What is Choriocarcinoma and How is it Treated

Choriocarcinoma is a rare but aggressive cancer that develops in the cells of the placenta. It often arises after pregnancy-related events, such as a normal pregnancy, miscarriage, or molar pregnancy. While uncommon, its incidence varies globally. For example, in Asia, the rate ranges from 5 to 200 cases per 100,000 pregnancies, compared to 2 to 7 cases in Europe and the Americas. Early detection plays a critical role in improving outcomes. With timely treatment, survival rates can reach up to 100%, offering hope to those affected.
Key Takeaways
Choriocarcinoma is a rare cancer that starts in placenta cells after pregnancy.
Finding it early is very important. Treatment can save lives up to 100%.
Symptoms include unusual bleeding and pain in the pelvis. See a doctor if you notice these.
Risks include molar pregnancies, miscarriages, and age. Knowing these helps find it early.
Chemotherapy is the main treatment and works well if caught early.
What is Choriocarcinoma?

Definition and Characteristics
Choriocarcinoma is a rare type of cancer that develops in the cells of the placenta. These cells, called trophoblasts, play a key role in nourishing a developing fetus during pregnancy. Unlike other cancers, this one grows quickly and can spread to other parts of your body, such as the lungs, liver, or brain. Despite its aggressive nature, choriocarcinoma responds well to treatment when detected early.
This cancer is part of a group of conditions known as gestational trophoblastic diseases (GTD). It can occur after various pregnancy-related events, including a normal pregnancy, miscarriage, or molar pregnancy. Its rarity makes it essential for you to recognize symptoms and seek medical advice promptly.
How It Develops
Choriocarcinoma begins when abnormal cells in the placenta grow uncontrollably. These cells invade surrounding tissues and may enter your bloodstream, allowing the cancer to spread to distant organs. This process, known as metastasis, often affects the lungs first. In some cases, it may also involve the brain or liver.
The exact cause of this abnormal growth remains unclear, but it often follows a molar pregnancy, where a nonviable fertilized egg implants in the uterus and forms a tumor instead of a healthy placenta. Understanding how this cancer develops can help you stay vigilant, especially if you have risk factors.
Classification as Gestational Trophoblastic Disease (GTD)
Choriocarcinoma falls under the broader category of gestational trophoblastic diseases. These conditions include both noncancerous and cancerous growths that arise during pregnancy. To help you understand this classification better, here’s a breakdown:
Category | Description |
|---|---|
Gestational Trophoblastic Disease (GTD) | Includes both noncancerous and cancerous tumors that can occur during pregnancy. |
Gestational Trophoblastic Neoplasia (GTN) | Typically cancerous and can spread to other parts of the body; includes choriocarcinoma. |
This classification highlights the importance of distinguishing between benign and malignant forms of GTD. Choriocarcinoma, as part of GTN, requires prompt medical attention due to its potential to spread rapidly.
Causes and Risk Factors of Choriocarcinoma
Common Causes
Choriocarcinoma often develops after specific pregnancy-related events. These include molar pregnancies, miscarriages, and even healthy full-term pregnancies. A molar pregnancy, the most common cause, occurs when abnormal cells grow in the uterus instead of forming a healthy placenta. This condition leads to an overproduction of trophoblast cells, which can become cancerous. Miscarriages and abortions may also trigger the development of this cancer. In rare cases, it can arise after an ectopic pregnancy, where the fertilized egg implants outside the uterus.
The table below summarizes the common causes and their connection to pregnancy events:
Cause of Choriocarcinoma | Relation to Pregnancy Events |
|---|---|
Molar pregnancy | Most common cause due to overproduction of abnormal cells. |
Abortion or miscarriage | Can originate after these events. |
Healthy full-term pregnancy | Can also develop post these pregnancies. |
History of ectopic pregnancy | Increases susceptibility to choriocarcinoma. |
Age factors (under 21 or over 35) | Certain age groups are at higher risk. |
Smoking | Identified as a risk factor. |
High levels of human chorionic gonadotropin | Associated with increased risk during pregnancy. |
Risk Factors
Previous molar pregnancy
If you have experienced a molar pregnancy, your risk of developing choriocarcinoma increases significantly. This condition involves abnormal tissue growth in the uterus, which can later become cancerous. Regular follow-ups after a molar pregnancy are essential to monitor your health.
Age-related risks
Your age can also influence your risk. Women under 21 or over 35 years old face a higher likelihood of developing this cancer. Maternal age above 40 years poses an even greater risk. Staying informed about these age-related factors can help you take preventive measures.
