10 Practical Tips for Managing Chemotherapy Side Effects at Home

You are not alone in facing the daily challenges of chemotherapy. Many people—about one-quarter to over two-fifths—experience side effects that make everyday life at home harder. Fatigue, nausea, mouth sores, neuropathy, and hair loss can all show up during treatment.
Fatigue
Mouth sores
Nerve damage
Infections
Changes in appetite
Hair loss
Chemotherapy Side Effects: Managing the Impact looks different for everyone. Stay in touch with your care team and remember, small changes at home can help you feel safer and more comfortable.
Key Takeaways
Track your symptoms daily and communicate often with your care team to manage side effects early and stay in control.
Eat small, bland meals and try natural remedies like ginger or peppermint to ease nausea and improve appetite.
Rest regularly, keep a sleep routine, and do gentle activities like walking or stretching to fight fatigue and boost mood.
Protect your skin and mouth with gentle care, avoid harsh foods or products, and keep your home safe to prevent injuries and infections.
Stay connected with friends, family, and support groups to care for your emotional health and feel less alone during treatment.
Chemotherapy Side Effects: Managing the Impact
Why Side Effects Occur
You might wonder why chemotherapy brings so many changes to your body. Chemotherapy Side Effects: Managing the Impact starts with understanding how these drugs work. Chemotherapy targets cancer cells because they grow and divide quickly. But some healthy cells in your body also grow fast. These include cells in your digestive tract, hair, bone marrow, and mouth. When chemotherapy damages these healthy cells, you feel side effects.
Cells in your digestive tract can get hurt, leading to nausea or mouth sores.
Hair follicles are sensitive, so you may notice hair loss.
Bone marrow makes blood cells. Damage here can cause anemia or lower your immunity.
Sometimes, nerves get affected, which can cause tingling or numbness in your hands and feet.
Hormonal changes may also happen, affecting how you feel day to day.
Chemotherapy Side Effects: Managing the Impact depends on your health, the type of cancer, and the treatment plan. Some people feel mild symptoms, while others have stronger reactions.
Proactive Management
You can take steps to make Chemotherapy Side Effects: Managing the Impact easier. Acting early helps you stay on track with your treatment and feel more in control. When you manage symptoms right away, you lower the risk of having to stop or change your treatment. This can help you get better results and keep your quality of life higher.
Talk with your care team often. They can help you find ways to handle side effects before they get worse.
Use a diary or a mobile app to track your symptoms each day. This helps you spot patterns and share details with your doctor.
Tracking symptoms can help you tell the difference between normal changes and signs that need quick attention.
Many people who use symptom tracking tools feel less pain and stress. They also have fewer emergency visits and feel more satisfied with their care.
Early action can help you manage fatigue, nausea, and even your mood.
Tip: Try writing down how you feel each day or using an app to log symptoms. This simple step can make Chemotherapy Side Effects: Managing the Impact much easier to handle.
Chemotherapy Side Effects: Managing the Impact does not have to control your life. By staying alert and working with your care team, you can take charge and feel more comfortable at home.
Nausea Relief

Diet Tips
Nausea can make eating feel like a chore, but the right food choices can help you feel better. Try these simple tips to keep your stomach calm:
Eat small meals every 2–3 hours instead of three big ones. This keeps your stomach from getting too full or too empty.
Choose cold or room-temperature foods. Hot foods often have strong smells that can trigger nausea.
Start with dry, bland foods like crackers, pretzels, or dry toast. These are gentle on your stomach.
Pick starchy foods such as rice, potatoes, applesauce, or bananas. These are easy to digest.
Avoid spicy, oily, or very sweet foods. These can make nausea worse.
Drink fluids between meals, not during. Sipping water, ginger tea, or clear broth throughout the day helps you stay hydrated without making you feel too full.
Take your medications with a light snack if your doctor says it’s okay.
