Does Cancer Only Affect Poor Lifestyles? Genetics Matter
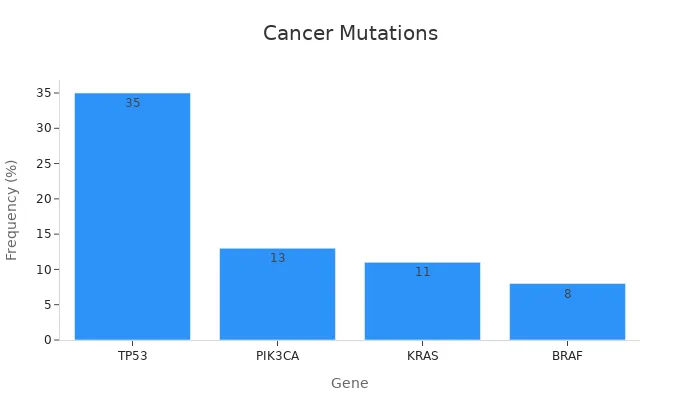
Cancer develops when cells grow uncontrollably, often due to genetic mutations. These mutations can be inherited or acquired over time. For example, TP53, the most commonly mutated gene, appears in 35% of all cancers, while KRAS mutations occur in 11%. Such genetic changes can significantly increase your risk, even if you lead a healthy lifestyle. This raises the question: Does cancer only affect people with poor lifestyles? The role of genetics and environment is crucial in understanding cancer development. However, research shows that lifestyle choices, like avoiding smoking and staying active, can help reduce this risk. This highlights the complex relationship between genetics and environment in cancer development.
Key Takeaways
Cancer can happen because of gene changes, not just bad habits. This explains why even healthy people can get cancer.
Some gene changes, like BRCA1 and BRCA2, raise cancer risk a lot. Knowing your family history can help prevent cancer.
Good habits, like not smoking and exercising, lower cancer risk. Staying healthy helps but doesn’t remove all risks.
Genetic tests can show if you might get certain cancers. This helps you make smart health choices and get checked early.
Special treatments match cancer care to your genes. This can make treatments work better and cause fewer problems.
What Is Cancer and How Do Genetics Contribute to Its Development?

The Basics of Cancer
Uncontrolled cell growth and its causes
Cancer begins when cells in your body grow uncontrollably. Normally, cells divide in a regulated way to replace old or damaged ones. However, when this process goes wrong, cells can multiply without stopping, forming tumors. These tumors may invade nearby tissues or spread to other parts of your body. This uncontrolled growth often starts with changes in your DNA, which acts as the instruction manual for your cells.
The role of DNA and genetic mutations in cancer
DNA contains genes that control how your cells function, grow, and divide. When mutations occur in these genes, they can disrupt normal cell behavior. Some mutations happen randomly, while others result from environmental factors like UV radiation or smoking. For example, mutations in the TP53 gene, a major tumor suppressor, are common in many cancers. These genetic changes can either activate cancer-promoting genes or disable protective ones, leading to the development of cancer.
How Genetic Mutations Lead to Cancer
Mutations in tumor suppressor genes
Tumor suppressor genes act as your body's natural defense against cancer. They regulate cell growth and repair damaged DNA. When mutations disable these genes, cells lose their ability to control growth. For instance, TP53 mutations are found in various cancers and play a critical role in tumor formation. Without functioning tumor suppressors, your cells can grow unchecked, increasing the risk of cancer.
Mutations in oncogenes and their effects
Oncogenes are genes that, when mutated, drive cancer development. Unlike tumor suppressor genes, oncogenes promote cell division. Mutations in oncogenes, such as KRAS or BRAF, can cause cells to divide uncontrollably. For example, BRAF mutations are frequently seen in melanoma, while KRAS mutations are common in adenocarcinomas. These genetic changes create a cascade of signals that fuel cancer growth.
Gene | Cancer Type | Mutation Frequency | Significance in Cancer Development |
|---|---|---|---|
BRAF | Melanoma | Most frequently mutated | Key role in melanoma development |
TP53 | Various cancers | Commonly mutated | Major tumor suppressor gene |
KRAS | Adenocarcinoma | Most frequently mutated | Promotes cancer in specific contexts |
Genetic mutations, whether in tumor suppressor genes or oncogenes, highlight the complex relationship between genetics and cancer. This interplay explains why some individuals develop cancer despite leading healthy lifestyles, as explored in the question, "Does Cancer Only Affect People with Poor Lifestyles? The Role of Genetics and Environment."
Inherited vs. Acquired Genetic Mutations
What Are Inherited Mutations?
Examples of hereditary cancers (e.g., BRCA1/BRCA2 in breast cancer)
Inherited mutations are genetic changes passed from parent to child. These mutations are present from birth and can significantly increase your risk of developing certain cancers. For example, mutations in the BRCA1 and BRCA2 genes are strongly linked to hereditary breast and ovarian cancers. If you inherit one of these mutations, your lifetime risk of developing breast cancer can rise to 45-65%. Similarly, Lynch syndrome, caused by inherited mutations in DNA mismatch repair genes, increases your risk of colorectal and endometrial cancers. These examples highlight how inherited mutations can predispose you to specific cancer types.
