How Cancer Treatments Impact Fertility in Men and Women
Cancer treatments can significantly affect your ability to have children. These effects depend on the type of treatment, your age, and your overall health. For example, certain chemotherapy drugs, like cyclophosphamide, are more likely to cause infertility, especially in women. Older women face a higher risk because they often have fewer eggs remaining, known as a reduced ovarian reserve. Men and women of all ages should consider how treatments might impact their fertility and explore options early. Asking questions like "Do Cancer Treatments Always Cause Infertility? Understanding Your Options" can help you plan for the future.
Key Takeaways
Cancer treatments can harm fertility in men and women. Learning about this helps you plan ahead.
Talk to a fertility doctor before treatment starts. Early talks can help you choose options like freezing eggs or sperm.
Some chemotherapy drugs and radiation may cause infertility. This can be temporary or permanent. Knowing this helps you decide better.
Methods like egg freezing or sperm banking are safe. They do not delay cancer treatment and work for hormone-sensitive cancers.
If infertility happens, methods like IVF or donor eggs/sperm can help you have children.
How Cancer Treatments Affect Fertility in Men

Chemotherapy and Male Fertility
Impact on sperm production and quality
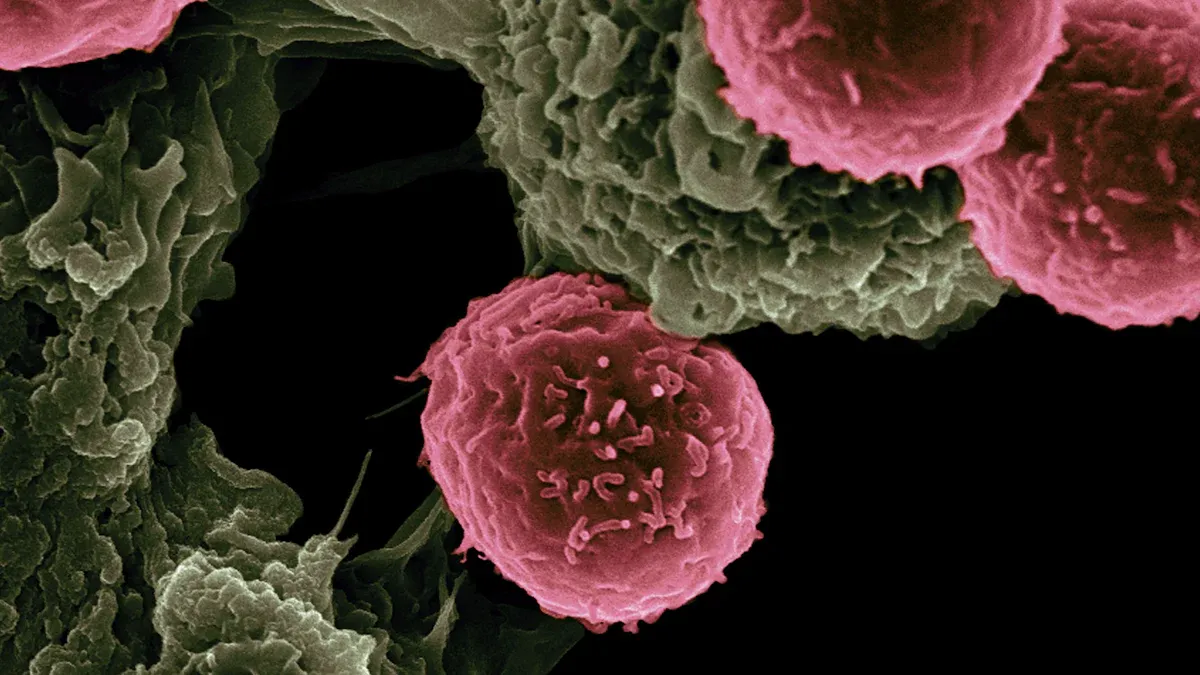
Chemotherapy can significantly affect sperm production and quality. These drugs target rapidly dividing cells, which include sperm-producing cells in your testicles. As a result, sperm counts may drop, and the remaining sperm may have reduced motility or abnormal shapes. This damage can make conception more challenging. Temporary infertility is common, but sperm production may recover over time, depending on the type and dosage of chemotherapy used. However, recovery does not always restore sperm quality to pre-treatment levels.