Stay away from strong smells—ask someone else to cook, or eat in a well-ventilated room.
Tip: Keep a snack like crackers by your bed. Eating a little before getting up can help settle your stomach in the morning.
Home Remedies
Some natural remedies can also help ease nausea. Ginger and peppermint are two favorites among people going through chemotherapy.
Remedy | How to Use | What Studies Show |
|---|---|---|
Ginger | Ginger tea, ginger ale, or ginger capsules (0.5–1g daily) | May reduce acute nausea when used with anti-nausea meds |
Brewed tea or peppermint extract | Can soothe the stomach and lessen nausea severity |
Sip cold, clear liquids like ginger ale, apple juice, or peppermint tea throughout the day.
Popsicles, yogurt, and gelatin are gentle options if you don’t feel like eating much.
Try water with a splash of lemon or cucumber for a fresh taste.
If you feel weak or dizzy, check your urine color. Dark urine can mean you need more fluids.
Note: Always talk to your care team before trying new remedies or supplements. They can help you find what works best for you.
Fatigue Solutions
Feeling tired during chemotherapy is very common. Many people notice their energy drops, even after a good night’s sleep. You are not alone if you feel this way. Take a look at how often people report fatigue during treatment:
Study Description | Sample Size | Percentage Reporting Fatigue | Fatigue Severity Criteria |
|---|---|---|---|
Outpatient chemotherapy patients | 608 | ESAS-r-J score ≥3 | |
Cancer patients undergoing treatment (various reports) | N/A | 30–60% | Moderate to severe fatigue |
Chemotherapy patients in cross-sectional study | 59 | Severe fatigue in all but one |
Rest Strategies
You might feel like you need more rest than usual. That is normal. Try these ideas to help your body recover:
Stick to a regular sleep schedule. Go to bed and wake up at the same time each day.
Make your bedroom cozy, dark, and quiet. Use soft bedding and keep the room cool.
Avoid caffeine or nicotine before bedtime.
Create a relaxing routine before sleep. You could read, listen to music, or take a warm bath.
Turn off screens at least 30 minutes before bed.
Listen to your body. Take breaks before you feel worn out.
Plan your day. Do important tasks when you have the most energy.
Keep things you use often—like water, snacks, or your phone—close by.
Freeze meals ahead of time. This way, you have food ready when you feel too tired to cook.
Ask friends or family to help with chores. You do not have to do everything alone.
Tip: Short naps (20–30 minutes) can boost your energy without making you groggy.
Gentle Activity
Moving your body, even a little, can help fight fatigue. You do not need to run or lift heavy weights. Try these gentle activities:
Take short walks. Start slow and add a few minutes each week.
Try yoga or stretching. These help your muscles and calm your mind.
Use light strength exercises. You can use your own body weight or simple items like water bottles.
Break up activity into small chunks. A few minutes here and there add up.
Always listen to your body. Rest if you feel dizzy or weak.
Staying active, even in small ways, can help you feel stronger and improve your mood. Remember, every step counts!
Taste and Appetite
Food Choices
Chemotherapy can change how food tastes and smells. You might notice that sweet or bitter foods taste different, or you may not enjoy your favorite meals like before. Many people find that their appetite drops, and eating feels less enjoyable. These changes can make it hard to get enough calories, protein, and nutrients, which your body needs to heal and stay strong.
You can make food more appealing by trying new flavors and textures. Here are some ideas to help you enjoy eating again:
Choose bland, boiled, or cold foods if strong tastes bother you.
Add a little sweetness to meats, like a honey glaze, to make them taste better.
Marinate meats or meat substitutes to reduce bitterness.
Use herbs, spices, or condiments to boost flavor without making food too strong.
Avoid foods with strong smells, such as beef or fish, if they turn your stomach.
Try poultry, eggs, or dairy for protein if red meat tastes odd.
Use plastic utensils instead of metal to cut down on metallic tastes.
