What Is Ductal Carcinoma In Situ and Its Symptoms
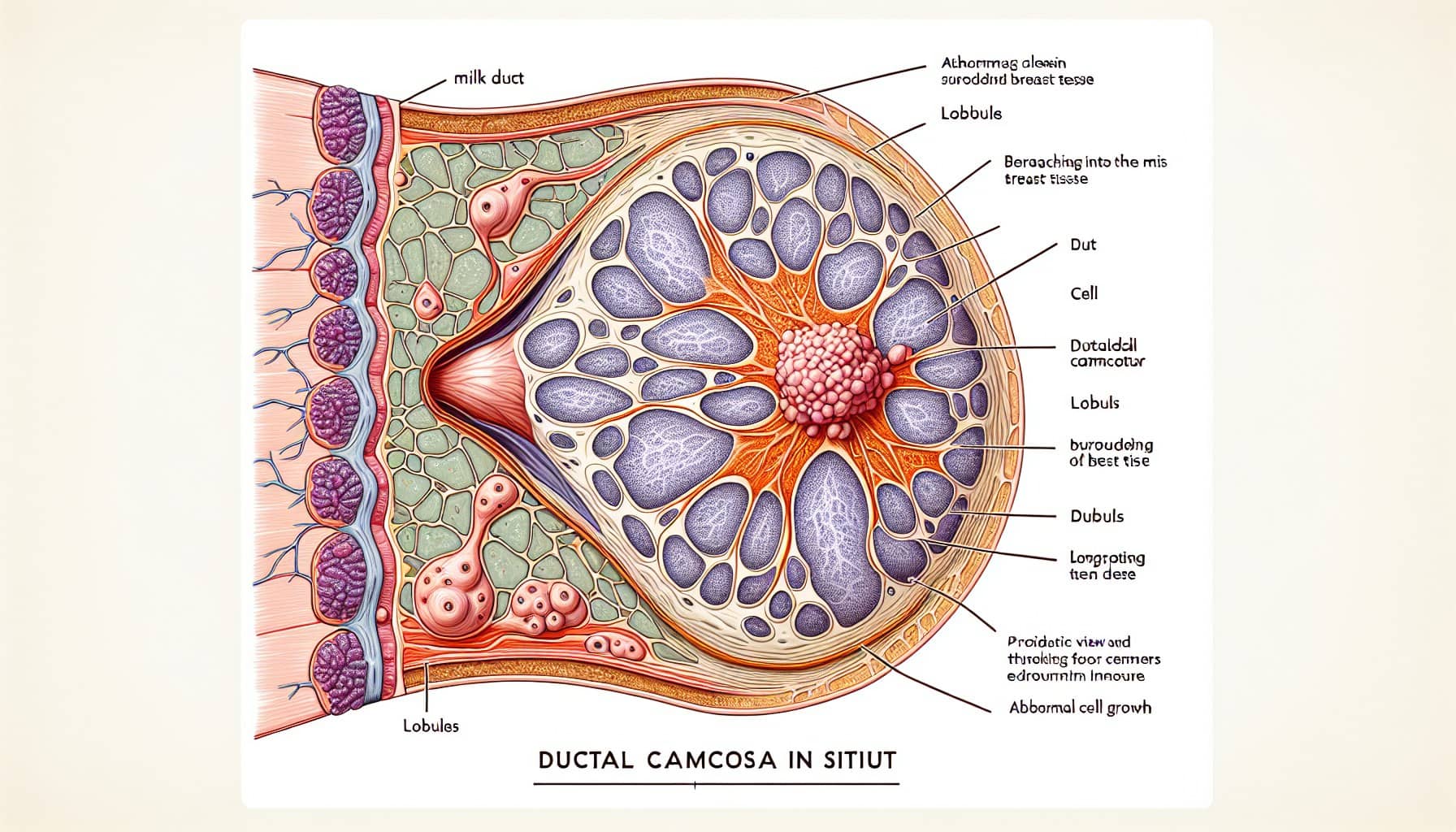
Ductal carcinoma in situ is a non-invasive breast cancer that stays within the milk ducts. It accounts for 20-25% of breast cancer diagnoses in the U.S. You may not notice symptoms, as DCIS is often silent. However, some individuals experience nipple discharge or feel a small lump. Routine mammograms play a vital role in identifying DCIS early. For women aged 40-49, 28.2% of screen-detected breast cancers are DCIS, while this percentage drops to 16.0% for those aged 70-84. Early detection improves outcomes and helps prevent progression to invasive cancer.
