Embryonal Carcinoma Explained: Key Facts You Need
Embryonal carcinoma is a rare type of germ cell tumor that grows aggressively. It often spreads quickly to other parts of your body, making early detection crucial. This tumor can appear as part of mixed germ cell tumors in 84% of cases, while pure forms account for only 16%. Its rapid progression poses serious health risks, but timely diagnosis and treatment can significantly improve outcomes. Understanding its nature helps you recognize symptoms early and seek medical care promptly.
Key Takeaways
Embryonal carcinoma is a rare but fast-growing tumor. It can spread quickly, so finding it early helps treatment.
Common signs are a painless lump in the testis or ovary, swelling, and feeling very tired. Spotting these signs early means faster care.
Doctors use physical exams, imaging tests, and blood tests to find tumor markers. A biopsy confirms if cancer cells are present.
Treatment usually starts with surgery to remove the tumor. Chemotherapy is used next to destroy leftover cancer cells. Using both treatments works better.
After treatment, regular check-ups are important to watch for cancer returning. Staying alert helps keep you healthy long-term.
What Is Embryonal Carcinoma?
Definition and Overview
Embryonal carcinoma is a type of nonseminoma germ cell tumor. It develops in the reproductive organs, such as the testes or ovaries. This tumor is relatively rare but highly aggressive. In the testis, pure embryonal carcinoma accounts for about 10% of testicular germ cell tumors. However, it appears in nearly 90% of mixed nonseminomatous germ cell tumors. Its rapid growth and potential to spread make early detection critical for effective treatment.
Common Locations in the Body
Embryonal carcinoma typically develops in specific areas of the body. The table below highlights its most common anatomical locations:
Anatomical Location | Prevalence |
|---|---|
Testis | 84% (as part of mixed germ cell tumors) |
Testis | 16% (pure embryonal carcinoma) |
Ovary | ~3% (of ovarian germ cell tumors) |
Understanding these locations can help you recognize symptoms early and seek medical care.
How It Differs From Other Germ Cell Tumors
Embryonal carcinoma stands out from other germ cell tumors due to its unique histological and clinical features. It exhibits three distinct patterns: solid, tubular (glandlike), and papillary. These patterns, along with specific cytological characteristics, differentiate it from seminomas. Clinically, embryonal carcinoma is more aggressive, often spreading to the retroperitoneum, lungs, or liver. It typically affects individuals around age 30, with 10-40% of cases presenting with metastasis at diagnosis.
By understanding these differences, you can better grasp the seriousness of embryonal carcinoma and the importance of early intervention.
Characteristics of Embryonal Carcinoma
Aggressive Growth and Spread
Embryonal carcinoma grows rapidly and spreads to other parts of your body. This tumor often invades nearby tissues and metastasizes to distant organs, such as the lungs, liver, and retroperitoneum. Its aggressive nature makes early detection essential. You may notice symptoms like swelling or pain in the affected area, but these signs often appear after the tumor has already advanced. Unlike some other germ cell tumors, embryonal carcinoma tends to spread through the bloodstream and lymphatic system, increasing the risk of widespread disease.
