Why Do Some Cancers Spread Faster Than Others?
Cancer spreads at different speeds depending on its unique biology. Genetic mutations can make cancer cells more aggressive, allowing them to invade nearby tissues. The tumor microenvironment, including surrounding cells and blood vessels, also plays a role in supporting or limiting growth. Your immune system may either fight cancer or unintentionally help it spread. You might wonder, does cancer always spreads quickly? The answer depends on the type of cancer and how it interacts with your body. Understanding these factors can help researchers develop better treatments.
Key Takeaways
Cancer spreads at different speeds depending on its type and genes. Knowing these differences helps create better treatments.
Metastasis happens in three steps: invasion, circulation, and colonization. These steps let cancer cells move to new body parts.
Fast-growing cancers, like pancreatic and small cell lung cancer, spread quickly. This makes them harder to treat. Finding them early is very important.
The tumor's surroundings, like blood vessels and nearby cells, help it grow. Changing this environment can slow cancer spread.
Treatments based on genetic tests can help people live longer. Targeted therapies attack specific mutations to fight cancer better.
What Is Metastasis?
Defining Metastasis
The process of cancer spreading to other parts of the body.
Metastasis occurs when cancer cells move from their original location to other parts of your body. This process makes cancer more dangerous and harder to treat. Once cancer spreads, it can affect vital organs like your lungs, liver, or brain. Doctors often use specific benchmarks to classify metastatic cancer. For example, the STARS staging system categorizes metastatic disease into stages IVA through E, based on factors like tumor location, age, and sex. These classifications help guide treatment decisions and predict outcomes.
Definition/Benchmark | Description |
|---|---|
STARS Staging System | A novel staging system that classifies metastatic disease into Stages IVA-E, accounting for site, tumor, age, race, and sex. |
Long-term Survivorship | Certain subgroups of patients with metastatic cancer are living longer due to advancements in metastases-directed therapy, particularly in low metastatic burden cases. |
Key steps in metastasis: invasion, circulation, and colonization.
Metastasis involves three main steps. First, cancer cells invade nearby tissues by breaking through barriers like the basement membrane. Next, they enter your bloodstream or lymphatic system, which acts as a highway for cancer cells to travel. Finally, these cells colonize new areas by attaching to tissues and forming secondary tumors. Each step requires cancer cells to adapt and survive in different environments.
Mechanisms of Metastasis
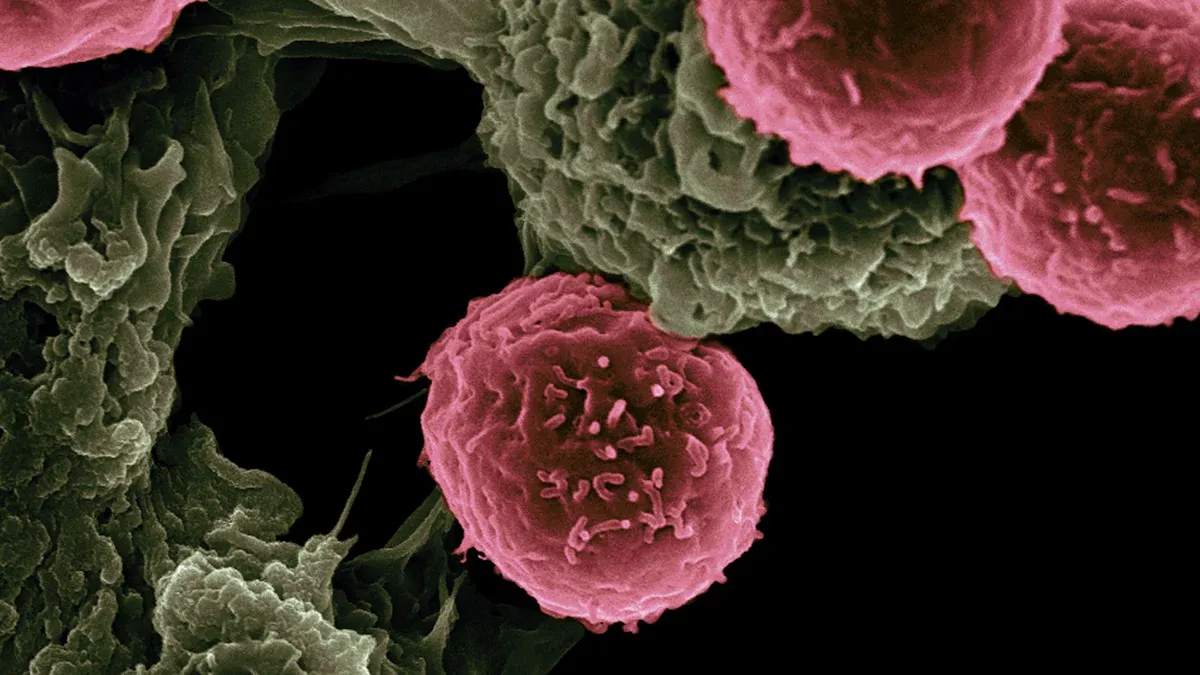
How cancer cells detach from the primary tumor.