Geographic and ethnic factors
Where you live and your ethnicity may also play a role. Studies show that choriocarcinoma occurs more frequently in certain regions, such as Asia, compared to Europe or the Americas. Socioeconomic and nutritional factors in these areas may contribute to this disparity. Understanding these risks can help you stay vigilant, especially if you belong to a high-risk group.
Note: If you have any of these risk factors, consult your healthcare provider for regular screenings and early detection.
Symptoms of Choriocarcinoma
Early Symptoms
Abnormal vaginal bleeding
One of the earliest signs of choriocarcinoma is abnormal or irregular vaginal bleeding. This bleeding may occur outside of your normal menstrual cycle or persist after a pregnancy-related event, such as a miscarriage or delivery. It often serves as the first noticeable symptom, prompting many individuals to seek medical attention.
These bleeding patterns can resemble other conditions, such as complications from a miscarriage or ectopic pregnancy. However, if you recently experienced a molar pregnancy or other pregnancy-related event, this symptom could indicate choriocarcinoma. Early recognition of this bleeding is crucial for timely diagnosis and treatment.
Pelvic pain or pressure
Pelvic pain or a feeling of pressure in the lower abdomen is another common early symptom. This discomfort may result from the enlargement of the ovaries or the presence of abnormal tissue growth in the uterus. You might notice this pain alongside vaginal bleeding, which can make it more concerning.
While pelvic pain can occur in many conditions, its association with recent pregnancy events, such as a hydatidiform mole, helps distinguish choriocarcinoma from other causes. If you experience persistent pelvic pain, consult your healthcare provider promptly.
Advanced Symptoms
Symptoms of metastasis (e.g., lung or brain involvement)
As choriocarcinoma progresses, it can spread to other parts of your body, such as the lungs or brain. This process, known as metastasis, often leads to additional symptoms. Lung involvement may cause coughing, shortness of breath, or chest pain. If the cancer spreads to the brain, you might experience headaches, dizziness, or even seizures. These symptoms indicate advanced disease and require immediate medical attention.
Fatigue and anemia
Fatigue is a common symptom in advanced cases of choriocarcinoma. You may feel unusually tired or weak, even after resting. This fatigue often results from anemia, a condition where your body lacks enough healthy red blood cells. Anemia can develop due to prolonged vaginal bleeding or the cancer's impact on your overall health. If you notice persistent fatigue, it’s essential to discuss it with your doctor.
Note: Early detection of choriocarcinoma significantly improves treatment outcomes. If you experience any of these symptoms, especially after a recent pregnancy event, seek medical advice without delay.
Diagnosis of Choriocarcinoma
Medical History and Physical Examination
Your medical history plays a critical role in diagnosing choriocarcinoma. Doctors often review past pregnancy-related events, such as molar pregnancies, miscarriages, or ectopic pregnancies, as these increase your risk. They also consider age-related factors, smoking habits, and elevated levels of human chorionic gonadotropin (HCG). The table below highlights key risk factors that may guide your doctor during the diagnostic process:
Risk Factor | Description |
|---|---|
History of molar pregnancy, miscarriage, or ectopic pregnancy | Previous reproductive issues that can increase the risk of choriocarcinoma. |
Pregnancies in women under the age of 21 and over the age of 35 | Age-related risks that may contribute to the development of this cancer. |
Smoking | A lifestyle factor that can elevate the risk of various cancers, including choriocarcinoma. |
High levels of human chorionic gonadotropin (HCG) | Elevated HCG levels can indicate abnormal pregnancy conditions linked to choriocarcinoma. |
During a physical examination, your doctor may perform a pelvic exam to check for an enlarged uterus or other abnormalities.
Diagnostic Tests
Blood tests (e.g., hCG levels)
Blood tests are essential for diagnosing choriocarcinoma. These tests measure your HCG levels, a hormone produced during pregnancy. Abnormally high or persistent HCG levels after a pregnancy-related event often indicate the presence of this cancer. Monitoring these levels helps confirm the diagnosis and track treatment progress.
Imaging tests (e.g., ultrasound, CT, MRI)
Imaging tests provide detailed insights into your condition. A pelvic ultrasound can reveal abnormalities in your uterus or surrounding organs. Advanced imaging techniques, such as CT or MRI scans, help detect tumors and assess their spread. In cases where conventional imaging methods fail, 18 FDG-PET/CT scans can identify metastases, especially in the lungs or brain.
Biopsy and Pathological Analysis
If blood and imaging tests suggest choriocarcinoma, your doctor may recommend a biopsy. This procedure involves collecting a tissue sample from the uterus or other affected areas. Pathologists then analyze the sample under a microscope to confirm the presence of cancerous cells. A biopsy provides definitive evidence, ensuring accurate diagnosis and guiding treatment decisions.