Histological Features
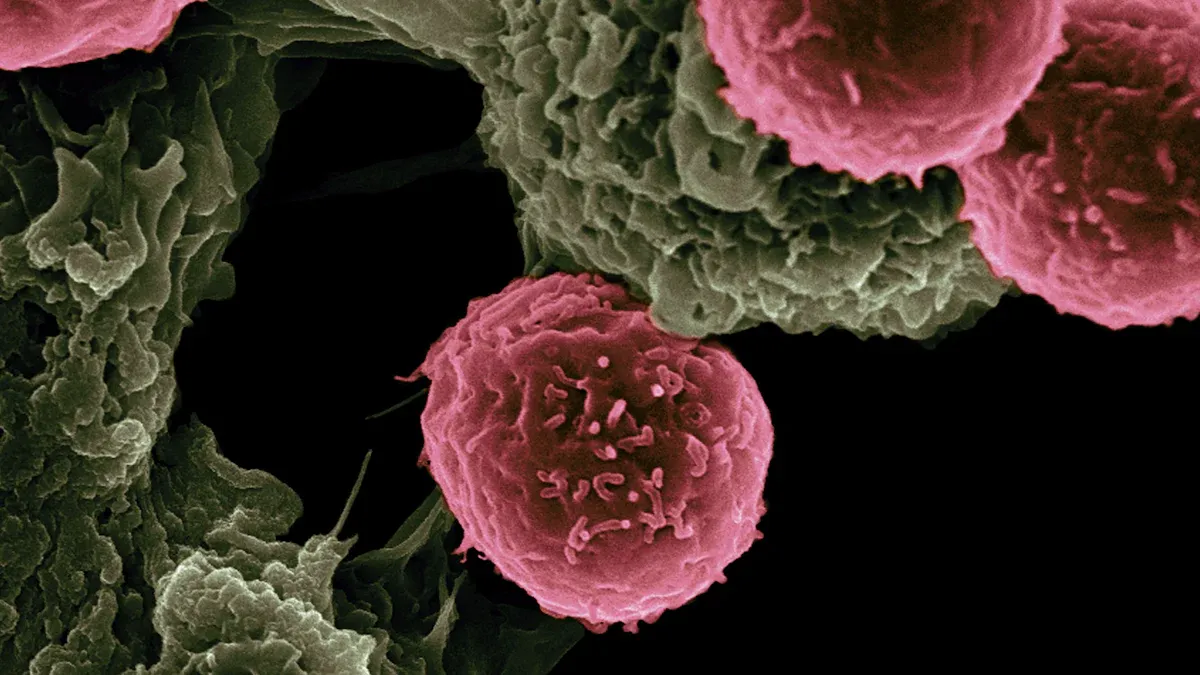
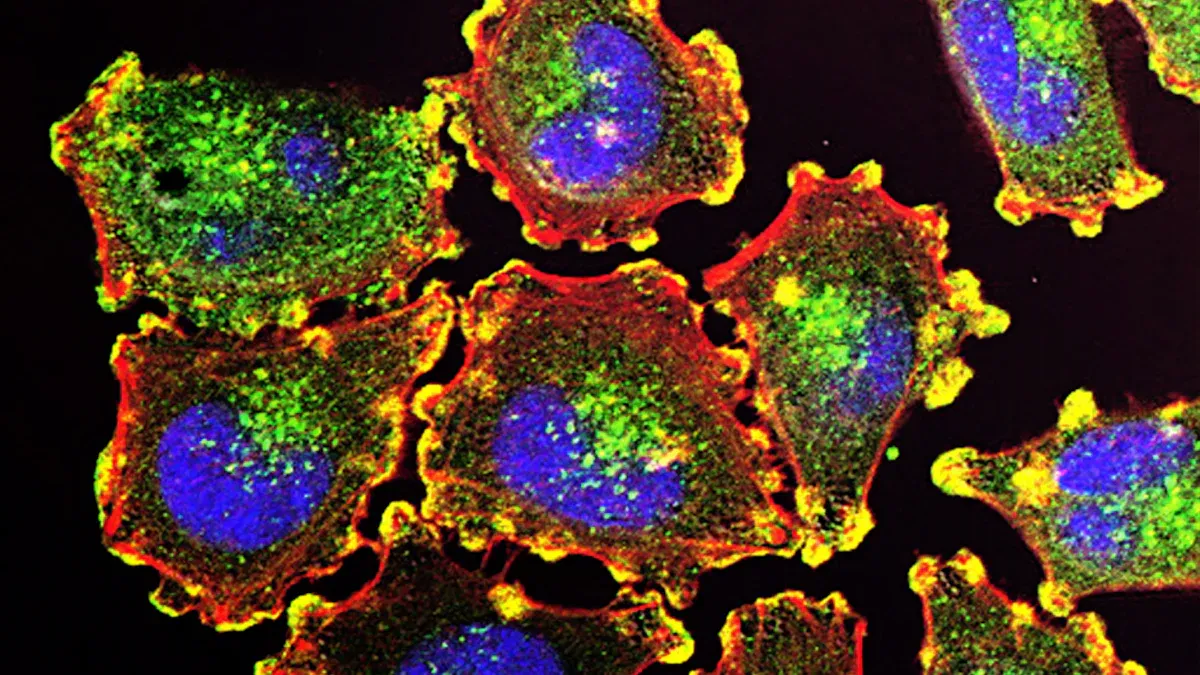
The unique histological features of embryonal carcinoma help doctors identify it under a microscope. These tumors display a variety of patterns, including solid, tubular (glandlike), and papillary structures. Key characteristics include:
Diffuse sheets of anaplastic cells with areas of necrosis.
