What is Chondrosarcoma and Its Symptoms
Chondrosarcoma is a rare type of cancer that begins in cartilage cells, which are found in bones and joints. You might notice symptoms like persistent pain, swelling, or stiffness in the affected area. These signs often worsen over time, making daily activities more challenging.
Early detection plays a critical role in improving outcomes. Most cases occur in adults aged 30 to 50, with an average diagnosis age of 42.5 years.
To promote awareness, educate yourself and others about bone sarcomas. Share information, support research, and advocate for policies that enhance cancer care. These efforts can help save lives and improve treatment options.
Key Takeaways
Chondrosarcoma is a rare type of cancer in cartilage. Watch for signs like long-lasting pain, swelling, or stiffness.
Finding it early is very important. If symptoms last for months, see a doctor to get better treatment results.
Your genes might raise your risk. Conditions like Ollier disease or past radiation can make chondrosarcoma more likely.
Surgery is the main way to treat it. Doctors remove the tumor and nearby tissue to stop it from coming back.
Learn about new treatments. Clinical trials and new therapies might help improve care for chondrosarcoma.
Symptoms of Chondrosarcoma

Common Symptoms
Persistent or worsening pain
One of the earliest signs of chondrosarcoma is pain in the affected area. This pain often persists even when you rest. Over time, it may worsen, making it difficult to ignore. You might notice the discomfort lasting for months or even years before seeking medical attention.
Swelling or a noticeable lump
Swelling is another common symptom. You may observe a lump forming near the tumor site. This lump can grow larger over time, becoming more noticeable. Swelling often accompanies pain, which can make the area feel tender to the touch.
Limited movement or stiffness in the affected area
Chondrosarcoma can also limit your ability to move. If the tumor develops near a joint, you might experience stiffness or reduced range of motion. Everyday activities, such as walking or bending, may become more challenging.
Symptom | Description |
|---|---|
Pain | Pain in the area of the tumor, which may not go away when resting. |
Swelling | Swelling in the area of the tumor. |
Large lump | A noticeable lump on the bone affected by chondrosarcoma. |
Duration of symptoms |
Additional Symptoms
Fractures from weakened bones
Chondrosarcoma weakens the bones where it develops. This can lead to fractures, even with minor injuries. If you experience a sudden break without a clear cause, it could be a sign of this condition.
Neurological symptoms (e.g., numbness, tingling, or weakness)
If the tumor presses on nearby nerves, you might feel numbness or tingling in the affected area. Weakness in the muscles surrounding the tumor is another possible symptom. These neurological signs often depend on the tumor's location.
Bowel or bladder control issues if the tumor presses on nerves
In rare cases, a tumor located near the spine may press on nerves that control your bladder or bowel. This can result in difficulty managing these functions. If you notice such changes, consult a healthcare professional immediately.
Causes and Risk Factors of Chondrosarcoma
Causes
Genetic mutations in cartilage cells
Chondrosarcoma often begins with changes in the genetic makeup of cartilage cells. These mutations disrupt normal cell behavior, leading to tumor growth. Some of the most common genetic alterations include:
Mutations in COL2A1, CDKN2A/B, and TP53, which drive tumor development.
Alterations in CDKN2A and TP53, frequently observed in high-grade cases.
Structural changes near the TERT promoter, found in about 20% of chondrosarcomas, especially in aggressive forms.
These mutations highlight the role of genetic instability in the progression of this cancer.
Unknown exact causes but potential genetic predispositions
While the exact cause of chondrosarcoma remains unclear, genetic predispositions may play a role. Research shows that mutations in IDH1 and IDH2 can trigger downstream genetic events, contributing to tumor evolution. Additionally, mutations in TP53 and CDKN2A may initiate the development of certain tumor types. These findings suggest that inherited or acquired genetic changes could increase your risk.
Risk Factors
Age (more common in adults over 40)
Your risk of developing chondrosarcoma increases with age. This cancer is most common in adults over 40, though it can occur at any age.
Pre-existing conditions like Ollier disease or Maffucci syndrome
Certain conditions, such as Ollier disease or Maffucci syndrome, significantly raise your risk. These rare disorders cause abnormal cartilage growth, which can lead to cancer.
Individuals with Ollier’s disease are at greater risk for developing chondrosarcoma.
History of radiation therapy
If you have undergone radiation therapy, especially for other cancers, your risk may be higher. Radiation can damage healthy cells, potentially leading to genetic mutations that cause tumors.
Understanding these causes and risk factors can help you recognize potential warning signs and seek medical advice early.