Cancer cells detach from the primary tumor by losing adhesion to neighboring cells. They produce enzymes that break down surrounding tissues, allowing them to escape. This ability to detach and invade is a hallmark of aggressive cancers, such as pancreatic and melanoma, which are known for their high metastatic potential.
The role of the bloodstream and lymphatic system in cancer spread.
Your bloodstream and lymphatic system play a critical role in metastasis. These systems transport cancer cells to distant organs. Some cancers, like breast and kidney cancer, show an increasing incidence of metastasis. However, others, such as lung and liver cancers, are decreasing in metastatic cases.
Cancers with increasing metastatic incidence:
Esophageal (APC = 0.45)
Pancreatic (APC = 1.66)
Kidney (APC = 0.40)
Melanoma of the skin (APC = 2.53)
Breast (APC = 1.84)
Cancers with decreasing metastatic incidence:
Lung (APC = -3.44)
Liver and intrahepatic bile duct (APC = -1.14)
Ovaries (APC = -1.62)
Prostate (APC = -1.28)
Understanding how cancer spreads can help you recognize the importance of early detection and targeted treatments.
Does Cancer Always Spreads Quickly?
Differences in Cancer Growth Rates
Slow-growing cancers vs. aggressive cancers.
Not all cancers grow or spread at the same speed. Some cancers, like prostate or thyroid cancer, grow slowly and may remain localized for years. These cancers often have high survival rates when detected early. On the other hand, aggressive cancers, such as small cell lung cancer or pancreatic cancer, grow and spread rapidly. These types are more challenging to treat and often lead to poorer outcomes.
The survival rates for slow-growing cancers highlight their less aggressive nature. For example:
Cancer Type | |
|---|---|
Prostate Cancer | High (exact percentage not specified) |
Thyroid Cancer | 98–100% at stages 1 and 2 |
Testicular Cancer | 99% for localized tumors |
Cervical Cancer | 92% for localized stages |
Hodgkin Lymphoma | 92-95% at stage 1 and 2 |
These statistics emphasize the importance of early detection and treatment for improving outcomes, especially for slow-growing cancers.
Examples of cancers with varying growth rates.
Small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC) provide a clear example of how growth rates differ. SCLC grows quickly and often spreads before diagnosis, making it more dangerous. In contrast, NSCLC grows more slowly, giving doctors more time to intervene. Understanding these differences helps you see why some cancers require more urgent treatment than others.
Factors Influencing Growth Speed
Genetic damage and differentiation levels in cancer cells.
The speed of cancer growth often depends on the genetic makeup of the cancer cells. Mutations in certain genes can make cells grow uncontrollably. For instance, high levels of the protein NUAK2 are linked to aggressive cancers. This protein boosts cell proliferation, making tumors grow faster. Researchers are exploring ways to target NUAK2 to slow cancer growth and improve treatment options.
Accessibility of nutrients and metabolic changes in tissues.
Cancer cells need nutrients to grow. Tumors in areas with abundant blood supply often grow faster because they have easy access to oxygen and nutrients. Metabolic changes in cancer cells also play a role. These cells adapt to survive in low-oxygen environments, allowing them to thrive even when resources are limited. This adaptability makes aggressive cancers harder to control.
By understanding these factors, you can better grasp why some cancers spread quickly while others grow more slowly. Asking "Does cancer always spreads quickly?" depends on the type of cancer and its unique biology.