Glandlike lumina lined by columnar cells, which may resemble yolk sac tumors.
Coagulative necrosis with dense eosinophilic debris.
Frequent mitoses and indistinct cell borders.
Variable architecture, such as tubulopapillary and embryoid bodies.
Doctors also look for spindle cell stroma surrounding tumor nests, which helps differentiate embryonal carcinoma from teratomas. These features highlight the tumor's complexity and aggressive behavior.
Risk Factors and Causes
Certain genetic and environmental factors increase your risk of developing embryonal carcinoma. Abnormal cell division in fetal gonocytes is believed to trigger tumor formation. Cryptorchidism, a condition where one or both testes fail to descend, is another significant risk factor. Studies show that about 10% of germ cell tumors occur in individuals with this condition. Understanding these risks can help you stay vigilant and seek medical advice if needed.
Symptoms of Embryonal Carcinoma
Early Symptoms
Embryonal carcinoma often begins with subtle signs that you might overlook. The most common early symptom is a lump in the affected area, such as the testis or ovary. This lump is usually painless but may occasionally cause discomfort. In rare cases, you might experience lumbar pain or renal colic, which feels like sharp pain in your lower back or side. These early symptoms can be easy to dismiss, but recognizing them promptly can make a significant difference in your treatment outcomes.
Advanced Symptoms
As embryonal carcinoma progresses, the symptoms become more pronounced and harder to ignore. You might notice swelling in the affected area, along with persistent pain. Fatigue and unexplained weight loss are also common as the tumor spreads to other parts of your body. If the cancer reaches your lungs, you could experience shortness of breath or even cough up blood. These advanced symptoms indicate that the tumor has metastasized, requiring immediate medical attention.
Symptoms Based on Tumor Location
The symptoms of embryonal carcinoma can vary depending on where the tumor develops. For example:
If the tumor spreads to your lungs, you might experience coughing up blood or difficulty breathing.
Tumors in the retroperitoneum can cause abdominal pain or swelling.
In the testis, you may notice a lump or swelling that feels firm to the touch.
Understanding how symptoms differ based on location can help you identify potential warning signs and seek timely medical care.
Diagnosis of Embryonal Carcinoma
Physical Examination and Medical History
Diagnosing embryonal carcinoma begins with a thorough physical examination and a review of your medical history. Your doctor will check for any lumps, swelling, or tenderness in the affected area, such as the testis or ovary. They may also ask about symptoms like pain, fatigue, or weight loss. Sharing your medical history, including any family history of cancer or conditions like cryptorchidism, helps your doctor assess your risk. This step lays the foundation for further diagnostic tests.
Imaging Tests
Imaging plays a vital role in confirming the presence of embryonal carcinoma and assessing its spread. Testicular ultrasonography is often the first imaging technique used. It helps identify the tumor and provides detailed images of the affected area. Advanced imaging methods, such as CT scans or MRIs, are used to evaluate the extent of the disease. These tests check for involvement of lymph nodes and distant metastasis, such as in the lungs or liver. Imaging results guide your doctor in planning the most effective treatment strategy.
Blood Tests and Tumor Markers
Blood tests are essential for diagnosing embryonal carcinoma. They measure specific tumor markers that are often elevated in this condition. These markers include:
Alpha fetoprotein (AFP)
Human chorionic gonadotropin (hCG)
Placental alkaline phosphatase (PLAP)
Lactic acid dehydrogenase (LDH)
Elevated levels of these markers not only confirm the diagnosis but also help monitor your response to treatment. Regular testing ensures that your doctor can track the tumor's progression or regression over time.
Biopsy and Histopathological Analysis
A biopsy is a critical step in diagnosing embryonal carcinoma. During this procedure, your doctor removes a small sample of tissue from the tumor. This sample undergoes detailed examination under a microscope to confirm the presence of cancer cells. A biopsy not only identifies the type of tumor but also provides essential information about its aggressiveness.