Diagnosis of Chondrosarcoma
Medical History and Physical Examination
Diagnosing chondrosarcoma begins with your medical history and a thorough physical examination. Your doctor will ask about symptoms, such as pain or swelling, and how long they have persisted. They may also inquire about any family history of cancer or genetic conditions that could increase your risk. During the physical exam, the doctor will check for lumps, tenderness, or restricted movement in the affected area. This step helps identify potential signs of a tumor and guides the need for further testing.
Imaging Tests
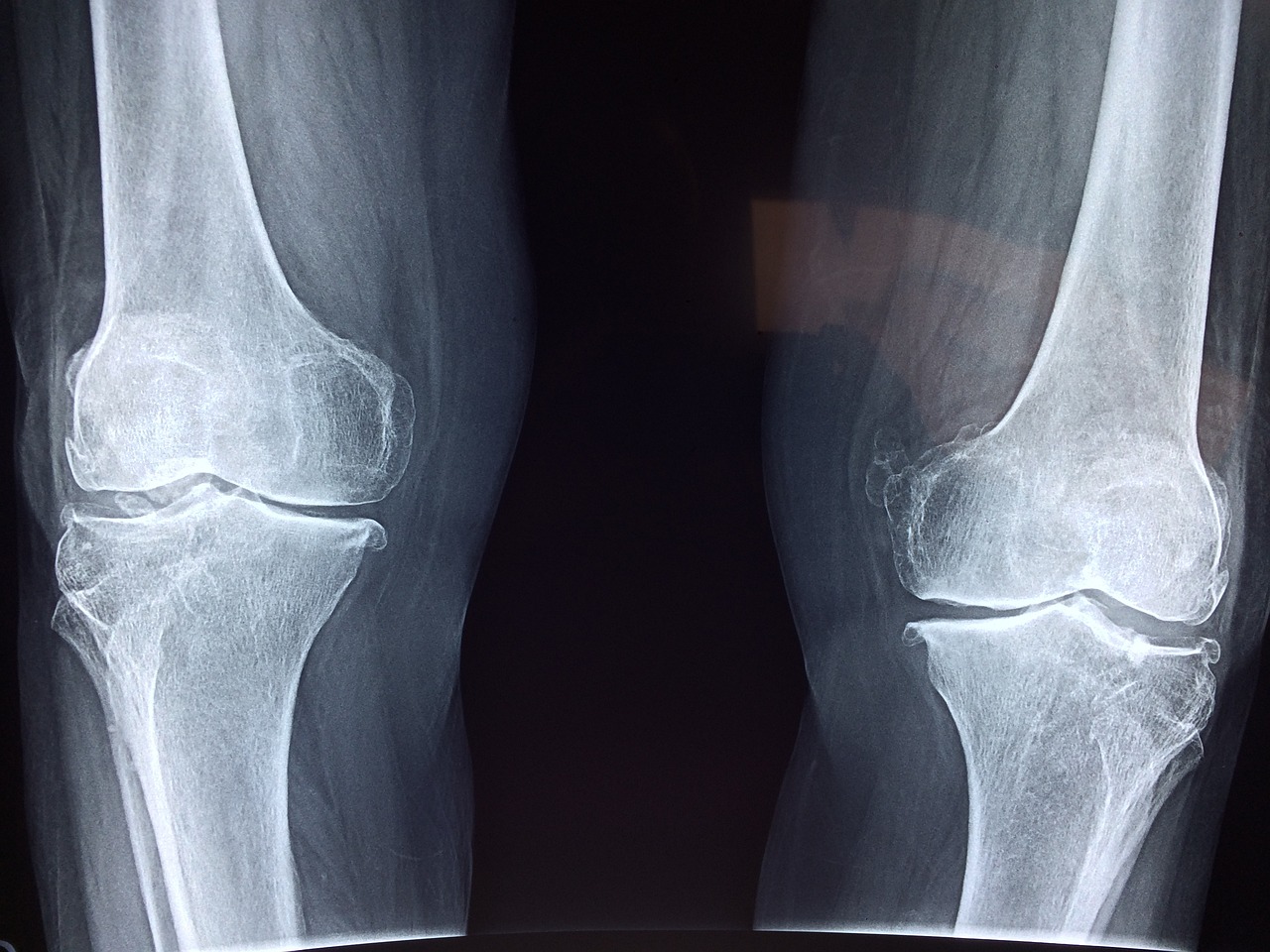
X-rays to detect bone abnormalities
X-rays are often the first imaging test used to evaluate chondrosarcoma. They can reveal abnormalities in the bone, such as irregular growths or areas of destruction. These images provide a basic overview of the tumor's location and size, helping doctors decide on the next steps.