Key Takeaways
Ductal carcinoma in situ (DCIS) is a type of breast cancer. It does not spread and often has no symptoms. Getting regular mammograms is important to find it early.
Things that increase the risk of DCIS are age, family history, and habits. Living a healthy life can lower your chances of getting it.
If a mammogram shows DCIS, a biopsy is done to confirm it. Learning about biopsies can help you know what to expect.
Treatments for DCIS include removing the lump, removing the breast, or using radiation. Talk to your doctor to decide the best treatment for you.
After treatment, follow-up care is very important. Regular check-ups and tests can help find any problems early.
Causes and Risk Factors of Ductal Carcinoma In Situ
What Causes DCIS?
Ductal carcinoma in situ develops when abnormal cells grow within the milk ducts of your breast. These cells do not spread beyond the ducts, which makes DCIS a non-invasive condition. Researchers believe that genetic changes in breast cells trigger this abnormal growth. However, the exact cause remains unclear. Environmental factors and hormonal imbalances may also play a role in the development of DCIS.
Tip: Understanding the causes of DCIS can help you identify potential risks and take preventive measures.
Key Risk Factors
Age and Gender
Your risk of developing DCIS increases as you age. Women over 50 are more likely to be diagnosed with this condition. Although rare, men can also develop DCIS, but their risk is significantly lower.
Family History and Genetic Mutations
If someone in your family has had breast cancer, your chances of developing DCIS may increase. Genetic mutations, such as BRCA1 and BRCA2, also raise your risk. You might consider genetic testing if you have a strong family history of breast cancer.
Hormonal and Lifestyle Influences
Hormonal factors, like early menstruation or late menopause, can increase your risk of DCIS. Lifestyle choices, such as a high-fat diet, lack of exercise, or alcohol consumption, may also contribute. Maintaining a healthy lifestyle can help reduce your risk.
Note: While you cannot control some risk factors, like age or genetics, adopting healthier habits can make a difference.
Diagnosing Ductal Carcinoma In Situ
Mammograms as the Primary Diagnostic Tool
Mammograms play a crucial role in detecting ductal carcinoma in situ. These imaging tests use low-dose X-rays to examine your breast tissue for abnormalities. They are particularly effective at identifying microcalcifications, which are tiny calcium deposits that may indicate DCIS. Screening mammograms have a high sensitivity rate of 86.0% for detecting DCIS, making them a reliable tool for early diagnosis. However, their sensitivity for invasive breast cancer is slightly lower at 75.1%.
The effectiveness of mammograms varies with age. For women aged 40-49, 28.2% of screen-detected breast cancers are DCIS. This percentage decreases to 16.0% for women aged 70-84. Regular mammograms can help you catch DCIS early, even if you have no symptoms.
Confirming DCIS Through Biopsy
Types of Biopsies
If a mammogram reveals suspicious findings, your doctor may recommend a biopsy to confirm the diagnosis. Several types of biopsies are available, including core needle biopsy and vacuum-assisted biopsy. These procedures involve removing a small sample of breast tissue for further examination under a microscope.
What to Expect During the Procedure
During a biopsy, you will likely remain awake, but the area will be numbed with a local anesthetic. The doctor will use imaging guidance, such as ultrasound or mammography, to locate the area of concern. The procedure is usually quick and minimally invasive. Afterward, you may experience mild discomfort or bruising, but these symptoms typically resolve within a few days.
Additional Imaging Techniques
In some cases, additional imaging techniques may be necessary to evaluate suspicious findings further. Diagnostic mammograms provide higher magnification images from multiple angles, allowing for a closer look at microcalcifications or other abnormalities. If more information is needed, your doctor might recommend other imaging methods, such as breast MRI or ultrasound. These techniques can help clarify the nature of the abnormality and guide the next steps in your care.
Tip: If your doctor suggests additional imaging, it doesn’t always mean you have cancer. These tests help ensure an accurate diagnosis.
Recognizing Symptoms of Ductal Carcinoma In Situ
Common Symptoms
Nipple Discharge
One of the few noticeable symptoms of ductal carcinoma in situ is nipple discharge. This discharge may appear clear, bloody, or of another unusual color. While it is not always linked to DCIS, any unexpected nipple discharge should prompt you to consult a healthcare provider. Early evaluation can help determine the cause and guide appropriate care.