How inherited mutations increase cancer risk
Inherited mutations disrupt the normal function of genes that protect your body from cancer. For instance, tumor suppressor genes like BRCA1 and BRCA2 help repair damaged DNA. When these genes are mutated, your cells lose their ability to fix DNA errors, leading to uncontrolled growth. This increases your susceptibility to cancer, even if you maintain a healthy lifestyle. While inherited mutations are less common than acquired ones, they play a critical role in hereditary cancers.
Type of Mutation | Description | Prevalence in Cancer Types |
|---|---|---|
Inherited Mutations | Present from birth, can increase cancer risk, passed from parent to child. | Associated with hereditary cancers. |
What Are Acquired Mutations?
Environmental and lifestyle factors that cause mutations
Acquired mutations develop over your lifetime due to environmental exposures or lifestyle choices. Factors like smoking, UV radiation, and exposure to toxins can damage your DNA, leading to mutations. For example, smoking introduces harmful chemicals that directly alter your DNA, increasing your risk of lung cancer. Similarly, prolonged sun exposure can cause mutations in skin cells, leading to melanoma. These mutations accumulate over time, making age another significant factor in cancer development.
The difference between inherited and acquired mutations
Unlike inherited mutations, acquired mutations are not present at birth. They occur in specific cells and are not passed to your children. While inherited mutations are linked to hereditary cancers, acquired mutations are more common in sporadic cancers. For instance, TP53 mutations, which occur in 35% of all cancers, are often acquired due to environmental factors. The table below highlights key differences between these mutation types:
Type of Mutation | Origin | Environmental Influences | Incidence Characteristics |
|---|---|---|---|
Inherited Mutations | Present from birth | Less influenced by environment; genetic factors | Higher risk of hereditary cancers |
Acquired Mutations | Develop over a lifetime | Influenced by aging, toxins, and viruses | Associated with sporadic cancers, lower initial risk |
Understanding the distinction between inherited and acquired mutations helps you grasp why cancer can affect individuals with healthy lifestyles. This interplay between genetics and environment is central to answering the question, "Does Cancer Only Affect People with Poor Lifestyles? The Role of Genetics and Environment."
Does Cancer Only Affect People with Poor Lifestyles? The Role of Genetics and Environment

The Role of Lifestyle in Cancer Risk
Smoking, diet, and other modifiable risk factors
Your lifestyle choices can significantly influence your cancer risk. Smoking, for instance, is one of the most well-documented causes of cancer. It increases the likelihood of developing lung, laryngeal, and oral cancers by several folds. Poor dietary habits, such as consuming processed foods and sugary drinks, also contribute to cancer risk. On the other hand, maintaining a healthy weight and staying physically active can lower your chances of developing cancer. Studies show that weight loss and increased physical activity reduce cancer incidence, especially among middle-aged adults.
Organizations like the World Health Organization and the American Cancer Society emphasize that adopting healthy habits can prevent many cancers. However, they also acknowledge that cancer causation is complex, involving both genetic and environmental factors. While lifestyle changes can reduce cancer mortality, they are not the sole determinant of your risk.
How lifestyle choices can trigger genetic mutations
Certain lifestyle factors can directly damage your DNA, leading to genetic mutations that may cause cancer. Smoking introduces harmful chemicals into your body, which can alter the DNA in your lung cells. Similarly, excessive sun exposure can damage the DNA in your skin cells, increasing the risk of melanoma. These mutations accumulate over time, making lifestyle choices a critical factor in cancer prevention. However, even with a healthy lifestyle, genetic predispositions can still play a role in cancer development.
The Interplay Between Genetics and Lifestyle
Why some people with healthy lifestyles still develop cancer
You might wonder why some individuals who follow healthy lifestyles still develop cancer. The answer lies in genetics. Inherited mutations, such as those in the BRCA1 and BRCA2 genes, can significantly increase your cancer risk regardless of your lifestyle. These genetic factors can override the protective effects of healthy habits, making cancer prevention more challenging for some individuals.
How genetic predisposition amplifies or mitigates lifestyle risks
Your genetic makeup can influence how lifestyle factors affect your cancer risk. For example, someone with a genetic predisposition to lung cancer may face an even higher risk if they smoke. Conversely, a person without such a predisposition might not develop cancer despite similar habits. This interplay between genetics and lifestyle highlights the importance of understanding your genetic risk. Genetic testing can help you identify potential vulnerabilities and take proactive steps to reduce your overall risk.