Keep your mouth clean by brushing your teeth before meals.
Drink small sips of water or clear liquids during meals to rinse away bad tastes.
Tip: If you have mouth sores, skip spicy, sour, or crunchy foods. Soft, cool foods like yogurt or pudding feel soothing.
Eating Habits
Changing how and when you eat can help you get the nutrition you need, even when your appetite is low. Eating small, frequent meals or snacks—about five or six times a day—works better than forcing yourself to eat three big meals.
Set a meal and snack schedule, and try to eat even if you are not hungry.
Keep healthy snacks nearby, like cheese sticks, nuts, or smoothies.
Use liquid nutrition drinks, such as milkshakes or soups, if solid foods are hard to eat.
Take a short walk before meals to help boost your appetite.
Make mealtime pleasant—eat with family, listen to music, or watch TV.
Try eating your biggest meal in the morning if that’s when you feel best.
Change up your routine by eating in a different spot or with a friend.
Remember, your taste and appetite may change from day to day. Be patient with yourself and try different foods until you find what works. If you struggle to eat enough, talk with your care team or a dietitian for extra support.
Neuropathy Care
Chemotherapy can sometimes cause nerve problems called neuropathy. You might notice numbness, tingling, or burning in your hands and feet. These feelings can make daily tasks harder and even affect your balance. Many people going through chemotherapy deal with these symptoms, so you are not alone.
Here’s a quick look at how common neuropathy is and what symptoms you might feel:
Aspect | Details |
|---|---|
Prevalence at chemotherapy end | |
Prevalence 2 months post-chemo | Drops to 31.1% |
Symptom severity | Most have mild to moderate symptoms |
Most common symptom | Numbness in both hands and legs |
Symptom pattern | Tingling, burning, stabbing pain in a “stocking and glove” pattern |
Home Safety
You can take steps at home to protect yourself from falls and injuries. Neuropathy can make it hard to feel sharp objects or changes in temperature. Try these safety tips:
Wear shoes with good traction to help prevent slips and falls.
Use nightlights so you can see clearly if you get up at night.
Check bath water with a thermometer before getting in to avoid burns.
Install grab bars and handrails in places like the bathroom or stairs.
Keep floors clear of clutter and loose rugs to reduce tripping hazards.
Ask a physical or occupational therapist to check your home for extra safety ideas.
Tip: Always look where you step and move slowly if your feet feel numb.
Comfort Tips
You can also find ways to make your hands and feet feel better at home. Self-care makes a big difference. Try these ideas:
Follow a care plan that fits your needs. This might include help with walking, pain, or taking medicine.
Do gentle exercises to keep your muscles strong and improve balance.
Check your feet and hands every day for cuts or blisters. Treat any wounds right away.
Wear soft, loose socks and gloves to keep your hands and feet warm.
Eat a healthy diet and stay active to support nerve health.
Avoid smoking and limit alcohol, as these can make neuropathy worse.
Ask for emotional support if you feel worried or alone.
Some people also try massage, acupuncture, or physical therapy. These may help, but results can vary. Always talk with your care team before starting new treatments.
Remember, you can take steps to stay safe and comfortable at home. Small changes can help you feel more in control each day.
