What is Cutaneous T-Cell Lymphoma and Its Symptoms
Cutaneous T-cell lymphoma is a rare form of non-Hodgkin lymphoma that primarily affects your skin. It accounts for only 5% of all non-Hodgkin lymphoma cases, as shown below:
Category | Percentage |
|---|---|
Cutaneous lymphomas in NHL | 5% |
This condition often begins with subtle skin changes. You might notice red, scaly patches or plaques that feel dry and itchy. These lesions can appear anywhere on your body, even in areas not exposed to sunlight. Itchy skin is particularly common, affecting more than half of those diagnosed.
Early recognition is crucial. If you observe persistent rashes, light spots, or unusual skin changes, consult a healthcare professional promptly. Early detection can lead to better outcomes.
Key Takeaways
Cutaneous T-cell lymphoma is a rare type of skin cancer. It often begins with red, flaky patches on the skin. Finding it early helps improve treatment success.
Common signs include constant itching, redness, and dry spots. These do not get better with usual treatments. See a doctor if you notice these symptoms.
Doctors use skin biopsies and blood tests to check for abnormal T-cells. Catching it early can make treatments work better.
Treatments include creams or ointments for early stages. Advanced cases may need stronger treatments like chemotherapy. Talk to your doctor about all choices.
Understanding Cutaneous T-Cell Lymphoma
What is Cutaneous T-Cell Lymphoma?
Cutaneous T-cell lymphoma is a type of cancer that originates in T-cells, a part of your immune system. Unlike other lymphomas, it primarily affects your skin rather than lymph nodes or internal organs. This condition is classified using systems like EORTC and WHO, which focus on its unique characteristics. For example, the malignant cells in this lymphoma show clonal expansion and resistance to apoptosis, making them distinct from other types of lymphoma.
Characteristic | Cutaneous T-Cell Lymphoma (CTCL) | Other Lymphomas |
|---|---|---|
Localization | Primarily localized to the skin | Can involve lymph nodes and other sites |
Common Immunophenotype | CD4 positive | Varies by lymphoma type |
Subtypes | Mycosis fungoides, Sézary syndrome | Various subtypes based on cell type |
Globally, cutaneous T-cell lymphoma accounts for 83% of primary cutaneous lymphomas. Mycosis fungoides is the most common subtype, representing 62% of cases, while Sézary syndrome accounts for 3%. These numbers vary by region, with a higher prevalence in Asian populations.
Types of Cutaneous T-Cell Lymphoma
Mycosis Fungoides
Mycosis fungoides is the most common form of cutaneous T-cell lymphoma. It typically begins with patches or plaques on your skin that resemble eczema or psoriasis. These lesions often progress slowly over years. Histologically, this subtype is characterized by small to medium-sized T-cells with cerebriform nuclei. Variants of mycosis fungoides include folliculotropic MF and pagetoid reticulosis.
Sézary Syndrome
Sézary syndrome is a more aggressive form of cutaneous T-cell lymphoma. It involves both your skin and blood. You may notice widespread redness, scaling, and severe itching. Blood tests often reveal Sézary cells, which are abnormal T-cells with hyperconvoluted nuclei. Flow cytometry and T-cell receptor gene analysis help confirm the diagnosis.
Diagnostic Method | Description |
|---|---|
Skin Biopsy | Identifies lymphocytes and Pautrier abscesses. |
Blood Evaluation | Detects circulating Sézary cells. |
Flow Cytometry | Highlights atypical lymphocytes with CD7 and CD26 deletion. |
How CTCL Affects the Skin
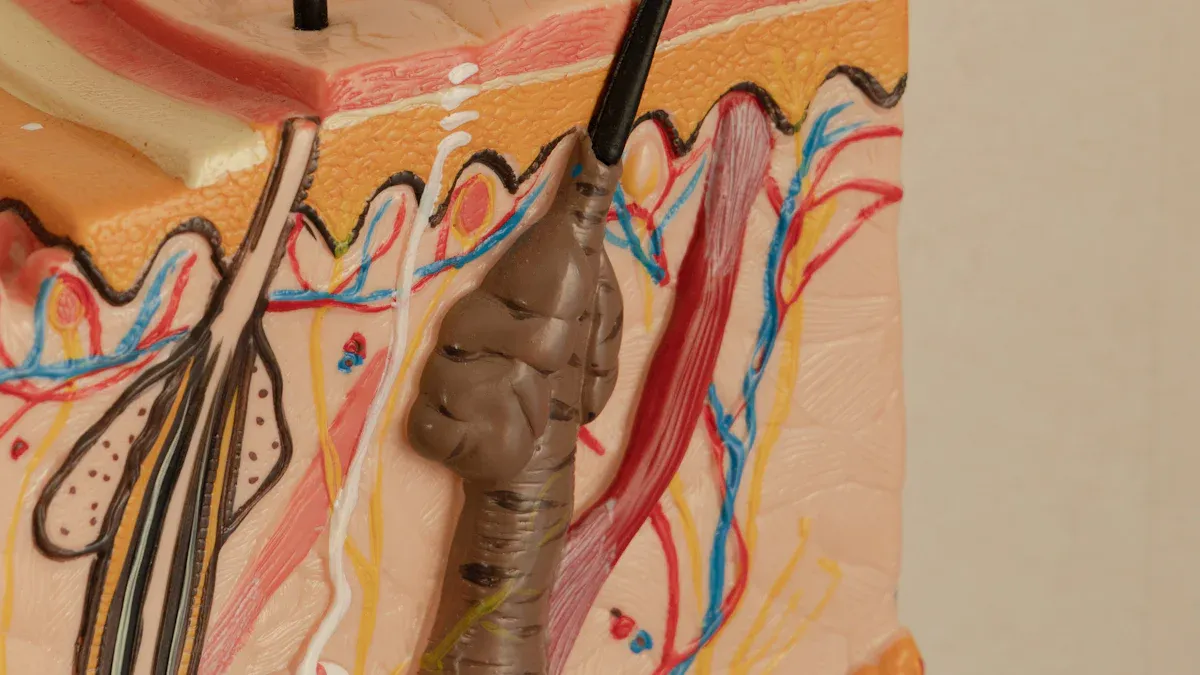