Lifestyle Factor | Cancer Type | Increased Risk |
|---|---|---|
Tobacco Smoking | Lung | Several folds |
Tobacco Smoking | Laryngeal | Several folds |
Tobacco Smoking | Oral Cancer | Several folds |
Poor Diet | Colorectal | Increased risk |
Physical Inactivity | Various types | Increased risk |
Understanding the relationship between genetics and lifestyle can help you make informed decisions about your health. While lifestyle changes are essential, they are only one piece of the puzzle in answering the question, "Does Cancer Only Affect People with Poor Lifestyles? The Role of Genetics and Environment."
Implications of Genetic Predisposition for Prevention and Treatment
Prevention and Early Detection
Genetic testing and its benefits
Genetic testing helps you understand your risk of developing certain cancers. It identifies mutations in genes like BRCA1, BRCA2, or TP53, which are linked to hereditary cancers. Knowing your genetic risk allows you to take proactive steps, such as lifestyle changes or regular screenings. For example, if you carry a BRCA mutation, you might consider preventive measures like increased monitoring or even surgery to reduce your risk.
Tip: Speak with a genetic counselor before undergoing testing. They can help you understand the results and guide you on the next steps.
Genetic testing empowers you to make informed decisions about your health. It also helps your family members, as they can assess their own risks based on your results.
Screening programs for high-risk individuals
If you have a higher genetic risk, screening programs can detect cancer early when it is most treatable. For instance, women with BRCA mutations often undergo regular mammograms or MRIs starting at a younger age. Similarly, individuals with Lynch syndrome may benefit from frequent colonoscopies to catch colorectal cancer early.
Screening programs are tailored to your specific risk factors. They provide a critical safety net, especially for those with inherited mutations. Early detection improves survival rates and reduces the burden of advanced treatments.
Advances in Treatment
Personalized medicine and targeted therapies
Personalized medicine tailors treatments to your unique genetic profile. Targeted therapies focus on specific mutations driving cancer growth. For example, drugs like PARP inhibitors work effectively in cancers with BRCA mutations. These therapies minimize damage to healthy cells, reducing side effects compared to traditional treatments.
Note: Personalized medicine is transforming cancer care by offering more precise and effective treatment options.
By understanding your genetic makeup, doctors can choose treatments that are most likely to succeed. This approach improves outcomes and enhances your quality of life during treatment.
The role of genetic research in improving outcomes
Genetic research continues to uncover new ways to fight cancer. Scientists are identifying more mutations linked to cancer, leading to the development of innovative therapies. For example, immunotherapy, which boosts your immune system to fight cancer, has shown promise in treating genetically driven cancers.
Ongoing research also improves prevention strategies. It helps refine screening guidelines and identifies new targets for treatment. As genetic knowledge grows, you benefit from more effective and less invasive options.
Understanding the role of genetics in cancer prevention and treatment highlights the complexity of the question, "Does Cancer Only Affect People with Poor Lifestyles? The Role of Genetics and Environment." While lifestyle changes are important, genetic predisposition plays a significant role in shaping your risk and treatment options.
While your lifestyle choices influence cancer risk, genetics often play a dominant role in its development. Understanding this genetic basis empowers you to take proactive steps, such as genetic testing and early screenings, to reduce your risk. Advances in research and personalized medicine offer hope for better outcomes.
Adopting multiple healthy habits can lower cancer risk by 29% and reduce cancer mortality by 52%.
However, genetic predispositions may override these benefits, making awareness of your genetic profile essential.
By combining healthy habits with genetic insights, you can take control of your health and improve your chances of early detection and effective treatment.
FAQ
What role does family history play in cancer risk?
Family history can indicate a higher risk of inherited genetic mutations, such as BRCA1 or BRCA2. If close relatives have had cancer, you might carry similar mutations. Genetic testing can help you understand your risk and take preventive measures.
Can lifestyle changes completely prevent cancer?
Lifestyle changes, like quitting smoking or eating healthy, reduce your risk but don’t guarantee prevention. Genetic predispositions may still lead to cancer. Combining healthy habits with regular screenings offers the best protection.
Should you consider genetic testing if no one in your family has cancer?
Yes, even without a family history, genetic testing can identify mutations that increase your risk. Some mutations occur spontaneously and aren’t inherited. Testing helps you make informed decisions about prevention and early detection.
How does age affect cancer risk?
As you age, your cells accumulate more mutations, increasing your cancer risk. Regular screenings become more important with age, especially if you have a genetic predisposition or other risk factors.
Are all cancers caused by genetic mutations?
Yes, all cancers involve genetic mutations. However, these mutations can be inherited or acquired. Environmental factors, like smoking or UV exposure, often cause acquired mutations. Understanding the type of mutation helps guide prevention and treatment strategies.
Tip: Stay proactive with regular check-ups and screenings to catch potential issues early.
See Also
Exploring Cancer Types Associated With AIDS Infection
Identifying Causes and Risks of Lung Adenocarcinoma
Recognizing Symptoms and Causes Associated With Anal Cancer
Key Features and Insights Into Cholangiocarcinoma Explained
Simplifying B-Cell Prolymphocytic Leukemia: What You Need to Know

