Unraveling the Rise of Early-Onset Cancers in Younger Adults
A 32-year-old woman, once focused on her career and family, now faces an unexpected diagnosis: colorectal cancer. Her story highlights a troubling shift in early-onset cancer trends. In the United States, cases among adults under 50 have risen sharply, with breast and colorectal cancers leading the surge. Globally, early-onset cancer incidence jumped by 79% between 1990 and 2019. Experts remain puzzled by the causes, pointing to possible links with lifestyle, environment, and early-life exposures. These changes challenge communities to re-examine health priorities and support those affected.
Key Takeaways
Early-onset cancers, diagnosed in adults under 50, are rising worldwide, especially breast and colorectal cancers.
Lifestyle factors like obesity, poor diet, and inactivity strongly increase cancer risk and offer chances for prevention.
Environmental exposures such as pollution and chemicals also contribute to early cancer development.
Genetic mutations play a key role, so genetic testing helps identify high-risk individuals and guide treatment.
Delays in diagnosis happen because symptoms are often missed or mistaken, so awareness and early checkups are vital.
Early-Onset Cancer Trends

Demographics
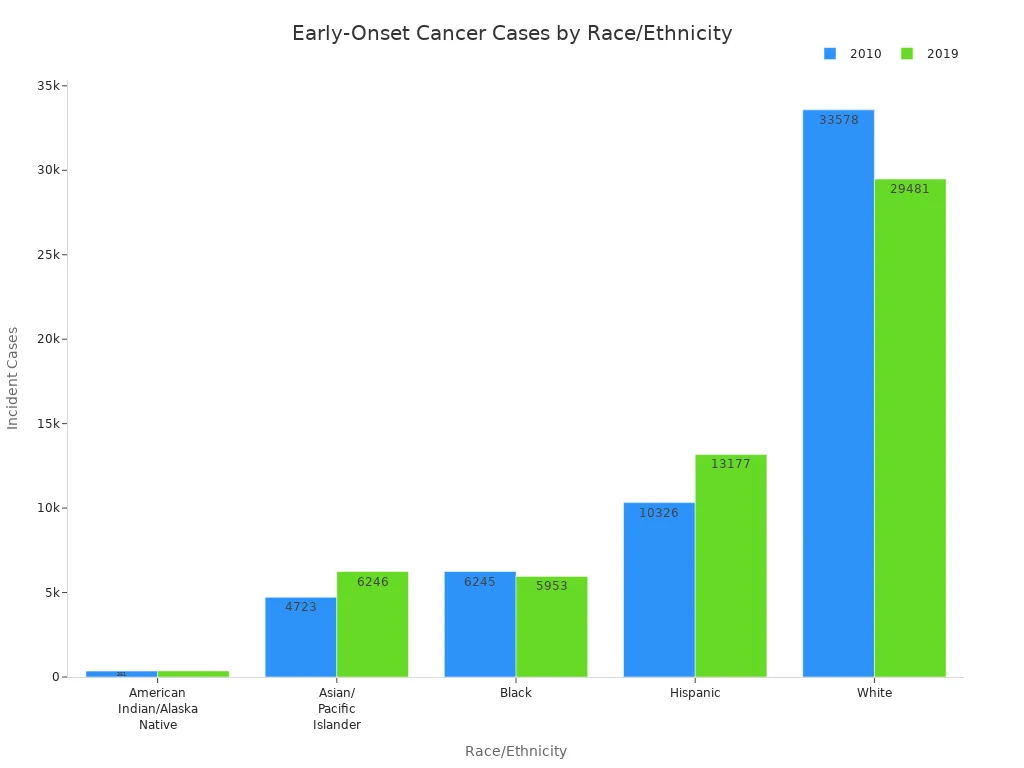
Early-onset cancer trends show a clear shift in who gets diagnosed. Females account for about 63% of cases, with breast, thyroid, and melanoma being the most common cancers. Males see higher rates of melanoma, colorectal, and testicular cancers. The largest increases in diagnoses from 2010 to 2019 occurred in female breast, colorectal, kidney, uterine, and pancreatic cancers. These five types made up over 80% of new cases in younger adults. The rise in early-onset cancer trends is not equal across all groups. Hispanic and Asian/Pacific Islander populations saw the largest increases, while rates among Black and White populations remained stable or declined. Genetics play a role, but rapid changes in early-onset cancer trends suggest that lifestyle and environment have a bigger impact.