MRI or CT scans for detailed imaging
For a more detailed view, your doctor may recommend an MRI or CT scan. MRI is the preferred method for diagnosing chondrosarcoma because it provides clear images of soft tissues and cartilage. It can also differentiate between various types of chondrosarcoma. However, if you have a medical device that prevents an MRI, a CT scan may be used instead. Both methods help determine the tumor's extent and its impact on surrounding tissues.
Radiology plays a crucial role in diagnosing cartilage tumors. Collaboration with an experienced musculoskeletal radiologist ensures accurate interpretation of imaging results.
Purpose | |
|---|---|
Bone scanning | Systemic staging of the tumor |
Chest CT | Systemic staging of the tumor |
Abdominal CT | Used for staging and evaluation |
Abdominal ultrasonography | Used for staging and evaluation |
MRI | Differentiates types of chondrosarcoma |
Biopsy
Needle biopsy or surgical biopsy
If imaging tests suggest a tumor, a biopsy is the next step. This procedure involves removing a small sample of tissue from the tumor for analysis. A needle biopsy uses a thin needle to extract tissue, while a surgical biopsy involves making an incision to remove a larger sample. Your doctor will choose the method based on the tumor's location and size.
Importance of tissue analysis for confirmation
Tissue analysis confirms whether the tumor is cancerous and determines its grade. This step is essential for planning treatment. However, biopsies carry risks, such as the potential spread of tumor cells along the biopsy tract. Chondrosarcomas have a gelatinous nature, which increases this risk. Proper planning and execution of the biopsy minimize complications and ensure accurate results.
Treatment Options for Chondrosarcoma
Surgery
Wide excision to remove the tumor
Surgery is the primary treatment for chondrosarcoma. Wide excision involves removing the tumor along with a margin of healthy tissue to ensure no cancer cells remain. This approach reduces the risk of recurrence. Studies show that 75% of patients achieve a five-year local recurrence-free survival rate. However, 24% experience local recurrences, with most occurring within the first two years after surgery. For localized chondrosarcomas, the five-year survival rate ranges from 80% to 90%.
Limb-sparing surgery vs. amputation
When the tumor affects a limb, doctors often consider limb-sparing surgery. This procedure removes the tumor while preserving as much of the limb as possible. Amputation may be necessary if the tumor is large, located in a challenging area, or if clear surgical margins cannot be achieved. Factors like your overall health, tumor size, and risk of complications influence the decision. Limb-sparing surgery aims to maintain function and quality of life, while amputation may be the safer option in certain cases.
Radiation Therapy
Used in cases where surgery is not possible
Radiation therapy is typically reserved for cases where surgery is not feasible. Chondrosarcomas are generally resistant to radiation due to their slow growth and low number of dividing cells. This limits its effectiveness as a curative treatment. Instead, radiation is often used to control symptoms or manage metastases. Advanced techniques, such as high-dose radiation, have shown promise in improving outcomes for patients with tumors in difficult-to-operate locations or those with incomplete excisions.
Chemotherapy
Limited effectiveness for most types
Chemotherapy is not effective for most chondrosarcoma types, especially conventional subtypes, which make up 85–90% of cases. These tumors resist standard chemotherapy treatments, and studies have not shown significant benefits from adjuvant chemotherapy in advanced cases.
Exceptions for aggressive subtypes
Some aggressive subtypes, such as mesenchymal and dedifferentiated chondrosarcomas, respond better to chemotherapy. Mesenchymal chondrosarcomas often benefit from Ewing sarcoma chemotherapy regimens, while dedifferentiated types respond to osteosarcoma treatment schedules. These exceptions highlight the importance of tailoring treatment to the specific tumor type.
Emerging Treatments
Targeted therapies and clinical trials
Researchers are exploring innovative treatments to improve outcomes for chondrosarcoma. Targeted therapies focus on specific genetic mutations and pathways that drive tumor growth. These therapies aim to disrupt cancer cell activity while minimizing harm to healthy tissues.
Some promising targets include:
Cyclin-dependent kinases, which regulate cell division.
Platelet-derived growth factor receptors and angiogenesis pathways, which support tumor blood supply.
Hedgehog signaling and bone morphogenetic protein-7, both involved in cartilage development.
Molecules like endothelin-1 (ET-1), sphingosine-1-phosphate, and basic fibroblast growth factor.
Tumor suppressor pathways, microRNAs, and the PI3K-Akt-mTOR pathway.
Advances in molecular biology have opened doors to therapies that target these pathways, offering hope for more effective treatments.