Factors That Influence the Speed of Cancer Spread
Cancer Type and Aggressiveness
How cancer type determines metastatic potential.
The type of cancer you have plays a major role in how quickly it spreads. Some cancers, like pancreatic cancer, are highly aggressive and have a greater ability to invade other tissues. Others, such as prostate cancer, tend to grow more slowly and remain localized for longer periods. The odds of long-term survivorship also vary depending on the cancer type. For example, lung and bronchus cancers show the highest odds ratio for survival compared to other types.
Cancer Type | Odds Ratio of Long-Term Survivorship (2013) | Incidence Trend |
|---|---|---|
Lung and Bronchus | Highest | |
Colon and Rectum | 2.62 | High |
Breast | 2.04 | High |
Overall | - | Increasing trend |
Examples of highly aggressive cancers (e.g., pancreatic, melanoma).
Highly aggressive cancers, such as pancreatic cancer and melanoma, often spread quickly and are harder to treat. Pancreatic cancer, for instance, had an incidence rate of 6.85 per 100,000 in 2015, which is predicted to rise to 7.20 per 100,000 by 2040. This increase highlights the need for early detection and targeted therapies. In contrast, less aggressive cancers like colon and rectum cancers show a declining trend in incidence rates.
Cancer Type | Incidence Rate (2015) | Predicted Incidence Rate (2040) |
|---|---|---|
Lung and Bronchus | 27.8 per 100,000 | 7.80 per 100,000 |
Colon and Rectum | 8.48 per 100,000 | 4.17 per 100,000 |
Pancreatic Cancer | 6.85 per 100,000 | 7.20 per 100,000 |
Genetic Mutations and Molecular Drivers
The role of specific gene mutations in promoting metastasis.
Certain genetic mutations can make cancer cells more likely to spread. These mutations alter how cells grow and divide, giving them the ability to invade other tissues. For example, mutations in the TP53 gene, often called the "guardian of the genome," can lead to uncontrolled cell growth. This makes cancers with such mutations more aggressive and harder to treat.
Proteins like VEGF and their impact on cancer spread.
Proteins like VEGF (vascular endothelial growth factor) play a critical role in cancer spread. VEGF promotes the growth of new blood vessels, which supply tumors with oxygen and nutrients. This process, known as angiogenesis, allows cancer cells to thrive and spread to other parts of your body. Targeting VEGF has become a key strategy in slowing the spread of aggressive cancers.
Tumor Microenvironment
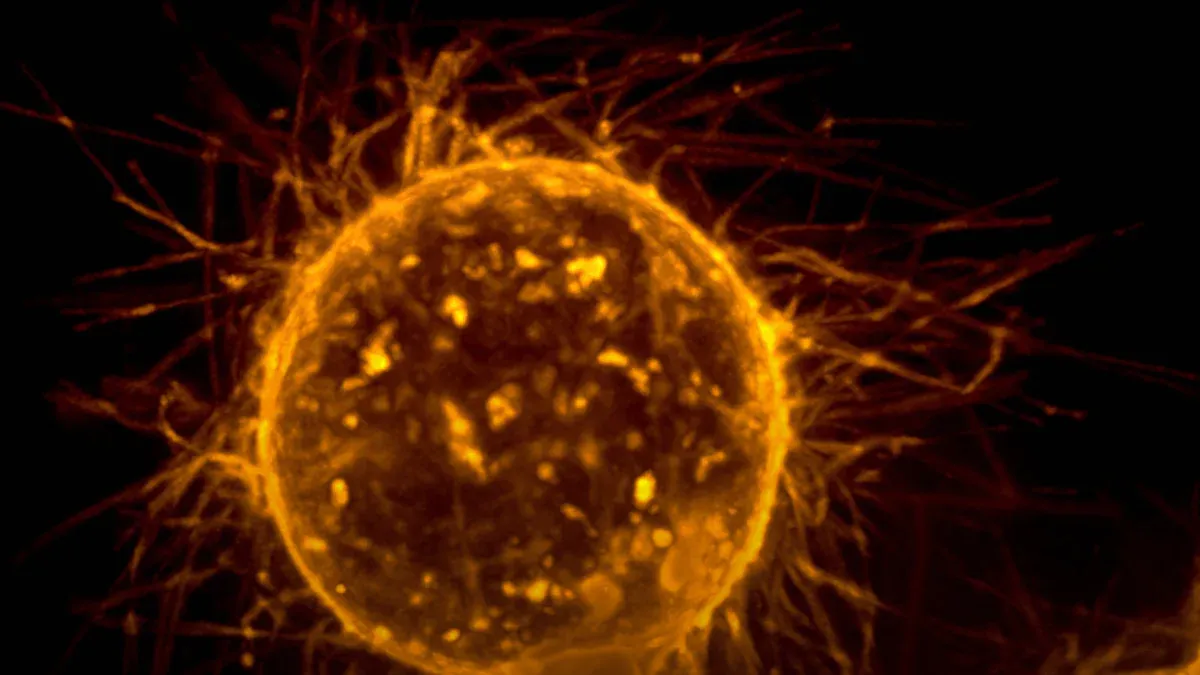
How surrounding cells and blood vessels support cancer growth.