Aspect | Data/Trend |
|---|---|
Overall early-onset cancer incidence in US (2010-2019) | Increased slightly from 99.96 to 102.97 cases per 100,000 (APC 0.28%, p=0.01) |
Incidence trend by sex | Females: increased (APC 0.67%, p=0.001); Males: decreased (APC -0.37%, p<0.001) |
Incidence trend by race/ethnicity | American Indian/Alaska Native: +1.97% APC; Asian/Pacific Islander: +0.97% APC; Hispanic: +1.43% APC; White: stable (0.04% APC); Black: decreased (-0.47% APC) |
Incidence trend by age group | 30-39 years: increased (APC 0.91%, p=0.002); other under-50 age groups stable |
Most common early-onset cancer (2019) | Breast cancer |
Fastest growing early-onset cancer types | Gastrointestinal cancers (colon/rectum, stomach, pancreas) |
Colorectal Cancer
Colorectal cancer stands out in early-onset cancer trends. It now makes up about 10% of all new colorectal cancer diagnoses. The incidence in adults under 50 rises by about 1.4% each year, while rates in older adults fall. The increase is most pronounced among non-Hispanic whites and younger age groups, especially those aged 15 to 29. Males experience faster increases than females. Most new cases appear in the left side of the colon or rectum and often at more advanced stages. Obesity in young adults is a likely factor. Screening guidelines now recommend starting at age 45 instead of 50 to catch more cases early.
Other Cancers
Early-onset cancer trends also include rising rates of other types. Breast cancer remains the most common, but kidney, uterine, pancreatic, and several digestive system cancers show significant increases. Researchers note a "birth cohort effect," where each new generation faces higher risks before age 50. Factors such as diet, alcohol use, processed foods, and sedentary lifestyles contribute to these trends. The table below highlights cancer types with increased incidence in adults under 50:
Cancer Types with Increased Incidence in Adults Under 50 | Notes |
|---|---|
Breast cancer (females) | Increased incidence observed |
Colorectal cancer | Increased incidence and deaths in younger groups |
Kidney cancer | Increased incidence observed |
Testicular cancer | Increased incidence and deaths in younger groups |
Uterine cancer | Increased incidence and deaths in younger groups |
Pancreatic cancer | Increased incidence observed |
Blood cancers (lymphomas - 3 types) | Increased incidence observed |
Melanoma | Increased incidence only in younger groups |
Cervical cancer | Increased incidence only in younger groups |
Stomach cancer | Increased incidence only in younger groups |
Cancer of bones and joints | Increased incidence only in younger groups |
Plasma cell neoplasms | Increased incidence only in younger groups |
Note: While some cancer types are rising, others like lung and prostate cancer are declining in younger adults. Early-onset cancer trends highlight the need for ongoing research and updated prevention strategies.
Causes
Lifestyle Factors
Researchers have identified several lifestyle factors that increase the risk of early-onset cancers. Many of these factors are modifiable, meaning people can change them to lower their risk. Studies show that certain habits and behaviors play a key role, especially for cancers like breast and colorectal cancer.
Overweight status in women aged 40-49 increases the chance of developing early-onset breast cancer.
Smoking in women within this age group links to a higher risk of breast cancer.
Even moderate physical activity, when combined with other risk factors, can raise breast cancer risk in some women.