Breast Lump or Thickening
In rare cases, you might feel a lump or notice thickened tissue in your breast. These changes can sometimes indicate DCIS. However, most lumps are benign and unrelated to cancer. If you detect any unusual changes in your breast, it is essential to have them examined by a medical professional.
It is most commonly discovered through breast screening mammograms or ultrasound.
Occasionally, it can be found following a change in the breast, such as a lump or discharge from the nipple.
Why DCIS Is Often Symptom-Free
Ductal carcinoma in situ often develops silently. The abnormal cells remain confined to the milk ducts and do not invade surrounding tissues. This lack of spread means you may not experience pain, swelling, or other noticeable symptoms. For this reason, many cases of DCIS are only identified during routine breast screenings.
The Role of Regular Screening in Detection
Routine mammograms play a critical role in detecting ductal carcinoma in situ early. These screenings can identify microcalcifications or other abnormalities that may not cause symptoms. By scheduling regular mammograms, you increase your chances of catching DCIS before it progresses to invasive cancer. Early detection allows for more treatment options and better outcomes.
Tip: If you are over 40 or have risk factors for breast cancer, talk to your doctor about the right screening schedule for you.
Treatment Options for Ductal Carcinoma In Situ
Surgical Treatments
Lumpectomy
A lumpectomy involves removing the abnormal cells and a small margin of surrounding healthy tissue. This procedure allows you to preserve most of your breast. It is often paired with radiation therapy to reduce the risk of recurrence. Studies show that lumpectomy combined with radiation offers a 10-year overall survival (OS) rate of 89.6%. The disease-specific survival (DSS) rate for this combination is 98.9%. If you opt for a lumpectomy alone, the OS rate drops to 80.6%, though the DSS rate remains high at 98.4%. These statistics highlight the effectiveness of lumpectomy, especially when paired with radiation.
Mastectomy
A mastectomy involves removing the entire breast. This option may be recommended if you have widespread ductal carcinoma in situ or if you prefer a more definitive approach. The 10-year OS rate for mastectomy is 86.1%, while the DSS rate is 98.5%. Despite the differences in survival rates, the prognosis for DCIS remains excellent regardless of the treatment type. Many women achieve long-term survival and low recurrence rates after a mastectomy.
Note: Both lumpectomy and mastectomy have favorable outcomes. Your doctor can help you decide which option aligns best with your needs and preferences.
Radiation Therapy
Radiation therapy is often used after a lumpectomy to target any remaining abnormal cells. This treatment significantly lowers the risk of recurrence. It involves directing high-energy rays at the affected area to destroy cancerous cells. Radiation therapy is a non-invasive option that complements surgical treatments, enhancing their effectiveness. If you choose this approach, your healthcare team will guide you through the process and address any concerns.
Hormone Therapy
Hormone therapy is recommended for hormone receptor-positive ductal carcinoma in situ. Medications like tamoxifen help reduce the risk of recurrence by blocking estrogen, which fuels the growth of some cancer cells. If you experience side effects from standard tamoxifen, low-dose tamoxifen may be an alternative. Women who undergo a lumpectomy for hormone receptor-positive DCIS often benefit from taking tamoxifen for three years. This therapy provides an additional layer of protection against recurrence.
Tip: If your DCIS is hormone receptor-positive, ask your doctor about the benefits of hormone therapy and whether it is right for you.
Importance of Follow-Up Care
Follow-up care plays a vital role in managing your health after treatment for ductal carcinoma in situ (DCIS). It helps monitor for recurrence and ensures that any new changes in your breast tissue are detected early. By staying proactive, you can maintain peace of mind and take control of your long-term health.
Your follow-up care plan should include regular screenings and check-ups. These appointments allow your doctor to assess your recovery and identify any signs of recurrence. The frequency of these visits depends on your individual case, so it’s important to discuss a personalized schedule with your healthcare provider.
Continued mammograms or other screening tests are essential components of follow-up care. Mammograms help detect any abnormalities in your breast tissue, even if you feel fine. Your doctor may recommend annual mammograms or more frequent screenings based on your risk factors and treatment history.
Tip: Keep a record of your follow-up appointments and test results. This helps you stay organized and ensures you don’t miss any critical steps in your care.