Risk of permanent infertility with certain drugs
Some chemotherapy drugs carry a higher risk of causing permanent infertility. Medications like cyclophosphamide, cisplatin, and busulfan are particularly gonadotoxic. Higher doses or combining these drugs with radiation therapy increases the likelihood of permanent damage to sperm-forming cells. Advances in cancer treatments have improved survival rates, but the risk of infertility remains a significant concern. Fertility preservation programs can help you plan for the future before starting treatment.
Radiation Therapy and Male Fertility
Effects on testicular function and sperm DNA
Radiation therapy can harm testicular function by damaging the cells responsible for producing sperm and testosterone. Even low doses of radiation directed at the pelvic area can lower sperm counts and impair sperm DNA. This damage may lead to genetic abnormalities in offspring if conception occurs. Shielding the testicles during radiation therapy can reduce these risks, but it does not eliminate them entirely.
Long-term risks of infertility
The long-term effects of radiation therapy on fertility depend on the dose and location of treatment. High doses aimed at the testicles or surrounding areas often result in permanent infertility. Advances in radiation techniques aim to minimize collateral damage, but the gonadotoxic effects remain a challenge. If you are concerned about fertility, discussing options like sperm freezing before treatment can provide peace of mind.
Surgery and Male Fertility
Removal of reproductive organs (e.g., testicles)
Surgical procedures, such as a bilateral orchiectomy (removal of both testicles), result in permanent infertility. This surgery is sometimes necessary to treat testicular cancer or other conditions. Without testicles, your body cannot produce sperm or testosterone, which are essential for reproduction.
Impact on hormone production and fertility
Other surgeries, such as a radical prostatectomy, can also affect fertility. This procedure may lead to retrograde ejaculation, where semen enters the bladder instead of exiting through the penis. Surgeries involving the bladder or urethra can disrupt normal ejaculation pathways, further complicating fertility. If you face surgery, consulting a fertility specialist beforehand can help you understand your options for preserving fertility.
Hormonal Therapies and Male Fertility
Suppression of testosterone and sperm production
Hormonal therapies often aim to block or reduce testosterone levels. These treatments are commonly used for prostate cancer. Lower testosterone levels can stop sperm production temporarily or permanently. Without enough testosterone, your body cannot produce healthy sperm. This suppression can also affect your sex drive and energy levels.
Doctors may prescribe medications like GnRH agonists or anti-androgens to control hormone levels. These drugs work by either stopping testosterone production or blocking its effects. While these therapies are effective for treating cancer, they can significantly impact your fertility. If you plan to have children in the future, you should discuss fertility preservation options with your doctor before starting treatment.
Reversible vs. irreversible effects on fertility
The effects of hormonal therapies on fertility can vary. Some treatments cause temporary infertility. For example, sperm production may resume after stopping the medication. However, the recovery process can take months or even years. The success of recovery depends on factors like your age, overall health, and the duration of treatment.
In some cases, hormonal therapies lead to permanent infertility. Long-term use of certain drugs or combining them with other treatments increases this risk. You should ask your doctor, "Do Cancer Treatments Always Cause Infertility? Understanding Your Options." This question can help you understand whether your fertility might recover or if you need to explore alternatives like sperm freezing.
Tip: Early consultation with a fertility specialist can help you make informed decisions about preserving your fertility before starting hormonal therapy.