Tip: Early diagnosis improves treatment outcomes. If you experience symptoms or have risk factors, consult your doctor promptly.
Treatment for Choriocarcinoma
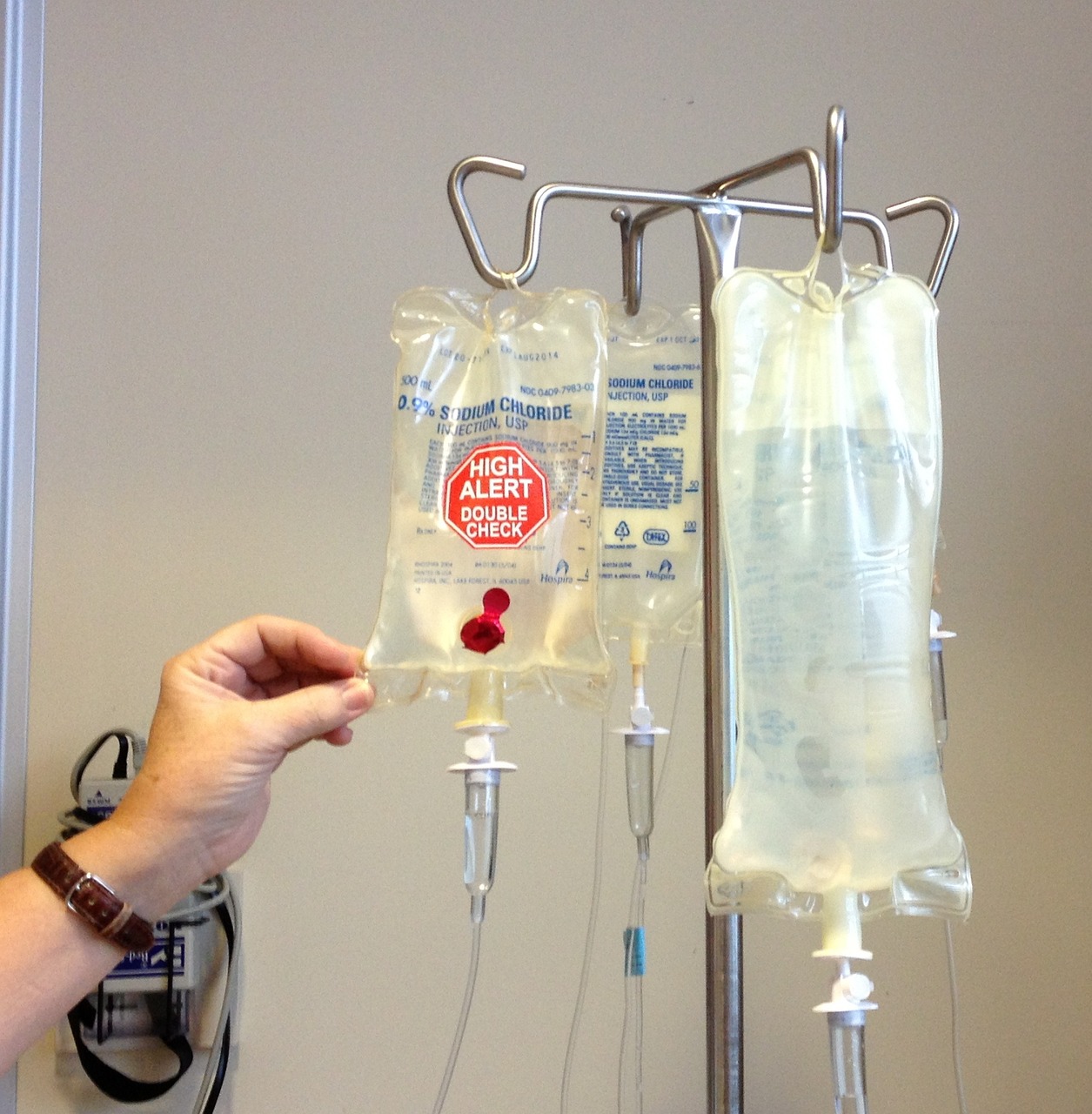
Chemotherapy
First-line treatments
Chemotherapy serves as the primary treatment for choriocarcinoma. It effectively targets cancer cells, stopping their growth and spread. Depending on your condition, doctors may recommend different chemotherapy regimens. Below is a table summarizing common first-line treatments:
Regimen Description | Administration Details |
|---|---|
Charing Cross regimen | Methotrexate (50 mg IM on days 1, 3, 5, and 7) and leucovorin (7.5 mg orally on days 2, 4, 6, and 8) |
Biweekly pulsed dactinomycin | 1.25 mg/m² IV |
Weekly methotrexate | 30 mg/m² IM |
Other regimens | Various combinations of methotrexate and dactinomycin with different dosages and schedules |
These treatments are highly effective, especially when the cancer is detected early. Your doctor will choose the best regimen based on your health and the extent of the disease.