Hormonal factors, such as early age at first period (menarche) and late menopause, are associated with increased breast cancer risk.
Use of hormonal contraceptives slightly raises the risk of breast cancer.
Reproductive choices, including the number of children and age at first childbirth, influence breast cancer risk in complex ways.
For early-onset colorectal cancer, unhealthy lifestyle patterns also play a major role:
Physical inactivity and long periods of sitting, such as watching TV for 14 or more hours per week, increase the risk of colorectal cancer in younger adults.
Obesity, defined as a body mass index (BMI) of 25 or higher, is strongly linked to early-onset colorectal cancer. The risk rises as BMI increases.
Diets high in processed meats, sugary drinks, and alcohol, as well as Western dietary patterns, contribute to higher cancer risk.
Large studies confirm that overweight and obesity increase the risk of early-onset colorectal cancer by up to 42%.
Modifiable lifestyle factors—diet, exercise, and weight management—offer important opportunities for prevention. Researchers continue to study how these factors interact and how changes in habits can lower cancer risk in younger adults.
Environment
Environmental exposures also contribute to the rise in early-onset cancers. These exposures include both physical surroundings and substances people encounter in daily life. Some of the most important environmental risk factors are excess body weight, pollution, and chemicals.
Environmental Exposure | Association with Early-Onset Cancer | Key Findings |
|---|---|---|
Excess Body Weight (BMI ≥25) | Strongest risk factor for colorectal cancer | Responsible for about 30% of the increase in early-onset colorectal cancer from 1992 to 2016 |
Obesity (BMI ≥30) | Significant risk factor across groups | Similar increased risk for men and women of different races |
Alcohol Consumption | Risk factor for several cancers | Linked to higher rates of early-onset colorectal cancer |
Associated with breast, prostate, and melanoma | Higher cancer rates in adults aged 25–49 years | |
Water Pollution (toxic metals, pesticides) | Linked to various cancers | Increases risk through contaminated drinking water |
Many common carcinogens found in the environment can damage DNA and lead to cancer. These include:
Arsenic (found in contaminated water and some workplaces)
Asbestos (used in construction materials)
Benzene (used in the petroleum industry and some manufacturing)
Cadmium and nickel (used in batteries and coatings)
Radon (a gas found in some homes and mines)
Formaldehyde (used in hospitals and labs)
Hair dyes (exposure for hairdressers and barbers)
Smoke from cigarettes and air pollution
Environmental carcinogens can cause genetic mutations in important genes that control cell growth and repair. These mutations may lead to cancer, especially in people who already have a genetic predisposition. Pollution and chemical exposures can also speed up biological aging, which may explain why some cancers appear earlier in life.
Genetics
Genetic factors play a significant role in early-onset cancers, especially when cancer appears in several family members at young ages. Inherited mutations in certain genes increase the risk of developing cancer before age 50.
BRCA1 and BRCA2 mutations are common in women with breast cancer under age 40. These mutations also increase the risk of ovarian and prostate cancers.
CHEK2 mutations, especially 1100delC and c.470T>C, raise the risk of breast, colon, prostate, kidney, and thyroid cancers. Younger patients have higher rates of these mutations.
Other important genes include ATM, PALB2, CDKN2A, HOXB13, PPM1D, and RECQL. Many of these genes help repair DNA or control cell growth.
About 21% of early-onset cancer patients carry inherited mutations, compared to a lower percentage in older adults.
Germline TP53 mutations, seen in Li-Fraumeni syndrome, are more common in young-adult cancers.
Aspect | Early-Onset Cancer Cases | Late-Onset Cancer Cases |
|---|---|---|
Stronger; highest familial risk when parents diagnosed young | Present but less pronounced | |
Familial Risk | High, especially with early-onset family history | Moderate |
Genetic vs Environmental Influence | Largely genetic | More environmental |
Clinical Implication | Important for counseling and prevention | Less impact on early detection |
Genetic testing helps identify people at higher risk and guides decisions about screening and prevention. While genetics explain many early-onset cancers, most cases still involve a mix of genetic and environmental factors. Families with a history of early-onset cancer should discuss genetic counseling with their healthcare provider.