Mouth Sores
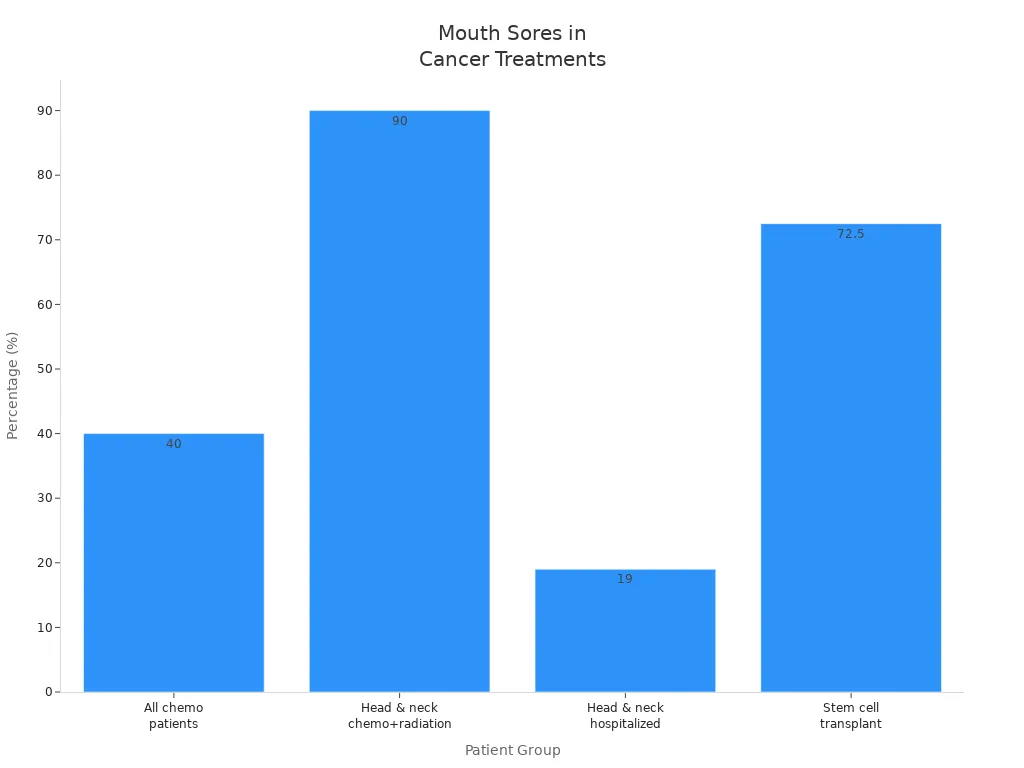
Mouth sores, also called oral mucositis, can make eating and talking tough during chemotherapy. You are not alone—about 40% of people on chemo get mouth sores. If you have head and neck cancer and get both chemo and radiation, the chance goes up to 90%. Good oral care can help you feel better and lower your risk.
Oral Care
You can protect your mouth with a gentle routine. Here are some easy steps:
Wash your hands before and after caring for your mouth.
Use a soft toothbrush or foam swab to clean your teeth 2–4 times a day.
Brush gently after meals and before bed.
Rinse your mouth often with a mild solution—try salt water or baking soda in water.
Skip mouthwashes with alcohol. They can dry and sting your mouth.
Check your mouth every day with a flashlight and mirror. Look for sores or bleeding.
Keep your lips moist with balm or lanolin.
Drink plenty of water. Suck on ice chips or popsicles to soothe pain.
Eat soft, moist foods in small bites.
Ask your care team before flossing or using new mouth rinses.
Tip: Cold foods like yogurt or applesauce can feel soothing if your mouth hurts.
Foods to Avoid
Some foods can make mouth sores worse. Try to skip these to keep your mouth comfortable:
Spicy, salty, or acidic foods (like salsa, citrus fruits, or tomato juice)
Hard, rough, or crunchy foods (such as chips, crackers, or crusty bread)
Hot foods and drinks
Raw vegetables and sour dairy products
Caffeinated, carbonated, or alcoholic drinks
Grapefruit and grapefruit juice
Choose soft, creamy, or pureed foods instead. Lukewarm or cold foods often feel best. Rinse your mouth before eating to help with taste and comfort.
If eating is hard, talk to your care team about meal ideas or special mouth rinses. Taking care of your mouth helps you heal and keeps you feeling your best.
Hair and Scalp
Gentle Care
Hair loss is one of the most common side effects of chemotherapy. You might notice your hair thinning or falling out in clumps. For many people, this feels like the hardest part of treatment. In fact, studies show that over 90% of breast cancer patients experience hair loss, and almost all say it affects their quality of life. Some people even think about stopping treatment because of it. You are not alone if you feel upset or worried.