Cutaneous T-cell lymphoma causes various changes in your skin at the cellular level. Malignant T-cells infiltrate the dermis and subcutis, often forming clusters called Pautrier microabscesses. These cells are positive for markers like CD2, CD3, and CD5 but negative for CD7. Over time, they invade blood vessels, leading to tissue necrosis and ulceration. These processes explain why you might experience symptoms like plaques, tumors, or open sores.
Symptoms of Cutaneous T-Cell Lymphoma

Early Symptoms
Dry, scaly patches or plaques
In the early stages of cutaneous T-cell lymphoma, you may notice red, scaly patches or plaques on your skin. These lesions often feel dry and may resemble common skin conditions like eczema or psoriasis. However, unlike these conditions, the patches can appear anywhere on your body, including areas not exposed to sunlight. Persistent symptoms that do not improve with topical treatments, such as corticosteroids, may indicate this type of lymphoma rather than a benign skin issue.
Itching and redness
Itchy skin is one of the most common symptoms, affecting more than half of those diagnosed. The itching can range from mild to intense and may disrupt your sleep. Redness often accompanies the itch, making the affected areas more noticeable. If you experience persistent itching and redness that worsens over time, it’s essential to seek medical advice.
Skin-Related Symptoms
Tumors or nodules
As cutaneous T-cell lymphoma progresses, you might develop thickened plaques or noticeable nodules under your skin. These tumors can vary in size and may feel firm to the touch. They often appear in areas where earlier patches or plaques were present.
Ulceration or open sores
In advanced stages, the skin may break down, leading to ulcers or open sores. These areas can become painful and prone to infections. You might also notice thick, cracked skin on your hands or feet, which can cause discomfort during daily activities.
Systemic Symptoms
Enlarged lymph nodes
Swollen lymph nodes are a key systemic symptom of cutaneous T-cell lymphoma. You may feel lumps under your skin, particularly in areas like your neck, armpits, or groin. These swollen nodes can indicate that the disease is spreading beyond the skin.
Fatigue, weight loss, and fever
Systemic symptoms like fatigue, unexplained weight loss, and fever often appear in advanced stages. You might feel unusually tired or notice a drop in your energy levels. Fever and chills can also occur, signaling that your body is fighting the disease.
If you experience any of these symptoms, consult a healthcare professional promptly. Early diagnosis can improve treatment outcomes and help manage the condition effectively.
Progression of Symptoms in Advanced Stages
Advanced Skin Symptoms
Widespread redness and scaling
In advanced stages of cutaneous T-cell lymphoma, your skin may develop widespread redness and scaling, a condition known as erythroderma. This rash often covers most of your body and feels itchy or uncomfortable. You might also notice thickened skin on your palms and soles, along with abnormalities in your fingernails and toenails. These changes can make daily tasks more challenging. Skin-directed therapies, such as topical steroids or retinoids, can help manage these symptoms. For severe cases, systemic treatments like chemotherapy or phototherapy may be necessary.
Severe itching and discomfort
Severe itching becomes more common as the disease progresses. This itching can disrupt your sleep and significantly impact your quality of life. Persistent scratching may lead to skin infections, further complicating your condition. Topical medications and external beam radiation therapy can provide relief. In some cases, advanced treatments like monoclonal antibodies or oral retinoids may be recommended to reduce inflammation and discomfort.