How Cancer Treatments Affect Fertility in Women
Chemotherapy and Female Fertility
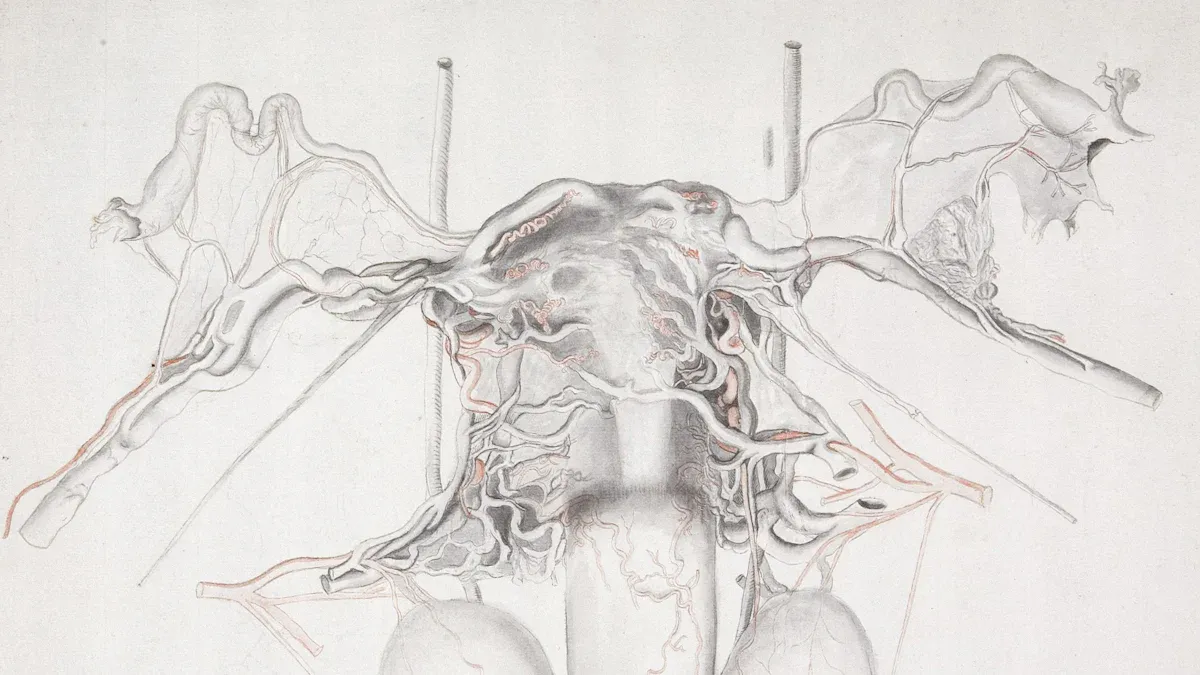
Damage to ovarian reserve and egg quality
Chemotherapy can harm your ovarian reserve, which refers to the number and quality of eggs in your ovaries. These drugs target rapidly dividing cells, including those in your ovaries, leading to a reduction in egg quantity and quality. This damage occurs through mechanisms like DNA cross-links in dormant oocytes, which trigger cell death. Chemotherapy also disrupts ovarian blood flow, further affecting egg health.
Mechanism | Description |
|---|---|
Protein Phosphorylation | Chemotherapy enhances protein activity involved in follicle maturation. |
DNA Damage | It induces DNA cross-links in oocytes, leading to ovarian follicle loss. |
Ovarian Vascularization | It reduces blood flow, impairing ovarian cell functionality. |
Risk of early menopause and infertility
Chemotherapy increases your risk of early menopause, especially if you are older or receive high doses. Early menopause results in infertility because your ovaries stop releasing eggs. Discussing fertility preservation options before treatment can help you plan for the future.
Radiation Therapy and Female Fertility
Effects on ovaries, uterus, and surrounding tissues
Radiation therapy can damage your ovaries and uterus, depending on the dose and location. Even low doses can lead to acute ovarian failure (AOF) or premature ovarian insufficiency (POI). High doses may shrink the uterus, making it harder to carry a pregnancy.
Finding | Description |
|---|---|
Acute Ovarian Failure | Risk increases with radiation dose and age. |
Premature Ovarian Insufficiency | Higher doses lead to increased risk of ovarian dysfunction. |
Uterine Toxicity | Doses above 12 Gy can restrict uterine size. |
Increased risk of miscarriage or complications
Radiation can weaken your uterus, increasing the risk of miscarriage or pregnancy complications. Shielding reproductive organs during treatment can reduce these risks.