Histopathological analysis focuses on the microscopic features of the tumor. Pathologists look for specific characteristics that define embryonal carcinoma. These include sheets of undifferentiated cells, areas of necrosis, and glandlike structures. The presence of high mitotic activity, where cells divide rapidly, also indicates the tumor's aggressive nature. This analysis helps differentiate embryonal carcinoma from other germ cell tumors, ensuring you receive the most accurate diagnosis.
Your doctor may use different biopsy techniques depending on the tumor's location. For testicular tumors, an orchiectomy (surgical removal of the affected testis) often serves as both a diagnostic and therapeutic procedure. For ovarian tumors, a needle biopsy or surgical excision may be performed. Each method aims to collect a sufficient tissue sample while minimizing risks.
The results of the biopsy and histopathological analysis guide your treatment plan. They help determine whether the tumor is localized or has spread to other areas. This information allows your medical team to choose the most effective therapies, such as surgery, chemotherapy, or radiation. By understanding the tumor's unique features, you can feel more confident about the steps ahead in your treatment journey.
Tip: Always discuss biopsy results with your doctor to fully understand your diagnosis and treatment options.
Treatment Options for Embryonal Carcinoma
Surgery
Surgery is often the first step in treating embryonal carcinoma. It aims to remove the tumor and prevent its spread. For testicular tumors, doctors commonly perform a radical orchiectomy. This procedure removes the affected testicle and the spermatic cord. If the cancer has spread to nearby lymph nodes, retroperitoneal lymph node dissection (RPLND) may be necessary. This surgery targets lymph nodes in the abdomen, where testicular cancer often spreads.
Surgical Technique | Description |
|---|---|
Radical orchiectomy | Surgery to remove the testicle and spermatic cord. |
Retroperitoneal lymph node dissection (RPLND) | Involves the removal of lymph nodes that testicular cancer typically spreads to. |
These surgical techniques play a crucial role in managing the disease. They help doctors confirm the diagnosis and reduce the tumor burden.
Chemotherapy
Chemotherapy uses powerful drugs to destroy cancer cells. It is especially effective for embryonal carcinoma because this tumor responds well to these treatments. Doctors often recommend chemotherapy after surgery to eliminate any remaining cancer cells. Common drugs include cisplatin, etoposide, and bleomycin. These medications work by targeting rapidly dividing cells, which helps prevent the cancer from spreading further.
You may experience side effects like nausea, fatigue, or hair loss during chemotherapy. However, these effects usually subside after treatment ends. Your doctor will monitor your progress closely to adjust the treatment plan as needed.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. While it is less commonly used for embryonal carcinoma, it may be an option in specific cases. For example, if the tumor has spread to areas like the brain or spine, radiation can help shrink the tumor and relieve symptoms.
This treatment is highly targeted, which minimizes damage to surrounding healthy tissues. You might experience mild side effects, such as skin irritation or fatigue, but these are typically temporary. Radiation therapy can complement other treatments, such as surgery or chemotherapy, to improve outcomes.
Note: Your treatment plan will depend on factors like the tumor's size, location, and stage. Always discuss your options with your doctor to make informed decisions.
Multimodal Treatment Approaches
Treating embryonal carcinoma often requires a combination of therapies. This approach, called multimodal treatment, increases the chances of success by targeting the tumor from multiple angles. You may undergo surgery, chemotherapy, and radiation therapy as part of a comprehensive plan. Each method plays a unique role in managing the disease.
Why Combine Treatments?
Embryonal carcinoma spreads quickly, making it challenging to control with a single therapy. Surgery removes the primary tumor, but microscopic cancer cells may remain. Chemotherapy destroys these cells, reducing the risk of recurrence. Radiation therapy targets specific areas where the cancer has spread. By combining these methods, doctors can address both the visible tumor and any hidden cancer cells.
Tip: Multimodal treatment is tailored to your specific needs. Your doctor will consider factors like the tumor's size, location, and stage when designing your plan.
Examples of Multimodal Strategies
Surgery Followed by Chemotherapy: After removing the tumor, chemotherapy eliminates any remaining cancer cells. This approach is common for testicular embryonal carcinoma.