The tumor microenvironment, which includes surrounding cells, blood vessels, and immune cells, significantly influences cancer growth. Cancer cells often manipulate nearby cells to create a supportive environment. For instance, they signal blood vessels to grow toward the tumor, ensuring a steady supply of nutrients and oxygen.
The impact of hypoxia (low oxygen) on tumor behavior.
Hypoxia, or low oxygen levels, can make tumors more aggressive. When oxygen is scarce, cancer cells adapt by activating genes that help them survive. This adaptation not only makes the tumor harder to treat but also increases its ability to spread. Understanding how hypoxia affects tumor behavior can help researchers develop more effective treatments.
Does cancer always spreads quickly? The answer depends on factors like cancer type, genetic mutations, and the tumor microenvironment. By understanding these influences, you can see why some cancers grow faster than others.
Immune System Involvement
How the immune system can suppress or enable metastasis
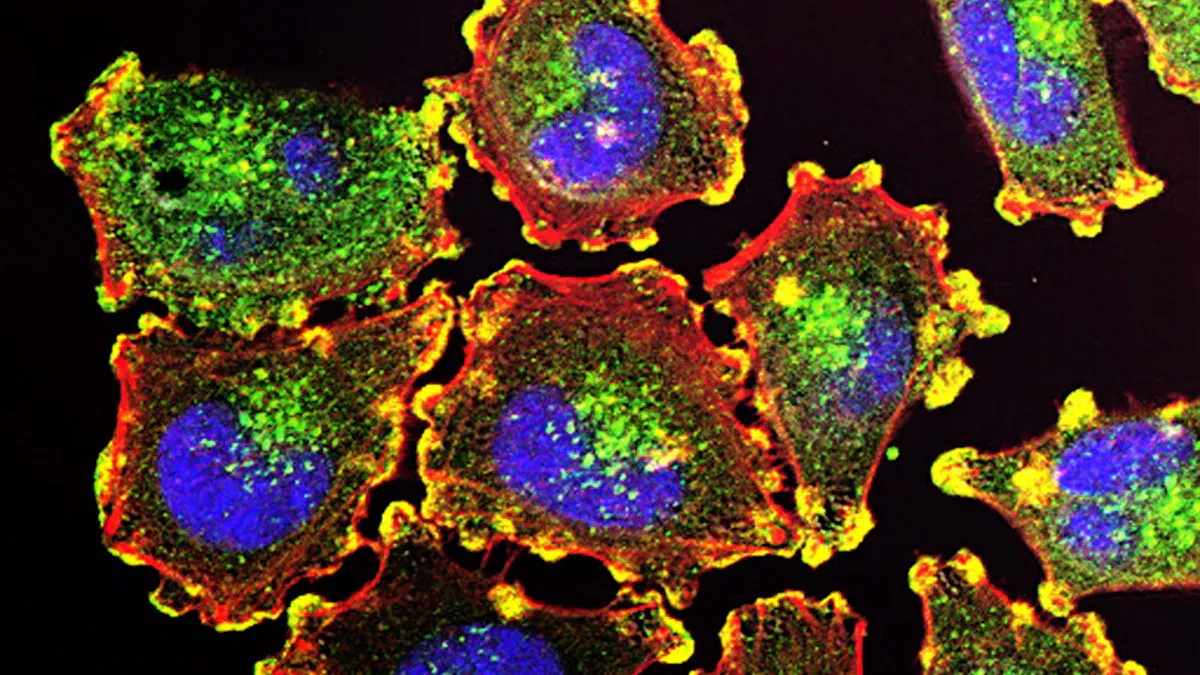
Your immune system plays a dual role in cancer spread. It can either fight cancer cells or unintentionally help them spread. Immune cells, such as T cells and natural killer (NK) cells, often attack cancer cells to prevent their growth. These cells patrol your body, identifying and destroying abnormal cells before they form tumors or metastasize. When your immune system functions effectively, it acts as a powerful defense against cancer.