You can take steps to care for your hair and scalp gently:
Wash your hair every 2 to 4 days with a mild or baby shampoo.
Use a soft-bristle brush or comb. Start at the ends and work up to your scalp.
Pat your hair dry with a soft towel. Avoid rubbing.
Skip hair dryers, curling irons, and straighteners. Heat can make hair fall out faster.
Do not use hair sprays, dyes, bleach, or perms.
Try cutting your hair short before treatment starts. Some people find this helps them feel more in control.
Sleep on a satin or silk pillowcase to reduce tangles.
Protect your scalp from the sun with a hat or scarf. In cold weather, wear a soft cap to stay warm.
Tip: Wash your hair after swimming to remove chlorine or chemicals that can irritate your scalp.
Taking care of your scalp helps you feel more comfortable and protects your skin. If your scalp feels dry or itchy, use a gentle, fragrance-free moisturizer.
Head Coverings
Losing your hair can change how you feel about your appearance. Many people choose to wear head coverings for comfort, warmth, or style. You have lots of options:
Scarves: Lightweight and easy to tie. You can find many colors and patterns.
Turbans: Soft, pull-on hats that stay in place and look stylish.
Wigs: Made to look like real hair. You can match your natural color or try something new.
Baseball hats: Some are made just for cancer patients and offer extra coverage.
Beanies and knit caps: Cozy and gentle on your scalp, perfect for cooler days.
Sunhats: Wide brims protect your scalp from the sun when you go outside.
Silk sleep caps: Keep your head warm and prevent tangling at night.
Head Covering | Best For | Special Features |
|---|---|---|
Scarf | Everyday wear | Lightweight, many styles |
Comfort and style | Easy to put on, stays in place | |
Wig | Natural look | Customizable, realistic |
Baseball hat | Casual outings | Extra coverage, sporty |
Beanie/Knit cap | Warmth | Soft, stretchy, cozy |
Sunhat | Outdoor protection | Wide brim, shields from sun |
Silk sleep cap | Nighttime comfort | Gentle, reduces friction |
Remember, you get to choose what feels right for you. Some people go without any covering, and that is okay too. Support from friends, family, or a support group can help you feel more confident during this time.
Skin Protection
Chemotherapy can make your skin feel dry, itchy, or extra sensitive. You might notice redness, rashes, or even changes in how your skin looks. Taking care of your skin helps you feel more comfortable and lowers your risk of infection or injury.
Here are some common skin changes you might see during treatment:
Skin Condition | What It Looks Like / Feels Like | Main Cause / Common Drugs |
|---|---|---|
Dry skin (Xerosis) | Flaky, rough, sometimes greasy patches | EGFR inhibitors |
Photosensitivity | Sunburns easily, redness after sun | Methotrexate, Fluorouracil, Dacarbazine |
Hand-Foot Syndrome | Red, sore, peeling skin on hands and feet | Capecitabine, Docetaxel, Doxorubicin |
Acne-like rash | Red bumps, mostly on face | EGFR inhibitors, Actinomycin D |
Hyperpigmentation | Dark patches or streaks | Bleomycin, Fluorouracil |
Nail changes | Brittle, discolored, or ridged nails | Taxanes, Anthracyclines |
Moisturizing
Your skin may get dry or cracked during chemo. You can help by using a gentle, fragrance-free moisturizer twice a day. Look for creams with ingredients like hyaluronic acid, ceramides, shea butter, or urea. These help lock in moisture and protect your skin.