Clinical trials are also investigating new approaches, including immunotherapy and combination therapies. Immunotherapy, which harnesses your immune system to fight cancer, has shown promise. For example, studies highlight the role of PD-L1 expression in predicting treatment response. Combining immunotherapy with agents like IDH inhibitors or chemotherapy may enhance effectiveness by addressing tumor heterogeneity and resistance.
One notable development is INBRX-109, a targeted therapy with reduced off-site toxicity. Researchers suggest combining it with other treatments, such as immunotherapy, to improve outcomes. Additionally, multi-omics and genetic testing are helping personalize care by identifying the best treatment options for each patient.
While challenges like treatment resistance remain, these emerging therapies represent a significant step forward. By targeting the unique biology of chondrosarcoma, they offer new hope for patients and their families.
Stay informed about clinical trials and discuss these options with your healthcare provider to explore the latest advancements in treatment.
Prognosis and Factors Influencing Outcomes
Survival Rates
The survival rates for chondrosarcoma depend heavily on the tumor's grade and stage at diagnosis. Low-grade tumors generally have better outcomes, while high-grade and dedifferentiated types show poorer survival rates.
The overall 5-year survival rate for chondrosarcoma patients is 79%, and the 10-year survival rate is 75%.
Low-grade chondrosarcoma has a 5-year survival rate of 83%.
High-grade chondrosarcoma shows a 5-year survival rate of 53%.
Dedifferentiated chondrosarcoma has the lowest 5-year survival rate, ranging from 7% to 24%.
The stage of the tumor also plays a critical role in survival. Localized tumors have significantly better outcomes compared to advanced stages.
Stage of Chondrosarcoma | 5-Year Survival Rate |
|---|---|
Localized | 80% - 90% |
Regional | 75% |
Advanced | 20% |
Factors Affecting Prognosis
Tumor location and size
The location of the tumor greatly influences your prognosis. Tumors in the pelvis are linked to poorer outcomes due to their higher risk of local recurrence. Pelvic chondrosarcomas have 5-year and 10-year survival rates of 50% and 42%, respectively. These tumors often require more aggressive treatment. Larger tumors also tend to have worse outcomes, as they are more challenging to treat effectively.
Patient’s age and overall health
Your age and overall health significantly impact your response to treatment. Patients over 50 years old generally have worse survival outcomes. Younger individuals, particularly those aged 30 to 50, are more likely to be diagnosed with chondrosarcoma. However, younger patients often present with larger tumors and higher histological grades, which can complicate treatment. Maintaining good overall health can improve your ability to tolerate treatments and recover effectively.
Response to treatment
Your response to treatment is another key factor. Early detection and appropriate therapy improve survival rates. Tumors that respond well to surgery or targeted therapies often lead to better outcomes. Discussing treatment options with your healthcare provider ensures you receive the most effective care for your specific case.
Chondrosarcoma presents unique challenges, but understanding its symptoms, diagnosis, and treatment options empowers you to take control of your health. Early detection remains critical. If you notice persistent pain, swelling, or other concerning symptoms, consult a specialist promptly.
Support is available to help you navigate a diagnosis. Organizations like the Chondrosarcoma Foundation and Sarcoma Alliance provide education and advocacy. Online communities, such as Smart Patients and the Sarcoma Oncology Center Private Support Group, connect you with others who share similar experiences. These resources ensure you never face this journey alone.
Staying informed and seeking professional guidance can make a significant difference in your outcomes.
FAQ
What is the most common symptom of chondrosarcoma?
Persistent pain in the affected area is the most common symptom. You may notice the pain worsening over time, even when resting. This discomfort often lasts for months or years before diagnosis.
Can chondrosarcoma spread to other parts of the body?
Yes, high-grade chondrosarcomas can spread to other areas, such as the lungs. Early detection and treatment reduce the risk of metastasis.
Is chondrosarcoma hereditary?
Chondrosarcoma is not usually hereditary. However, certain genetic conditions, like Ollier disease or Maffucci syndrome, may increase your risk.
How can you differentiate chondrosarcoma from other bone conditions?
Doctors use imaging tests like X-rays, MRIs, and biopsies to confirm a diagnosis. These tests help distinguish chondrosarcoma from other bone conditions, such as benign cartilage tumors.
Are there lifestyle changes that can help manage chondrosarcoma?
While lifestyle changes cannot cure chondrosarcoma, maintaining a healthy diet and staying active can support your overall well-being during treatment. Always follow your doctor’s advice.
See Also
Understanding Carcinoid Syndrome: Key Symptoms to Recognize
Cerebellar Astrocytoma Explained: Symptoms You Should Know
Angiosarcoma: An Overview of This Rare Cancer Type
Burkitt's Lymphoma: Symptoms and Important Information to Know