However, cancer cells can manipulate your immune system to their advantage. They release signals that confuse immune cells, making them less effective. For example, some cancer cells produce proteins that suppress immune responses, allowing them to grow unchecked. This manipulation creates an environment where cancer cells can thrive and spread. Understanding how your immune system interacts with cancer cells can help researchers develop therapies that strengthen its ability to fight cancer.
The role of immune evasion in aggressive cancers
Aggressive cancers often use immune evasion to spread more effectively. These cancers trick your immune system into ignoring them, allowing them to move through your body undetected. They achieve this by altering how immune cells, like gamma delta T cells, respond. Instead of attacking cancer cells, these immune cells may receive signals that make them support cancer growth.
Cancer cells manipulate gamma delta T cells to aid their spread.
These immune cells can either attack or protect cancer cells, depending on the signals they receive.
Communication between cancer and immune cells helps cancer cells avoid detection as they travel through your body.
This ability to evade your immune system makes aggressive cancers harder to treat. Researchers are studying ways to block this communication, giving your immune system a better chance to fight back. By understanding immune evasion, scientists can create treatments that target these mechanisms and improve outcomes for patients with aggressive cancers.
Implications for Treatment and Research
Current Approaches to Slowing Cancer Spread
Targeting specific genetic mutations with precision medicine.
Precision medicine focuses on targeting specific genetic mutations that drive cancer growth. By identifying these mutations, doctors can use therapies designed to attack cancer cells while sparing healthy tissue. For example, in non-small cell lung cancer (NSCLC), mutations in the EGFR gene can be treated with drugs like erlotinib and gefitinib. Clinical trials such as IPASS and EURTAC have shown improved outcomes for patients with these therapies. Similarly, breast cancer patients with HER2-positive tumors benefit from trastuzumab, as demonstrated in trials like HERA and CLEOPATRA.
Cancer Type | Genetic Mutation | Targeted Therapy | Clinical Trials |
|---|---|---|---|
Non-small cell lung cancer | EGFR | IPASS (NCT00322452), EURTAC (NCT00446225), OPTIMAL (NCT00874419) | |
Breast cancer | HER2 | Trastuzumab | HERA (NCT00045032), CLEOPATRA (NCT00567190), NCCTG N9831 (NCT00004067; NCT00005970) |
Therapies aimed at disrupting the tumor microenvironment.
The tumor microenvironment plays a critical role in cancer spread. Therapies that disrupt this environment can slow metastasis. For instance, drugs targeting VEGF reduce blood vessel growth around tumors, cutting off their nutrient supply. Researchers are also exploring treatments that block signals between cancer cells and surrounding tissues, making it harder for tumors to grow and spread.
Emerging Research and Future Directions
Advances in immunotherapy to combat metastasis.
Immunotherapy is transforming cancer treatment by boosting your immune system's ability to fight cancer. Checkpoint inhibitors like pembrolizumab and nivolumab block proteins such as PD-1 and CTLA-4, helping immune cells attack cancer more effectively. CAR T-cell therapy, which engineers your T cells to target cancer, has shown success in blood cancers. Combining immunotherapies with traditional treatments has also improved outcomes. Experts predict significant advancements in antibody-drug conjugates (ADCs) by 2025, offering targeted delivery of toxic agents to cancer cells.
Checkpoint inhibitors enhance immune response against cancers like melanoma and lung cancer.
CAR T-cell therapy targets and kills cancer cells, especially in blood cancers.