Product Name | Key Features & Ingredients | Best For | Fragrance-Free |
|---|---|---|---|
Recovery Skin Relief Cream | Soothing, gentle | All-over dry skin | Yes |
Lindi Skin Body Lotion | Works well on damp skin | After shower | Yes |
Bag Balm Moisturizing Hand Lotion | Shea butter, jojoba, lanolin | Hands and feet | Yes |
Oncoderm Chemotherapy Cream | Urea, ceramides, hypoallergenic | Cracked skin | Yes |
CeraVe Daily Moisturizing Lotion | Hyaluronic acid, ceramides | Face, body, hands | Yes |
Tip: Avoid hot showers and scrubbing. Pat your skin dry and apply lotion right after bathing.
Sun Safety
Chemotherapy can make your skin burn more easily, even on cloudy days. Protecting yourself from the sun keeps your skin safe and helps prevent painful reactions.
Use a broad-spectrum sunscreen with SPF 30 or higher. Reapply often, especially after sweating or swimming.
Wear long sleeves, pants, a wide-brimmed hat, and sunglasses.
Find shade under trees or umbrellas. Remember, water and sand reflect sunlight.
Drink plenty of water to keep your skin hydrated.
Get vitamin D from food or supplements, not from sunbathing.
Note: If you notice redness, swelling, or a rash after being outside, let your care team know. Your skin needs extra care during treatment.
Infection Prevention
Staying safe from infections is a big part of chemotherapy care. Your body’s defenses get weaker during treatment, so germs can cause problems more easily. You can lower your risk by following some simple steps at home.
Hygiene Tips
Chemotherapy often lowers your white blood cell count, especially neutrophils. This makes it harder for your body to fight off bacteria, viruses, and fungi. When your neutrophil count drops below 500, your risk of infection goes way up. Mucositis, or sores in your mouth and gut, can also let germs into your bloodstream.
Here are some ways you can protect yourself:
Wash your hands often with soap and water or use an alcohol-based hand sanitizer. This is the best way to stop germs.
Shower every day with mild soap. Keep your skin clean and dry.
Brush your teeth gently with a soft toothbrush. Rinse your mouth with salt water or saline 4–6 times a day.
Avoid sharing towels, cups, or eating utensils.
Stay away from people who are sick or from crowded places.
Eat only well-cooked foods. Skip raw meats, eggs, and unwashed fruits or veggies.
Keep cuts and scrapes clean and covered.
Avoid tampons, rectal thermometers, and enemas during treatment.
Change your bed sheets and towels often.
Tip: Keep a bottle of hand sanitizer in your bag or by your bed for quick cleaning.
Recognizing Signs
Even with good hygiene, infections can still happen. It’s important to know what to look for so you can get help fast. Fever is often the first sign. Other symptoms can show up, too.
Watch for these signs:
Chills or sweats
New cough or sore throat
Mouth sores
Shortness of breath
Burning or pain when you pee
Redness, swelling, or pain around wounds or ports
Diarrhea or vomiting
New pain anywhere
If you notice any of these, call your doctor right away. Keep a thermometer at home and check your temperature every day, especially 7–12 days after chemo, when your white blood cell count is lowest. Quick action can keep you safe and help you recover faster.
Emotional Well-Being

Chemotherapy can feel overwhelming, not just for your body but also for your mind. You might notice days when you feel anxious, sad, or just not like yourself. That’s normal. Taking care of your emotional health is just as important as looking after your body.
Stress Relief
You can try simple ways to calm your mind and ease stress at home. Many people find that a few minutes of quiet time each day helps them feel better. Here are some ideas you can use:
Practice deep breathing. Sit in a comfortable spot, close your eyes, and take slow, deep breaths. Inhale through your nose, hold for a moment, then exhale through your mouth. Repeat this a few times.
Try meditation or guided imagery. You can listen to calming music or use an app that leads you through a short meditation.
Write in a journal. Putting your thoughts on paper can help you process feelings and worries.
Take short walks outside. Fresh air and a change of scenery can lift your mood.
Do gentle stretches or yoga. Moving your body, even a little, can help you relax.