Systemic Involvement
Blood involvement in Sézary Syndrome
Sézary syndrome, an aggressive form of cutaneous T-cell lymphoma, often involves your blood. You may experience erythroderma, swelling, and enlarged lymph nodes. Other symptoms include hair loss, outward-turning lower eyelids, and trouble regulating body temperature. Blood tests typically reveal Sézary cells, which are abnormal T-cells. This condition can also affect your spleen, lungs, liver, or gastrointestinal tract. Treatments like extracorporeal photopheresis or stem cell transplantation may be considered for refractory cases.
Organ dysfunction
In advanced stages, the disease can spread to your organs, leading to dysfunction. You might notice symptoms like persistent fever, fatigue, and weight loss. Larger skin plaques or tumors may ulcerate, causing pain and secondary infections. The immune system often weakens, increasing your vulnerability to infections. Organ involvement can also result in complications like anemia, edema, or even secondary malignancies. Managing these symptoms requires a combination of systemic therapies and supportive care to improve your overall well-being.
Diagnosis and Treatment Overview
Diagnosing Cutaneous T-Cell Lymphoma
Skin biopsy
A skin biopsy is the most reliable method for diagnosing cutaneous T-cell lymphoma. During this procedure, a small sample of your skin is removed and examined under a microscope. This helps identify abnormal T-cells and confirm the presence of the disease. Early-stage lesions often resemble chronic skin conditions like eczema, making diagnosis challenging. Multiple biopsies may be necessary over time to ensure accuracy.
Blood tests and imaging
Blood tests play a crucial role in assessing the severity of the disease. For example, a complete blood count (CBC) can measure white blood cell levels, which may indicate Sézary syndrome if abnormal T-cells are present in your blood. Additional tests, such as flow cytometry, can detect circulating lymphoma cells. Imaging tests like PET scans help determine whether the cancer has spread to lymph nodes or other tissues. These scans also assist in staging the disease and monitoring treatment progress.
Tip: If you experience persistent skin symptoms, consult a dermatologist. Early diagnosis can improve treatment outcomes.
Treatment Options
Topical therapies
Topical treatments are often the first line of defense for cutaneous T-cell lymphoma. These include creams, ointments, or gels applied directly to affected areas. Common options include topical steroids, retinoids, and chemotherapy agents like mechlorethamine. Psoralen-enhanced light therapy and total body electron beam radiation are also effective for localized skin involvement. While these therapies are generally safe, they may cause side effects like skin thinning, redness, or irritation.
Systemic treatments (e.g., chemotherapy, immunotherapy)
Systemic treatments are used for advanced stages of the disease. Chemotherapy is typically reserved for cases where other therapies have failed or when the cancer has spread. Immunotherapy, including interferons and targeted drugs like vorinostat and romidepsin, offers a less toxic alternative. These treatments aim to control the disease and improve your quality of life. Clinical trials are also exploring new therapies, such as antibody-drug conjugates and cellular therapies, to expand treatment options for aggressive forms like Sézary syndrome.
Note: Discuss all treatment options with your healthcare provider to find the best approach for your condition.
Cutaneous T-cell lymphoma is a rare cancer that primarily affects the skin, often mimicking common conditions like eczema or psoriasis. Early detection plays a vital role in managing this disease. Skin biopsies are essential for confirming the diagnosis, as they help identify cancer cells and guide treatment planning. You should monitor skin changes closely and attend all dermatology appointments. If diagnosed, discuss the stage of the disease with your healthcare provider to explore treatment options. Collaborating with medical professionals ensures timely care and symptom relief, improving your quality of life.
Tip: Seek medical advice promptly if you notice persistent skin changes or unusual symptoms.
FAQ
What causes cutaneous T-cell lymphoma?
The exact cause remains unknown. However, genetic mutations in T-cells and environmental factors may play a role. You might also have a higher risk if you have a weakened immune system or a family history of lymphomas.
Is cutaneous T-cell lymphoma contagious?
No, it is not contagious. You cannot spread it to others through physical contact or shared items. It develops due to changes in your immune cells, not because of an infection.
How is cutaneous T-cell lymphoma different from eczema?
Eczema usually responds to topical treatments and does not involve cancerous cells. Cutaneous T-cell lymphoma, however, persists despite treatment and may progress to form tumors or systemic symptoms. A biopsy can confirm the diagnosis.
Can cutaneous T-cell lymphoma be cured?
Treatment can manage symptoms and slow progression, but a complete cure is rare. Early detection improves outcomes. Your doctor may recommend therapies like topical treatments, phototherapy, or systemic medications based on the stage.
What should you do if you suspect cutaneous T-cell lymphoma?
Consult a dermatologist immediately. Persistent skin changes, itching, or unusual rashes require medical evaluation. Early diagnosis through a biopsy or blood test can help you start treatment sooner.
Tip: Keep track of any skin changes and share them with your doctor during appointments. Early action can make a big difference!
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Burkitt's Lymphoma: Key Symptoms to Recognize
Acute Lymphoblastic Leukemia: Symptoms You Should Know
Identifying Angioimmunoblastic T-Cell Lymphoma Symptoms Easily