In addition to screenings, you should remain vigilant about any changes in your breasts. Report symptoms like new lumps, nipple discharge, or skin changes to your doctor immediately. Early reporting can lead to prompt evaluation and treatment if needed.
By committing to follow-up care, you improve your chances of maintaining good health and reducing the risk of recurrence. Regular monitoring empowers you to address potential issues early, giving you the best possible outcome after DCIS treatment.
Prognosis and Recurrence Risks of Ductal Carcinoma In Situ
Long-Term Prognosis for DCIS
The long-term outlook for ductal carcinoma in situ is highly favorable. Most patients achieve excellent outcomes with timely treatment. The 10-year survival rate for DCIS is approximately 98%, reflecting the effectiveness of current therapies. Over a 20-year period, the overall death rate from breast cancer after a DCIS diagnosis is just 3.3%. This rate is comparable to that of the general population, highlighting the low likelihood of life-threatening progression when DCIS is managed appropriately.
Tip: Early detection and treatment significantly improve your chances of maintaining good health after a DCIS diagnosis.
Risks of Recurrence After Treatment
While the prognosis is excellent, DCIS can recur in some cases. Several factors influence the risk of recurrence. The type of treatment you receive plays a major role. For example, lumpectomy without radiation therapy increases the likelihood of recurrence compared to lumpectomy with radiation or mastectomy. Younger age at diagnosis, larger tumor size, and positive surgical margins also elevate the risk. High-grade tumors, such as the comedo subtype, are more likely to return than lower-grade forms.
Other factors include:
Tumor size (≥ 1.5 cm)
Premenopausal status, which doubles the risk
Higher body mass index, linked to a twofold increase in recurrence
By working closely with your healthcare team, you can choose a treatment plan that minimizes these risks.
Consequences of Leaving DCIS Untreated
If left untreated, ductal carcinoma in situ may progress to invasive breast cancer. Unlike DCIS, invasive cancer spreads beyond the milk ducts and poses a greater threat to your health. The progression rate varies, but untreated DCIS increases the likelihood of developing a more aggressive form of cancer. Additionally, the psychological toll of living with untreated DCIS can be significant. Many individuals experience anxiety, depression, and emotional distress due to the uncertainty surrounding the condition.
Note: Seeking timely treatment not only reduces the risk of progression but also provides peace of mind.
Understanding ductal carcinoma in situ empowers you to take control of your breast health. Recognizing its symptoms and risk factors can help you stay vigilant. Early detection through routine mammograms plays a vital role in identifying this condition before it progresses. By catching it early, you increase your chances of successful treatment and long-term health. Always consult your doctor for personalized care and screening recommendations. Taking proactive steps today can make a significant difference in your future well-being.
FAQ
What is the difference between DCIS and invasive breast cancer?
DCIS stays within the milk ducts and does not spread to surrounding tissues. Invasive breast cancer grows beyond the ducts and can spread to other parts of your body. Early detection of DCIS helps prevent progression to invasive cancer.
Can men develop ductal carcinoma in situ?
Yes, men can develop DCIS, but it is rare. Male breast cancer accounts for less than 1% of all breast cancer cases. If you notice unusual changes in your chest area, consult a doctor for evaluation.
How often should you get a mammogram?
Women aged 40 and older should discuss mammogram frequency with their doctor. Most guidelines recommend annual or biennial screenings. If you have risk factors, your doctor may suggest starting earlier or screening more frequently.
Tip: Regular mammograms improve early detection and treatment outcomes.
Is DCIS life-threatening?
DCIS is not life-threatening when treated promptly. It is a non-invasive condition with a high survival rate. However, untreated DCIS can progress to invasive cancer, which poses greater health risks.
Can lifestyle changes reduce your risk of DCIS?
Yes, adopting a healthy lifestyle can lower your risk. Maintain a balanced diet, exercise regularly, and limit alcohol consumption. These habits support overall breast health and may reduce the likelihood of developing DCIS.
Note: While lifestyle changes help, regular screenings remain essential for early detection.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Carcinoid Syndrome: Key Symptoms To Recognize
Identifying Basal Cell Carcinoma: Symptoms You Should Know
Breast Cancer: Common Symptoms and Underlying Causes Explained
Burkitt's Lymphoma: Symptoms and Important Information To Know
Essential Insights About Carcinoid Tumors You Must Understand