High-risk cases
For high-risk cases, chemotherapy remains the cornerstone of treatment. However, additional interventions may be necessary. The table below outlines options for managing advanced or high-risk choriocarcinoma:
Treatment Type | Description |
|---|---|
Chemotherapy | The main treatment, effective in killing cancer cells or stopping tumor growth. |
Radiation therapy | Rarely used, but may be needed if the tumor has spread to specific areas. |
Surgery | Surgeons may remove the tumor or affected tissues in certain cases. |
Your healthcare team will tailor the treatment plan to address the severity of your condition and ensure the best possible outcome.
Surgery
Hysterectomy
In rare cases, a hysterectomy may be recommended. This procedure involves removing the uterus and is typically reserved for patients who do not respond to chemotherapy or have completed childbearing. Factors such as age, overall health, and personal preferences play a role in this decision.
Treatment Option | Frequency of Use |
|---|---|
Hysterectomy | Rarely needed |
Chemotherapy | Main treatment |
Other surgical options
Other surgical interventions may include removing localized tumors or abnormal tissues. These procedures are less common but can be effective in specific situations. In rare cases, radiation therapy may also be considered as an alternative.
Tip: Surgery is usually a secondary option. Chemotherapy remains the most effective treatment for choriocarcinoma.
Follow-Up Care
Monitoring hCG levels
After completing treatment, regular monitoring of hCG levels is essential. This hormone serves as a marker for choriocarcinoma. Persistent or rising levels may indicate residual cancer, requiring further intervention. Your doctor will schedule periodic blood tests to ensure the cancer has not returned.
Long-term care and fertility considerations
Long-term care focuses on your overall health and well-being. If you wish to have children in the future, discuss fertility preservation options with your doctor before starting treatment. Many patients successfully conceive after treatment, but individual outcomes vary. Emotional support and counseling can also help you navigate this journey.
Note: Consistent follow-up care improves your chances of a full recovery and helps you maintain a good quality of life.
Choriocarcinoma is a rare but treatable cancer that arises from pregnancy-related events. Understanding its causes, symptoms, and treatment options can help you stay informed and proactive. Here are the key takeaways:
This cancer affects about one in 20,000–40,000 pregnancies in the U.S.
Risk factors include molar pregnancy, miscarriage, ectopic pregnancy, and maternal age under 21 or over 35.
Early detection improves outcomes, with an 87.5% chance of remission.
Modern treatments, especially chemotherapy, have proven highly effective. The table below highlights their impact:
Evidence Type | Details |
|---|---|
Treatment Effectiveness | Chemotherapy is usually effective for choriocarcinoma. |
Early Diagnosis Impact | Early diagnosis significantly enhances treatment success. |
Prognosis for Non-Spread | Most women whose cancer has not spread can be cured. |
Remission Rate | About 70% of women with a poor outlook initially go into remission. |
If you experience symptoms or have risk factors, consult your doctor promptly. Early action can save lives and improve your quality of life.
FAQ
What is the survival rate for choriocarcinoma?
The survival rate for choriocarcinoma is high, especially with early detection. When treated promptly, survival rates can reach up to 100%. Even in advanced cases, modern treatments like chemotherapy have significantly improved outcomes, offering hope to most patients.
Can choriocarcinoma affect future pregnancies?
Yes, but many women successfully conceive after treatment. Discuss fertility preservation options with your doctor before starting therapy. Regular follow-ups ensure your health and help you plan for future pregnancies safely.
How long does treatment for choriocarcinoma take?
Treatment duration varies based on the cancer's stage and response to therapy. Most cases require several weeks to months of chemotherapy. Your doctor will monitor your progress and adjust the treatment plan as needed.
Is choriocarcinoma hereditary?
No, choriocarcinoma is not hereditary. It develops from abnormal placental cells during or after pregnancy. However, certain risk factors, like a history of molar pregnancy, may increase your chances of developing it.
What should you do if you suspect choriocarcinoma?
Seek medical attention immediately if you experience symptoms like abnormal vaginal bleeding or pelvic pain after a pregnancy-related event. Early diagnosis improves treatment success and prevents complications.
Tip: Regular follow-ups after pregnancy-related events can help detect issues early and ensure better outcomes.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Carcinoid Syndrome: Key Symptoms To Recognize
Essential Information About Carcinoid Tumors You Need
Anaplastic Large Cell Lymphoma: Overview and Treatment Options
Cervical Cancer: Identifying Symptoms and Understanding Risks