Chemotherapy and Radiation Therapy: If the cancer has spread to distant organs, these treatments work together to shrink tumors and prevent further spread.
Neoadjuvant Chemotherapy: In some cases, chemotherapy is given before surgery to shrink the tumor, making it easier to remove.
Benefits of Multimodal Treatment
Higher Success Rates: Combining therapies improves the chances of complete remission.
Reduced Recurrence: Addressing cancer on multiple fronts lowers the risk of it coming back.
Personalized Care: Your treatment plan is customized to give you the best possible outcome.
By understanding the importance of multimodal treatment, you can feel more confident about your care plan. This approach offers hope for managing even aggressive cancers like embryonal carcinoma.
Prognosis and Outlook for Embryonal Carcinoma
Factors Influencing Prognosis
Your prognosis depends on several key factors. The clinical stage of the tumor plays the most significant role. Early-stage embryonal carcinoma has a better outlook compared to advanced stages. Tumors with a higher proportion of embryonal carcinoma in mixed germ cell neoplasms tend to behave more aggressively. This increases the likelihood of tumor progression and metastasis. Age can also influence outcomes, as younger individuals often respond better to treatment. By understanding these factors, you can work closely with your doctor to develop a treatment plan tailored to your needs.
Survival Rates
Survival rates for embryonal carcinoma have improved significantly due to advancements in treatment. For early-stage cases, the five-year survival rate exceeds 90%. Even for advanced stages, combining surgery, chemotherapy, and other therapies has led to promising outcomes. These statistics highlight the importance of early detection and comprehensive care. While survival rates provide a general idea, your individual prognosis will depend on factors like tumor stage, treatment response, and overall health.
Importance of Follow-Up Care
Follow-up care is essential for managing embryonal carcinoma. After completing treatment, regular check-ups help monitor for recurrence or complications. Your doctor may recommend imaging tests, blood work, or physical exams during these visits. Staying consistent with follow-up appointments ensures that any issues are detected early. This proactive approach improves long-term outcomes and gives you peace of mind. By prioritizing follow-up care, you can take an active role in maintaining your health and recovery.
Embryonal carcinoma is an aggressive cancer that demands your attention. Its rapid growth and potential to spread make early detection essential. Recognizing symptoms and acting quickly can significantly improve your chances of recovery.
Treatment options, including surgery, chemotherapy, and multimodal approaches, have proven highly effective. Many patients achieve positive outcomes when they receive timely and comprehensive care.
Remember: If you notice unusual symptoms or have concerns, consult a healthcare professional immediately. Taking action early could save your life.
FAQ
What is the difference between pure and mixed embryonal carcinoma?
Pure embryonal carcinoma consists only of embryonal carcinoma cells. Mixed embryonal carcinoma includes other germ cell tumor types, such as yolk sac tumors or teratomas. Mixed forms are more common and may require different treatment approaches.
Can embryonal carcinoma occur in women?
Yes, embryonal carcinoma can develop in women, though it is rare. It typically arises in the ovaries and accounts for a small percentage of ovarian germ cell tumors. Early detection improves treatment outcomes.
How is embryonal carcinoma different from seminoma?
Embryonal carcinoma grows faster and spreads more aggressively than seminoma. It also has distinct histological features under a microscope. Seminomas usually respond well to radiation, while embryonal carcinoma often requires chemotherapy or multimodal treatment.
Are there any lifestyle changes that can reduce the risk of embryonal carcinoma?
While you cannot completely prevent embryonal carcinoma, maintaining a healthy lifestyle may help. Regular self-examinations and prompt medical attention for unusual symptoms can aid in early detection. Addressing risk factors like cryptorchidism through surgery may also lower your risk.
What should you do if you suspect symptoms of embryonal carcinoma?
Consult a healthcare professional immediately. Early symptoms, such as a painless lump or swelling, require prompt evaluation. Early diagnosis and treatment significantly improve your chances of recovery.
Tip: Keep track of any unusual changes in your body and seek medical advice without delay.
See Also
Essential Insights Into Carcinoid Tumors You Need
Key Information Regarding Basaloid Squamous Lung Cancer
A Comprehensive Guide To Astrocytoma Variants Explained
Simplifying B-Cell Prolymphocytic Leukemia For Better Understanding