Biology
Tumor Behavior
Tumors in early-onset cancers often act differently than those in older adults.
Many early-onset colon cancers show more aggressive growth.
Doctors often find these cancers at advanced stages because symptoms may go unnoticed or misattributed.
Despite this, younger adults usually have better survival rates than older adults when doctors compare cancers at the same stage.
Younger patients can handle strong treatments, such as surgery and chemotherapy, more effectively.
Unique genetic profiles in younger patients may affect how tumors grow and respond to treatment, but researchers continue to study these differences.
Genetic Mutations
Gene mutations play a key role in early-onset cancers. Mutations in oncogenes can cause cells to grow out of control. When tumor suppressor genes lose their function, the body loses important checks on cell growth. Mutations in DNA repair genes allow more genetic errors to build up. These changes can lead to cancer at a younger age and may make tumors more aggressive or harder to treat. Doctors use this knowledge to understand why some families see cancer appear earlier and more often.
Genetic Mutation | Associated Syndrome | Impact on Prognosis |
|---|---|---|
PTEN | Cowden Syndrome | Higher risk of many tumors, often at a young age |
MLH1, MSH2, MSH6, PMS2, EPCAM | Lynch Syndrome | High risk of colorectal and other cancers, earlier onset |
APC | Familial Adenomatous Polyposis (FAP) | Many colon polyps, high colon cancer risk, early onset |
TP53 | Li-Fraumeni Syndrome | Multiple cancers, early onset, more aggressive |
VHL | Von Hippel-Lindau Disease | Tumors in kidneys and brain, early onset |
Lynch Syndrome
Lynch Syndrome stands out as a common inherited cause of early-onset colorectal cancer. Studies show that 5% to 20% of young adults with colorectal cancer have Lynch Syndrome, with higher rates in those with a family history. Doctors use tests like immunohistochemistry and microsatellite instability analysis to find Lynch Syndrome. Family history and tumor location help guide who should get these tests. Universal screening of all colorectal tumors for mismatch repair problems helps catch more cases. People with Lynch Syndrome need early and regular colonoscopies, starting as young as 20 to 25 years old, and other screenings to lower cancer risk and improve survival.
Diagnosis Challenges
Awareness
Many healthcare providers and patients do not expect cancer in younger adults. This low awareness leads to missed early signs and delays in diagnosis. Doctors often focus on more common illnesses in young people and may not consider cancer as a possible cause. This age-related bias means that cancer is rarely included in the first list of possible diagnoses.
General practitioners often have a low suspicion of cancer in patients under 50.
Cancer is not usually considered when younger adults present with symptoms, even if those symptoms are serious.
Many younger patients do not recognize cancer warning signs or do not think they are at risk.
Public health campaigns about cancer symptoms rarely target younger adults.
Healthcare providers sometimes misattribute symptoms in women to gynecological issues instead of considering cancers like colorectal cancer.
The absence of traditional risk factors, such as family history, can lead doctors to dismiss the possibility of cancer.
There is a lack of age-appropriate diagnostic pathways and support services for younger patients.
Training and awareness programs for healthcare providers can help reduce these biases.
Decision support tools and updated clinical guidelines can prompt doctors to consider cancer in younger adults.
Raising awareness among both patients and clinicians is essential. Early recognition of symptoms and a willingness to consider cancer in younger adults can improve outcomes.
Symptoms
Early-onset cancers often present with symptoms that are vague or similar to common, less serious conditions. This overlap makes it easy for both patients and doctors to misinterpret the warning signs.
Common symptoms include persistent fatigue, unexplained weight loss, night sweats, mild anemia, and low-grade fever.