Surgery and Female Fertility
Removal of reproductive organs (e.g., ovaries, uterus)
Surgical removal of your ovaries or uterus results in permanent infertility. These procedures are often necessary for treating ovarian or uterine cancers. Without these organs, natural conception becomes impossible.
Impact on hormone levels and menstrual cycles
Surgeries that remove reproductive organs also disrupt hormone production. This disruption can stop your menstrual cycles and lead to symptoms of menopause. If you are concerned about fertility, ask your doctor, "Do Cancer Treatments Always Cause Infertility? Understanding Your Options."
Hormonal Therapies and Female Fertility
Suppression of ovarian function and fertility
Hormonal therapies often suppress ovarian function to slow the growth of hormone-sensitive cancers like breast cancer. Medications such as gonadotropin-releasing hormone (GnRH) agonists temporarily shut down ovarian activity. This suppression reduces estrogen levels, which can stop ovulation and menstrual cycles. While this approach helps treat cancer, it can also affect your ability to conceive.
Some women choose fertility preservation methods before starting hormonal therapy. For example, GnRH agonists are sometimes used to protect ovarian function during treatment. Studies show that 93% of young women with breast cancer discuss fertility with their doctor before therapy. Nearly half take steps to reduce infertility risks, and 31% use GnRH agonists for preservation. These proactive measures can improve your chances of having children after treatment.
Long-term effects on reproductive health
Hormonal therapies can have lasting effects on your reproductive health. Extended use of these treatments may lead to ovarian dysfunction or premature menopause. This can result in permanent infertility, especially if therapy continues for several years. Hormonal changes may also affect your uterine lining, making it harder to sustain a pregnancy.
The impact of hormonal therapies varies depending on your age, health, and treatment duration. Younger women may recover ovarian function after stopping therapy, but older women face a higher risk of permanent damage. Discussing your options early, including asking questions like "Do Cancer Treatments Always Cause Infertility? Understanding Your Options," can help you make informed decisions. Fertility specialists can guide you through preservation techniques and post-treatment evaluations to support your family-building goals.
Tip: Early conversations with your doctor about fertility can help you plan for the future and reduce uncertainty during treatment.
Fertility Preservation Options
For Men
Sperm freezing (cryopreservation)
Sperm freezing is the most common fertility preservation method for men. This process involves collecting and freezing sperm for future use in assisted reproductive technologies like in vitro fertilization (IVF). You can store frozen sperm indefinitely, making it a reliable option if you plan to have children later. Studies show that sperm banking is highly effective, with many men successfully fathering children after cancer treatment.
If you cannot produce a semen sample, doctors may recommend testicular sperm extraction (TESE). This surgical procedure retrieves sperm directly from the testicles and freezes it for future use. TESE provides an alternative for men who face challenges with traditional sperm collection methods.
Testicular tissue freezing for prepubescent boys
For boys who have not yet reached puberty, testicular tissue freezing offers a promising experimental option. This technique involves removing and freezing a small piece of testicular tissue containing sperm-producing cells. Clinical trials are ongoing to determine its effectiveness, but it holds potential for preserving fertility in young boys at high risk of infertility.
For Women
Egg freezing (oocyte cryopreservation)
Egg freezing allows you to preserve unfertilized eggs before starting cancer treatment. Doctors retrieve mature eggs from your ovaries and freeze them for future use. This method is particularly beneficial if you are not ready to start a family but want to keep your options open.
In a study of 425 women with breast cancer, 97 women who underwent fertility preservation later gave birth to at least one child. Among them, 20 used assisted reproductive technologies, demonstrating the success of egg freezing in helping women achieve their family-building goals.
Embryo cryopreservation for future use
Embryo freezing involves fertilizing your eggs with sperm to create embryos, which are then frozen for later use. This method has a higher success rate than egg freezing because embryos are more resilient during the freezing and thawing process. If you have a partner or donor sperm available, this option may be ideal for you.
