are less common but more aggressive. They tend to invade surrounding brain tissue, making complete removal difficult. This type has a poorer prognosis compared to pilocytic astrocytomas.
Type of Astrocytoma | 5-Year Survival Rate | 10-Year Survival Rate | 20-Year Survival Rate |
|---|---|---|---|
Pilocytic Astrocytomas | 81% | 79% | |
Diffuse Astrocytomas | 7% | 7% | 7% |
Causes and Risk Factors
Genetic predispositions
Certain genetic mutations increase your risk of developing cerebellar astrocytomas. These include:
IDH1 gene mutation: Causes abnormal cell behavior in low-grade astrocytomas.
Li-Fraumeni syndrome: Linked to TP53 gene mutations, raising cancer risk.
Neurofibromatosis type 1: Leads to early-onset astrocytomas.
Tuberous sclerosis: Associated with TSC1 and TSC2 mutations.
Turcot syndrome: Involves tumor suppressor gene mutations.
In rare cases, cerebellar astrocytomas have been linked to von Hippel-Lindau disease, involving mutations in the VHL gene.
Environmental factors (e.g., exposure to radiation or toxins)
Exposure to ionizing radiation significantly increases your risk of developing cerebellar astrocytomas. For example, children who receive radiation therapy for conditions like acute lymphocytic leukemia are 22 times more likely to develop central nervous system tumors within five to ten years.
Symptoms of Cerebellar Astrocytoma
General Symptoms
Persistent headaches, especially in the morning
Morning headaches are one of the earliest signs of cerebellar astrocytoma. These headaches often result from increased intracranial pressure caused by the tumor. You may notice that the pain is more intense after waking up and gradually improves throughout the day.
Nausea and vomiting
Nausea and vomiting frequently accompany morning headaches. These symptoms occur due to the pressure the tumor places on the brain, disrupting normal functions. If these symptoms persist without an obvious cause, you should seek medical attention promptly.
Specific Symptoms Related to the Cerebellum
Loss of balance and coordination
Cerebellar astrocytomas directly affect the cerebellum, which controls balance and coordination. You might experience difficulty walking or standing steadily. Everyday activities, such as climbing stairs or turning corners, may feel unusually challenging.
Difficulty with fine motor skills
Tasks requiring precision, like writing or buttoning a shirt, can become difficult. This happens because the tumor interferes with the cerebellum's ability to manage fine motor control.
Dizziness or vertigo
You may feel dizzy or experience vertigo, a sensation of spinning or losing your sense of direction. This symptom often arises when the tumor disrupts the cerebellum's role in maintaining spatial awareness.
Symptoms in Infants and Young Children
Torticollis (twisted neck)
In infants, torticollis may develop as a result of the tumor's impact on muscle control. You might notice your child holding their head at an unusual angle or struggling to move their neck freely.
Ataxia (lack of muscle control)
Ataxia is another common symptom in young children. It can cause clumsiness or an unsteady gait. Your child may stumble frequently or have trouble performing simple movements.
Macrocephaly (abnormally large head size)
In infants, cerebellar astrocytomas can lead to macrocephaly. This occurs when increased intracranial pressure causes the head to grow larger than normal. If you observe this, consult a healthcare provider immediately.
Diagnosing cerebellar astrocytomas in infants can be challenging. Symptoms like torticollis and ataxia are nonspecific and may mimic other conditions. Advanced imaging techniques, such as MRI, are often required for accurate diagnosis.
Children with cerebellar astrocytomas often display symptoms like clumsiness, nausea, and vomiting. These signs typically result from increased intracranial pressure caused by the tumor. In some cases, additional symptoms like personality changes or nystagmus (involuntary eye movements) may also appear.
Symptoms Based on Tumor Progression
Increased intracranial pressure
As cerebellar astrocytomas grow, they can block the normal flow of cerebrospinal fluid in your brain. This blockage increases intracranial pressure, leading to severe symptoms. You might experience intense headaches that worsen over time. These headaches often feel more pronounced when you lie down or strain, such as during coughing or sneezing. Other signs include blurred vision, nausea, and a feeling of pressure behind your eyes. If left untreated, this condition can become life-threatening.
Tip: If you notice persistent headaches combined with nausea or vision changes, consult a healthcare provider immediately. Early intervention can prevent complications.
Vision or speech difficulties
Tumor progression can also affect your vision and speech. You may notice blurry or double vision, which occurs when the tumor presses on areas controlling eye movement. In some cases, you might develop nystagmus, where your eyes make involuntary, rapid movements. Speech difficulties, such as slurred or slowed speech, can arise if the tumor impacts the cerebellum's role in coordinating muscle movements. These changes often develop gradually, so paying attention to subtle shifts in your abilities is crucial.