Organ-specific symptoms often mimic benign conditions:
Persistent cough or hoarseness may look like a simple infection.
Changes in bowel habits are often blamed on diet, stress, or irritable bowel syndrome.
Breast lumps or skin changes may be dismissed as cysts or normal variations.
Ovarian cancer symptoms, such as bloating and pelvic discomfort, can resemble urinary or digestive problems.
Hematologic cancers may cause fatigue, fever, and swollen lymph nodes, which are often mistaken for infections.
Many symptoms last for weeks or months before patients seek help.
Doctors may attribute symptoms to lifestyle factors or stress, especially in younger adults.
The rarity of cancer in this age group leads to frequent misdiagnosis.
Symptom Type | Common Misattribution | Cancer Type(s) |
|---|---|---|
Fatigue, weight loss | Stress, overwork, infection | Many |
Bowel changes | IBS, hemorrhoids, diet | Colorectal |
Breast lumps | Cysts, fibrocystic changes | Breast |
Bone pain/swelling | Sports injury, benign tumor | Sarcoma |
Night sweats, fever | Viral infection, autoimmune disease | Lymphoma, leukemia |
Skin changes | Benign moles, eczema | Melanoma |
Pelvic pain/bloating | GI or urinary infection | Ovarian |
Persistent, unexplained symptoms lasting more than four to six weeks should prompt further evaluation, even in younger adults.
Delays
Diagnostic delays remain a major challenge for early-onset cancers. These delays can occur at several stages, from the time symptoms first appear to the moment a diagnosis is made.
The average delay in diagnosis for early-onset cancer patients is about five months.
Nearly half of patients experience delays of three months or more.
Delays often result from:
Socioeconomic deprivation, with lower-income patients facing more barriers.
Lack of symptom recognition, leading patients to ignore or minimize warning signs.
Embarrassment, fear, or being too busy to seek medical advice.
Worry about wasting the doctor's time.
Practitioner-related issues, such as misdiagnosis or inadequate examination.
Poor continuity of care and slow referrals between primary and specialist care.
Patients from impoverished or less-educated backgrounds are more likely to experience delays.
Delays often lead to diagnosis at more advanced cancer stages, which lowers survival rates.
Clinical audit data show that 22% of cancer cases involve significant diagnostic delays due to patient, clinician, or system factors.
Diagnostic delay in cancer occurs in three phases: patient delay (waiting to see a doctor), practitioner delay (doctor not recognizing or investigating symptoms), and system delay (slow referrals or test results). Addressing each phase can help reduce delays and improve outcomes for younger adults.
Treatment and Support
Immunotherapy
Immunotherapy has changed how doctors treat many early-onset cancers. This treatment uses the body’s own immune system to find and attack cancer cells. Doctors use immunotherapy for cancers like melanoma, lymphoma, and some types of colorectal cancer. Drugs called immune checkpoint inhibitors help the immune system work better against cancer. Younger adults often respond well to these treatments because their immune systems are strong. Immunotherapy can cause side effects, such as fatigue or skin problems, but doctors monitor patients closely. New research explores how to combine immunotherapy with other treatments to improve results for younger patients.
Genetic Testing
Genetic testing plays a key role in guiding treatment for early-onset cancers. Doctors test for changes in genes like BRCA1, BRCA2, CHEK2, and ATM, especially in young women with breast cancer. These tests help doctors choose the best treatment, such as targeted therapies like PARP inhibitors for cancers with BRCA mutations. Genetic testing also finds circulating tumor DNA in blood, which helps with diagnosis and staging. In a recent study, doctors offered genetic testing to women diagnosed with breast cancer at age 35 or younger. They found that 10–15% carried important gene changes. This information helped guide treatment and future cancer screening. Patients who learned about their genetic risks received counseling and support, making it easier to manage their care.