Other Techniques
Ovarian tissue freezing for young women
Ovarian tissue freezing is an innovative technique where doctors remove and freeze a portion of your ovarian tissue. This tissue can later be re-implanted to restore fertility and hormone production. Although still experimental, this method has shown promise in clinical trials. For example, the NCT01558544 study focuses on advancing ovarian tissue cryopreservation technologies.
Shielding reproductive organs during radiation
If your cancer treatment involves radiation, shielding your reproductive organs can help protect them from damage. Testicular shielding is a common practice for men, while women may benefit from techniques that minimize radiation exposure to the ovaries and uterus. These protective measures reduce the risk of infertility and preserve your ability to conceive naturally.
Note: Fertility preservation techniques like GnRH agonists may also help protect ovarian function during chemotherapy. Studies report higher post-treatment pregnancy rates and lower rates of ovarian insufficiency in patients who used these therapies.
Post-Treatment Fertility Evaluation and Assistance
Fertility Testing After Cancer Treatment
Hormone level assessments for men and women
After cancer treatment, assessing hormone levels helps determine how your reproductive system has been affected. For men, doctors measure testosterone levels to evaluate testicular function. For women, tests focus on hormones like follicle-stimulating hormone (FSH) and estradiol to assess ovarian function. These tests provide insight into whether your body can still produce healthy sperm or eggs.
Semen analysis and ovarian reserve testing
Semen analysis evaluates sperm count, motility, and shape to determine male fertility. For women, ovarian reserve testing measures the quantity and quality of eggs remaining in your ovaries. This includes blood tests for anti-Müllerian hormone (AMH) and antral follicle count (AFC) through ultrasound. These evaluations help you understand your fertility status and plan for future family-building options.
Category | Evidence |
|---|---|
Effects of Cancer Treatment | Some cancers and treatments can affect fertility, with effects being temporary or permanent. |
Fertility Preservation Options | Options include menstrual suppression, ovary shielding, egg freezing, and embryo freezing. |
Factors Influencing Fertility | Type and dose of chemotherapy, age, and ovarian reserve are key factors affecting fertility. |
Recommendations | Oncologists should discuss fertility preservation with patients before treatment begins. |
Assisted Reproductive Technologies (ART)
In vitro fertilization (IVF) and related options
IVF offers a way to conceive if natural conception is not possible. This process involves fertilizing eggs with sperm in a lab and transferring the resulting embryos into the uterus. If you preserved eggs or embryos before treatment, IVF can help you achieve pregnancy later.
Use of donor eggs, sperm, or embryos
If your fertility is permanently affected, using donor eggs, sperm, or embryos provides another option. Many cancer survivors successfully build families through these methods. A study found that among 425 women with breast cancer who preserved fertility, 20 used assisted reproductive technologies to conceive. This highlights the importance of exploring preservation options early.
Emotional and Psychological Support
Counseling for fertility-related concerns
Fertility challenges after cancer treatment can feel overwhelming. Counseling helps you process these emotions and make informed decisions about your options. Speaking with a fertility counselor can reduce anxiety and provide clarity about your next steps.
Support groups and resources for cancer survivors
Joining support groups connects you with others who share similar experiences. These groups offer emotional support and practical advice for navigating fertility concerns. Addressing these issues early can reduce future regret and dissatisfaction.
Evidence Type | Findings |
|---|---|
Fertility Concerns | Addressing fertility concerns can reduce future regret and dissatisfaction among women with cancer. |
Tip: Asking questions like "Do Cancer Treatments Always Cause Infertility? Understanding Your Options" can guide you toward the right resources and support.
Do Cancer Treatments Always Cause Infertility? Understanding Your Options
Factors Influencing Fertility Outcomes
Type and dosage of treatment
The type and dosage of cancer treatment play a major role in determining fertility outcomes. Chemotherapy drugs like cyclophosphamide are known to have a high likelihood of causing infertility. Higher doses of these medications increase the risk of damaging reproductive cells. Radiation therapy, especially when directed at the pelvic area, can also harm reproductive organs. Shielding techniques and fertility preservation methods, such as egg or sperm freezing, can help reduce these risks.