Increased sleepiness or fatigue
As the tumor grows, you might feel unusually tired or sleepy throughout the day. This fatigue results from the brain's struggle to function under increased pressure. You may find it harder to stay alert or concentrate on tasks. In severe cases, excessive sleepiness could indicate a medical emergency, as it may signal significant pressure on your brainstem.
Note: Fatigue caused by cerebellar astrocytoma often doesn't improve with rest. If you feel persistently drained, seek medical advice to rule out serious conditions.
How is Cerebellar Astrocytoma Diagnosed?
Medical History and Physical Examination
Neurological assessments
Diagnosing cerebellar astrocytoma begins with a thorough neurological assessment. During this process, your doctor evaluates your reflexes, muscle strength, coordination, and balance. These tests help identify abnormalities in the cerebellum's function. While neurological exams are essential, they cannot confirm the presence of a tumor. Imaging studies are necessary for a definitive diagnosis.
Component | Description |
|---|---|
Imaging Studies | |
MRI | Produces detailed images of the brain to visualize the tumor. |
CT Scan | Used when MRI is not available; provides images of the tumor using X-rays. |
Frameless Stereotactic Guidance | Enhances precision in tumor location during surgery using 3D reconstruction from MRI data. |
Patient-reported symptoms
Your symptoms play a critical role in the diagnostic process. Persistent headaches, nausea, dizziness, or difficulty with coordination often prompt further investigation. If you experience these symptoms, your doctor may recommend imaging tests to confirm the diagnosis.
Imaging Techniques
MRI (Magnetic Resonance Imaging)
MRI is the most effective imaging technique for identifying cerebellar astrocytomas. It provides highly detailed images of your brain, allowing doctors to locate the tumor and assess its size. MRI scans often include contrast agents to highlight the tumor more clearly. Advanced methods like MRI spectroscopy can analyze the tumor's chemical composition, while functional MRI (fMRI) maps brain activity to aid in surgical planning.
CT (Computed Tomography) scans
CT scans serve as an alternative when MRI is unavailable. These scans use X-rays to create cross-sectional images of your brain. Although less detailed than MRI, CT scans can still detect tumors and their impact on surrounding structures.
Additional Diagnostic Tests
Biopsy for tumor analysis
A biopsy involves removing a small sample of the tumor tissue for analysis. This test confirms the tumor type and grade, helping your doctor determine the best treatment plan. In some cases, frameless stereotactic guidance enhances the precision of the biopsy procedure.
Lumbar puncture (if needed)
In rare cases, your doctor may recommend a lumbar puncture to analyze cerebrospinal fluid. This test helps detect tumor cells or increased pressure caused by the tumor. However, it is not commonly used unless other tests suggest its necessity.
Tip: Early diagnosis improves treatment outcomes. If you notice persistent symptoms, consult a healthcare provider promptly.
Treatment Options for Cerebellar Astrocytoma
Surgery
Tumor resection techniques
Surgery is often the first step in treating cerebellar astrocytoma. The goal is to remove as much of the tumor as possible while preserving brain function. Surgeons use advanced techniques like frameless stereotactic guidance to precisely locate and remove the tumor. In a study involving 50 patients, gross total resection (GTR) was achieved in 76% of cases, showing the effectiveness of surgical intervention.
Risks and recovery
While surgery offers high success rates, it carries risks. Neurological complications, such as cognitive deficits or emotional disturbances, may occur in some patients. Studies report that 43% of patients experience neurological sequelae, and 19% face school-related challenges due to cognitive issues. Recovery depends on the extent of the surgery and the patient’s overall health. With proper care, many patients regain normal function and enjoy a good quality of life.
Radiation Therapy
When radiation is used
Radiation therapy is recommended when the tumor cannot be completely removed or if cancer cells remain after surgery. It also helps prevent tumor regrowth. This treatment is often used as a follow-up to surgery to ensure all tumor cells are destroyed.
Types of radiation therapy
Several types of radiation therapy are available:
Conformal radiation therapy: Shapes radiation beams to match the tumor’s size and shape.
Intensity-modulated radiation therapy (IMRT): Delivers radiation at varying intensities from multiple angles.
Stereotactic radiation therapy: Targets the tumor with high precision, minimizing damage to healthy tissue.
Proton beam radiation therapy: Uses protons to focus radiation on the tumor while sparing nearby healthy cells.