Patient Resources
Younger adults with cancer face unique challenges. Many turn to social media and online groups for support and information. These platforms offer peer mentorship, where patients share advice and emotional support. This peer-to-peer help reduces anxiety and gives practical tips for managing treatment and side effects. Specialized care programs assign each patient a coordinator who connects them to doctors, social workers, and psychologists. This team approach ensures patients get the right care during and after treatment. Resources for young adults include education, advocacy, fertility preservation, financial help, and telehealth services. Nonprofit groups and patient advisory boards also help improve care and support for this age group.
Research and Action

Knowledge Gaps
Researchers continue to face many unanswered questions about early-onset cancers. While some cases link to inherited gene changes, most appear without a clear cause. Scientists do not fully understand how diet, lifestyle, environment, and the microbiome from early life through adulthood contribute to cancer risk. The exact role of early-life exposures, including those before birth, remains unclear. Experts call for new research that brings together epidemiology, molecular biology, nutrition, and environmental science. They also see a need for advanced tools, such as multi-omics technologies, to study how genes and environment interact over time. These gaps make it difficult to create strong prevention and treatment strategies. The complexity of early-onset cancers means that doctors and scientists must work together across many fields to find answers.
The rising number of early-onset cancers, especially in the digestive system, highlights the urgent need for better research and new approaches to prevention and care.
Awareness Efforts
Several organizations have launched campaigns to raise awareness about cancer risk and prevention. These efforts aim to educate both the public and healthcare professionals, though few focus only on early-onset cancers. Some key campaigns include:
The American Association for Cancer Research promotes National Cancer Prevention Month and World Cancer Day, encouraging healthy habits to lower cancer risk.
The GW Cancer Center offers health awareness campaigns and training for healthcare workers to improve communication and provide culturally sensitive care.
FORCE (Facing Our Risk of Cancer Empowered) supports individuals and families facing hereditary cancer through education and advocacy.
The Foundation for Women’s Cancer provides information on gynecologic cancer risk, prevention, and early detection.
The Gay and Lesbian Medical Association works to ensure health equity for LGBTQ+ populations, offering resources for both patients and providers.
While these campaigns help spread important messages, most do not target early-onset cancers directly. More focused efforts could help younger adults and their doctors recognize cancer risks and symptoms sooner.
Rising early-onset cancer trends present urgent and complex challenges.
Rates have increased across many countries and cancer types, especially among younger adults.
Multiple factors, such as obesity, environmental exposures, and changing lifestyles, interact to drive these trends.
Delayed diagnosis and unique tumor biology add to the burden.
Stakeholders can improve early detection and support by engaging communities, strengthening partnerships, and co-designing solutions that fit local needs. Ongoing research and collaboration remain essential for better outcomes.
FAQ
What is early-onset cancer?
Early-onset cancer refers to cancer diagnosed in adults under age 50. These cancers often show different patterns and risks compared to those found in older adults.
Why are cancer rates rising in younger adults?
Researchers see increases due to changes in lifestyle, environment, and genetics. Obesity, poor diet, and pollution play major roles. Scientists continue to study other possible causes.
What symptoms should younger adults watch for?
Younger adults should watch for unexplained weight loss, fatigue, changes in bowel habits, or lumps. Persistent symptoms lasting more than four weeks need medical attention.
Can early-onset cancers be prevented?
Some risk factors, like genetics, cannot be changed. However, healthy eating, regular exercise, and avoiding tobacco and excess alcohol can lower risk. Regular checkups help with early detection.
Should younger adults get screened for cancer?
Doctors recommend screening based on personal and family history. For example, colorectal cancer screening now starts at age 45. People with strong family histories may need earlier or more frequent tests.
See Also
Essential Information About Embryonal Carcinoma You Should Know
Different Cancer Types Commonly Associated With AIDS Patients
An In-Depth Overview Covering Every Recognized Cancer Type
A Clear Explanation Of Islet Cell Carcinoma In Pancreas
Key Characteristics And Insights Into Glioblastoma Brain Tumors