Factor | Description |
|---|---|
Type of chemotherapy | Certain chemotherapies, like cyclophosphamide, have a high probability of causing infertility. |
Dose of chemotherapy | Higher doses may increase the risk of infertility. |
Age and ovarian reserve | Older women have less ovarian reserve, making them more susceptible to fertility issues. |
Fertility preservation options | Options include menstrual suppression, ovary shielding, egg freezing, and embryo freezing. |
Age and overall health of the patient
Your age and overall health significantly influence how cancer treatments affect fertility. Younger individuals often have a better chance of recovering fertility after treatment. Women with a higher ovarian reserve may experience less damage to their eggs. However, older women face a greater risk of infertility due to a naturally reduced ovarian reserve. Maintaining good overall health before and during treatment can improve your chances of preserving fertility.
Temporary vs. Permanent Infertility
Recovery of fertility after treatment
Fertility recovery depends on the type of treatment and your body’s ability to heal. Some treatments cause temporary infertility, allowing you to conceive once your reproductive system recovers. For example, sperm production in men may resume months or years after chemotherapy. Women may regain ovarian function if their eggs were not severely damaged. Fertility preservation methods, such as ovarian tissue freezing, can also support recovery.
Options for addressing infertility
If cancer treatments result in permanent infertility, you still have options for building a family. Assisted reproductive technologies, such as in vitro fertilization (IVF), can help you conceive using preserved eggs, sperm, or embryos. Donor eggs, sperm, or embryos provide another path to parenthood. Fertility preservation methods do not delay cancer treatment and are safe, even for hormonally sensitive cancers. Discussing these options with your doctor early ensures you can make informed decisions.
Tip: Fertility counseling is essential. Studies show that many young women with breast cancer do not receive adequate counseling, even though fertility preservation does not delay treatment or increase cancer recurrence risks.
Cancer treatments can affect your fertility, but many preservation and post-treatment options exist. Early consultation with fertility specialists improves your chances of achieving family-building goals.
93% of women who received fertility counseling before treatment showed greater awareness of fertility issues.
Fertility concerns influenced treatment decisions, such as shortening endocrine therapy.
These findings highlight the importance of discussing fertility early. With the right support and resources, you can plan for the future and make informed decisions about your reproductive health.
Tip: Speak with a fertility specialist before starting treatment to explore your options.
FAQ
What is the best time to discuss fertility preservation with your doctor?
You should talk to your doctor about fertility preservation before starting cancer treatment. Early discussions allow you to explore options like egg or sperm freezing and make informed decisions about your future family-building goals.
Can fertility preservation delay cancer treatment?
Most fertility preservation methods, like egg or sperm freezing, do not delay cancer treatment. Doctors often coordinate these procedures to ensure they fit within your treatment timeline without compromising your health.
Are fertility preservation methods safe for hormone-sensitive cancers?
Yes, many fertility preservation techniques are safe for hormone-sensitive cancers. For example, ovarian tissue freezing and shielding reproductive organs during radiation do not involve hormone stimulation, making them suitable for these cases.
How long can frozen eggs, sperm, or embryos be stored?
Frozen eggs, sperm, and embryos can be stored indefinitely. Studies show that their quality remains stable over time, allowing you to use them whenever you are ready to start a family.
What if cancer treatment causes permanent infertility?
If treatment causes permanent infertility, you can still build a family using donor eggs, sperm, or embryos. Assisted reproductive technologies like IVF also provide options for achieving parenthood after cancer.
Tip: Always consult a fertility specialist to understand your options and make the best decisions for your situation.
See Also
Understanding Choriocarcinoma: Treatment Options and Insights
Essential Information About Embryonal Carcinoma You Should Know
Endometrial Cancer: Symptoms and Important Information to Know
Recognizing Duodenal Cancer: Symptoms and Available Treatments
Fallopian Tube Cancer: Causes and Symptoms You Must Recognize