Chemotherapy
Medications used
Chemotherapy is another option for treating cerebellar astrocytomas. Common drugs include carboplatin, vincristine, and temozolomide. Combination therapies, such as carboplatin with vincristine, are also frequently used.
Chemotherapy Drug Options | Description |
|---|---|
Carboplatin + Vincristine | Commonly used regimen |
Temozolomide | Frequently used alone or in combination |
Irinotecan + Bevacizumab | Additional treatment option |
Side effects and management
Chemotherapy can cause side effects like nausea, fatigue, and hair loss. Managing these effects involves supportive care, such as anti-nausea medications and dietary adjustments. Your healthcare team will monitor your response to treatment and adjust the plan as needed to minimize discomfort.
Tip: Discuss all treatment options with your doctor to choose the best approach for your condition.
Factors Influencing Treatment Decisions
Tumor type and grade
The type and grade of a cerebellar astrocytoma play a significant role in determining the best treatment approach. Tumors like pilocytic astrocytomas are typically low-grade and grow slowly. These tumors often respond well to surgical removal, and additional treatments may not be necessary. On the other hand, diffuse astrocytomas are more aggressive and invasive. They often require a combination of surgery, radiation therapy, and chemotherapy to manage their progression.
Doctors assess the tumor grade based on how abnormal the cells appear under a microscope. Low-grade tumors usually have a better prognosis and fewer complications. High-grade tumors, however, tend to grow faster and may spread to nearby tissues. This makes them more challenging to treat. Understanding the tumor's characteristics helps your healthcare team create a personalized treatment plan that maximizes effectiveness while minimizing risks.
Tip: If you or a loved one has been diagnosed with a cerebellar astrocytoma, ask your doctor about the tumor's grade and how it impacts treatment options.
Patient age and overall health
Your age and overall health significantly influence treatment decisions. Younger patients, especially infants under one year, often face unique challenges. Studies show that infants have poorer progression-free survival rates compared to older children. Their developing bodies may not tolerate aggressive treatments like radiation therapy. In such cases, doctors may prioritize less invasive options or delay certain treatments until the child is older.
Your overall health also determines how well you can handle specific treatments. For example, chemotherapy and radiation therapy can cause side effects like fatigue and nausea. Patients with pre-existing conditions or weakened immune systems may struggle with these treatments. Doctors carefully evaluate your health status to decide whether to proceed with surgery, chemotherapy, or observation.
Note: Maintaining good overall health can improve your ability to tolerate treatments and recover more quickly. Discuss any health concerns with your doctor to ensure the best possible care.
Cerebellar astrocytoma is a serious condition that affects balance, coordination, and neurological functions. Early detection plays a key role in improving outcomes. On average, patients with cerebellar glioma survive for 73.8 months, while those with glioblastoma face shorter survival periods of three to seven months. Long-term outcomes vary, with 60 out of 104 patients experiencing permanent neurological deficits. However, advancements in treatment have led to survival rates as high as 90% over five years. If you notice symptoms, consult a healthcare provider promptly to explore treatment options and improve quality of life.
FAQ
What is the survival rate for cerebellar astrocytoma?
The survival rate depends on the tumor type and grade. For pilocytic astrocytomas, the 5-year survival rate is around 85%. Diffuse astrocytomas have a much lower survival rate of about 7%. Early diagnosis and treatment improve outcomes significantly.
Can cerebellar astrocytoma recur after treatment?
Yes, recurrence is possible, especially with high-grade tumors. Regular follow-up appointments and imaging tests help monitor for any signs of regrowth. Discuss a long-term care plan with your doctor to stay proactive.
Are cerebellar astrocytomas always cancerous?
Not all cerebellar astrocytomas are cancerous. Low-grade tumors, like pilocytic astrocytomas, are typically benign. However, high-grade tumors, such as diffuse astrocytomas, are malignant and more aggressive.
How long does recovery take after surgery?
Recovery time varies. Most patients need several weeks to months to regain strength and coordination. Physical therapy often helps speed up recovery. Your doctor will guide you based on your specific condition.
Can lifestyle changes help manage symptoms?
Yes, maintaining a healthy lifestyle can support recovery. Focus on balanced nutrition, regular exercise, and stress management. These habits improve overall well-being and may help you cope better with treatment side effects.
Tip: Always consult your healthcare provider before making significant lifestyle changes during treatment.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Key Insights Into Symptoms of Adrenocortical Carcinoma
Understanding Angioimmunoblastic T-Cell Lymphoma Symptoms and Identification
Exploring Acute Lymphoblastic Leukemia and Its Key Symptoms
Symptoms and Treatment Options for Adrenocortical Adenoma Explained