Tip: Even five minutes of quiet breathing or stretching can make a big difference in your day.
Your care team—doctors, nurses, and other staff—want to support you. They can listen to your concerns and help you find ways to cope. Sometimes, they may notice if you seem down or worried and can connect you with extra help if you need it.
Staying Connected
You don’t have to go through this alone. Staying in touch with others can boost your mood and help you feel supported. Here are some ways to stay connected:
Talk with family and friends. Share how you feel and let them know what you need.
Join a support group. Many people find comfort in talking with others who understand what they’re going through.
Use online tools or apps to connect with people, even if you can’t meet in person.
Ask your care team about local resources or expert volunteers who can offer support.
Let your nurses and doctors know if you feel lonely or need someone to talk to.
Remember: Many people feel stronger when they have support. Your care team, friends, and even people online can help you feel less alone.
Taking care of your emotional well-being can help you handle treatment better and improve your quality of life. You are resilient, and support is always within reach.
Daily Living Hacks
Home Organization
You can make life at home much easier by setting up your space for comfort and safety. Start by keeping the things you use most often within easy reach. Place water bottles, snacks, tissues, and your phone on a small table next to your favorite chair or bed. This way, you do not have to walk far when you feel tired.
Try these simple ideas to organize your home:
Use baskets or bins to group items together. Label them so you can find things quickly.
Keep a small basket in the bathroom with your toothbrush, toothpaste, and mouth rinse.
Store medications in a pill organizer. Set reminders on your phone so you never miss a dose.
Place a cozy blanket and slippers near your resting spot.
Clear walkways of clutter and loose rugs to prevent trips and falls.
Tip: Ask a friend or family member to help you set up your space. Sometimes, a fresh set of eyes can spot ways to make things even easier.
Helpful Tools
You do not have to do everything by hand. Many tools and gadgets can help you save energy and stay safe. Here are some favorites:
Tool or Gadget | How It Helps | Where to Use It |
|---|---|---|
Grabber tool | Picks up items without bending | Living room, bedroom |
Electric kettle | Heats water quickly and safely | Kitchen |
Pill organizer | Keeps track of daily medications | Bedroom, kitchen |
Shower chair | Lets you sit while bathing | Bathroom |
Non-slip socks | Prevents slips on smooth floors | All rooms |
Lightweight vacuum | Makes cleaning less tiring | Living areas |
You might also like using a voice assistant (like Alexa or Google Home) to set reminders or play music. These small changes can make a big difference in your day.
Remember, you deserve comfort and support. Try out different tools until you find what works best for you.
You have many ways to manage chemotherapy side effects at home. These tips can help you feel better and make daily life easier. Stay in touch with your care team and let them know how you feel. You can also look for support groups or trusted websites for more help.
Remember, you are not alone. Every step you take is a step toward healing. Keep going—hope is always within reach. 💙
FAQ
What should you do if a side effect gets worse suddenly?
Call your care team right away. Sudden changes can mean something serious. Keep your symptom diary handy so you can share details. Never wait if you feel very sick, have a fever, or notice new pain.
Can you keep working or going to school during chemotherapy?
You might be able to, but listen to your body. Some people work part-time or take breaks. Talk with your doctor and your boss or teacher. Ask for help when you need it.
How can you help your family understand what you’re going through?
Share how you feel each day.
Let them know what helps and what doesn’t.
Give them simple ways to support you, like making meals or just listening.
Honest talks can bring you closer together.
Are there foods you should always avoid during chemotherapy?
Stay away from raw meats, unwashed fruits or veggies, and foods past their expiration date. These can carry germs. Eat only well-cooked foods. If you have questions, ask your care team or a dietitian.
See Also
An In-Depth Overview Of Every Recognized Cancer Type
Exploring Symptoms And Treatment Options For Choroid Plexus Carcinoma
Recognizing Signs And Managing Treatment For Duodenal Cancer