ADCs are advancing, allowing precise delivery of treatments to cancer cells.
The potential of liquid biopsies for early detection of metastasis.
Liquid biopsies offer a non-invasive way to detect cancer spread early. These tests analyze blood samples for cancer-related markers, such as circulating tumor DNA. Early detection through liquid biopsies can help doctors monitor treatment effectiveness and adjust therapies as needed, improving patient outcomes.
Importance of Personalized Treatment
Tailoring therapies based on the unique biology of each cancer.
Personalized treatment tailors therapies to your cancer's specific genetic profile. Molecular profiling has revolutionized care by identifying mutations that guide treatment decisions. For example, NSCLC patients with EGFR mutations benefit from targeted therapies like erlotinib, while HER2-positive breast cancer patients respond well to trastuzumab. These approaches improve survival rates and reduce side effects.
The role of genetic testing in guiding treatment decisions.
Genetic testing plays a vital role in personalized cancer care. It helps doctors identify mutations driving your cancer, allowing them to choose the most effective treatments. Studies show that targeted therapies based on genetic testing improve outcomes across various cancer types. For instance, molecular profiling in metastatic cases has enhanced care by matching patients with therapies tailored to their specific needs.
Cancer Type | Treatment Approach | Outcome Description |
|---|---|---|
Non-small cell lung cancer | Targeted therapies (erlotinib, gefitinib) | Improved survival rates linked to specific genetic mutations in the EGFR gene. |
Various cancer types | Molecular profiling | Enhanced identification of mutations leading to targeted therapies and improved care. |
The speed at which cancer spreads depends on factors like its type, genetic mutations, and the tumor microenvironment. These elements shape how cancer grows and invades other parts of your body. By understanding these influences, you can see why some cancers are more aggressive than others.
Ongoing research continues to improve outcomes for metastatic cancer patients. Studies like the SABR-COMET trial show that metastases-directed therapy increases survival rates for patients with low metastatic burden. The STARS system also predicts a growing number of long-term survivors in certain patient groups.
Study Title | Findings |
|---|---|
Future trends in incidence and long-term survival of metastatic cancer | Certain subgroups of patients with metastatic cancer are living longer than in the past. |
Palma, D. A. et al. (2019) - SABR-COMET trial | Metastases directed therapy has improved survival outcomes in patients with low metastatic burden. |
Zaorsky, N. G. et al. (2021) - STARS system | STARS IVA and IVB patients groups projected to contain a greater proportion of long-term survivors. |
These advancements offer hope for better detection, prevention, and management of metastatic cancers, paving the way for improved treatments and brighter futures.
FAQ
What makes some cancers more aggressive than others?
Aggressive cancers often have genetic mutations that promote rapid growth and spread. These mutations help cancer cells invade tissues and evade your immune system. The tumor microenvironment, including blood vessels and surrounding cells, also plays a role in supporting aggressive behavior.
Can lifestyle choices affect how fast cancer spreads?
Lifestyle factors like smoking, poor diet, and lack of exercise can influence cancer progression. These habits may weaken your immune system or create conditions that help cancer grow. Maintaining a healthy lifestyle can reduce risks and improve treatment outcomes.
Why do some cancers respond better to treatment?
Cancers with specific genetic markers often respond well to targeted therapies. For example, HER2-positive breast cancer can be treated with trastuzumab. Early detection also improves treatment success, as localized cancers are easier to manage than metastatic ones.
How does early detection improve cancer outcomes?
Early detection helps doctors treat cancer before it spreads. Localized tumors are easier to remove or target with therapies. Screening tests like mammograms or colonoscopies can catch cancer early, increasing survival rates and improving your quality of life.
Are there new treatments for slowing cancer spread?
Yes, researchers are developing advanced therapies like immunotherapy and precision medicine. These treatments target specific cancer traits, such as genetic mutations or immune evasion mechanisms. Liquid biopsies and antibody-drug conjugates are also promising tools for managing metastatic cancers.
See Also
Exploring Cancer Types Associated With AIDS Infection
Key Characteristics of Glioblastoma You Need to Know
Understanding Lung Adenocarcinoma Causes and Associated Risks
Essential Information About Carcinoid Tumors You Should Know

