Emerging Breakthroughs in Cancer Imaging Technologies
Cancer imaging has entered a new era, transforming how you approach diagnosis and treatment. Emerging technologies in cancer imaging are making healthcare in 2025 faster, more precise, and accessible. For instance, AI systems now reduce unnecessary breast cancer screenings by 42% and cut false positives by 31.1%, saving billions annually. Tools like the PrismNN neural network can detect pancreatic cancer 18 months earlier, catching 3.5 times more cases than before. These innovations empower you with earlier, more accurate detection, improving outcomes and reshaping global healthcare.
Key Takeaways
AI and machine learning make cancer imaging more accurate. This helps find cancer earlier and improves patient care.
New tools like photon-counting CT and whole-body MRI give clear pictures. They use less radiation and make diagnoses better.
Portable imaging machines help people in remote areas. They allow faster cancer detection and treatment.
Combining genetics with imaging helps create custom treatments. This improves how well patients respond and live longer.
Smart imaging tools, like teleradiology, let doctors work together quickly. This makes diagnosing faster and more accurate.
AI and Machine Learning in Imaging

Artificial intelligence (AI) and machine learning (ML) are revolutionizing cancer imaging. These technologies enhance diagnostic accuracy, enable early detection, and provide deeper insights through multi-modal platforms. By leveraging AI, you can access faster, more precise imaging solutions that improve patient outcomes.
Diagnostic accuracy improvements with AI
AI has significantly improved the accuracy of cancer diagnosis. Advanced algorithms analyze imaging data with remarkable precision, often surpassing human performance. For example, AI models like YOLO and Custom CNN achieve diagnostic accuracies of up to 98.7%. The following table highlights key metrics demonstrating AI's effectiveness:
Metric | Value (%) |
|---|---|
AUC | 91 |
Sensitivity | 86 |
Specificity | 82 |
Additionally, comparative studies show that AI models outperform healthcare experts in sensitivity and specificity:
Metric | AI Models (%) | Healthcare Experts (%) |
|---|---|---|
Sensitivity | 87 | 86.4 |
Specificity | 92.5 | 90.5 |
These advancements ensure you receive more accurate diagnoses, reducing the risk of false positives and negatives. Clinical studies, such as Hawkins 2016 and Liu 2017, further validate AI's potential. For instance, Hawkins 2016 demonstrated an AUC of 0.83 in predicting lung cancer risk using CT imaging and machine learning algorithms.
Predictive analytics for early cancer detection
Predictive analytics powered by AI plays a crucial role in early cancer detection. By analyzing patterns in imaging data, AI identifies malignancies before they spread. This approach has proven effective in clinical trials, such as the Galleri trial, which explores cell-free DNA for early detection. Similarly, CancerSEEK detects eight common cancer types with an impressive AUC of 91%.
Key benefits of predictive analytics include:
Early detection supports national cancer control initiatives.
Screening programs for cervical, breast, and colorectal cancers reduce advanced-stage diagnoses.
Machine learning applied to liquid biopsies achieves high accuracy in detecting cancer.
These advancements enable you to benefit from timely interventions, improving survival rates and overall health outcomes.
Multi-modal AI platforms for enhanced imaging analysis
Multi-modal AI platforms integrate data from various sources, such as radiology and histology, to provide comprehensive insights. These platforms enhance cancer imaging analysis by identifying associations across modalities. For instance, AI can predict histology subtypes from radiomics features, offering non-invasive alternatives to traditional biomarkers.
The table below outlines the capabilities of multi-modal AI platforms:
Evidence Description | Key Findings |
|---|---|
AI identifies associations across modalities, such as mutations from images. | |
Discovery of morphological associates | AI reveals cost-efficient biomarker surrogates. |
Prediction of histology subtypes | AI predicts subtypes from radiomics features, aiding non-invasive diagnostics. |
Performance in predicting outcomes | AI predicts survival, treatment response, and recurrence using multi-modal data. |
By leveraging these platforms, you gain access to cutting-edge imaging technologies that support personalized and precise cancer care.
Emerging Technologies in Cancer Imaging

Advancements in cancer imaging are transforming how you detect and diagnose cancer. Emerging technologies in cancer imaging, such as photon-counting CT, digital SPECT, and whole-body MRI, are setting new standards for precision and comprehensiveness. These innovations offer you better image quality, reduced radiation exposure, and improved diagnostic accuracy.
Photon-counting CT for high-resolution imaging
Photon-counting CT (PCCT) represents a significant leap forward in imaging technology. Unlike traditional CT scanners, PCCT uses photon-counting detectors to measure individual X-ray photons, resulting in sharper images and enhanced tissue characterization. This technology benefits you by improving diagnostic accuracy and reducing radiation exposure.
Key Advantages of Photon-counting CT:
Enhanced accuracy in imaging.
Improved tissue characterization.
Reduction of artifacts.
Decreased radiation dosing.
A comprehensive review of 155 studies highlighted PCCT's ability to enhance imaging quality across various applications, including thoracic and abdominal imaging. For example, PCCT improves lung density evaluation by reducing electronic noise and managing noise more effectively. It also enhances the detection of low-contrast nodules, such as ground-glass nodules, with a fivefold higher detectability index for a 4 mm nodule compared to traditional methods.
The table below summarizes additional findings:
Evidence Description | Findings |
|---|---|
PCD-CT image quality | Better image quality and improved reader confidence, aiding tumor response evaluation. |
Iodine concentration correlation | Higher normalized IC values associated with lymphovascular invasion and predictive accuracy for treatment response (AUC = 0.85). |
These advancements make photon-counting CT a powerful tool for high-resolution imaging, helping you achieve earlier and more accurate cancer detection.
Digital SPECT for precise cancer detection
Digital single-photon emission computed tomography (SPECT) is another emerging technology in cancer imaging. By combining molecular imaging with radiotracers, digital SPECT allows you to evaluate metabolic activity visually and quantitatively. This capability enhances diagnostic precision and interpretation.
How Digital SPECT Benefits You:
Provides detailed metabolic activity assessments.
Uses radiotracers for both visual and quantitative evaluations.
Offers standardized interpretations for improved diagnostic outcomes.
SPECT/CT has been integrated into various clinical scenarios for cancer detection. While some studies suggest limited improvements in sensitivity and specificity for certain cancers, molecular imaging techniques like SPECT have shown promise in enhancing diagnostic accuracy. For instance, the quantitative evaluation of images allows for more precise assessments of cancerous tissues.
The table below highlights the sensitivity and dose range of SPECT compared to other modalities:
Imaging Modality | Sensitivity | Dose Range (MBq) |
|---|---|---|
10^-6 | 0.2–1 (89Zr-PANC1) to 5–10 (111In) |
Digital SPECT continues to evolve, offering you a reliable option for precise cancer detection.
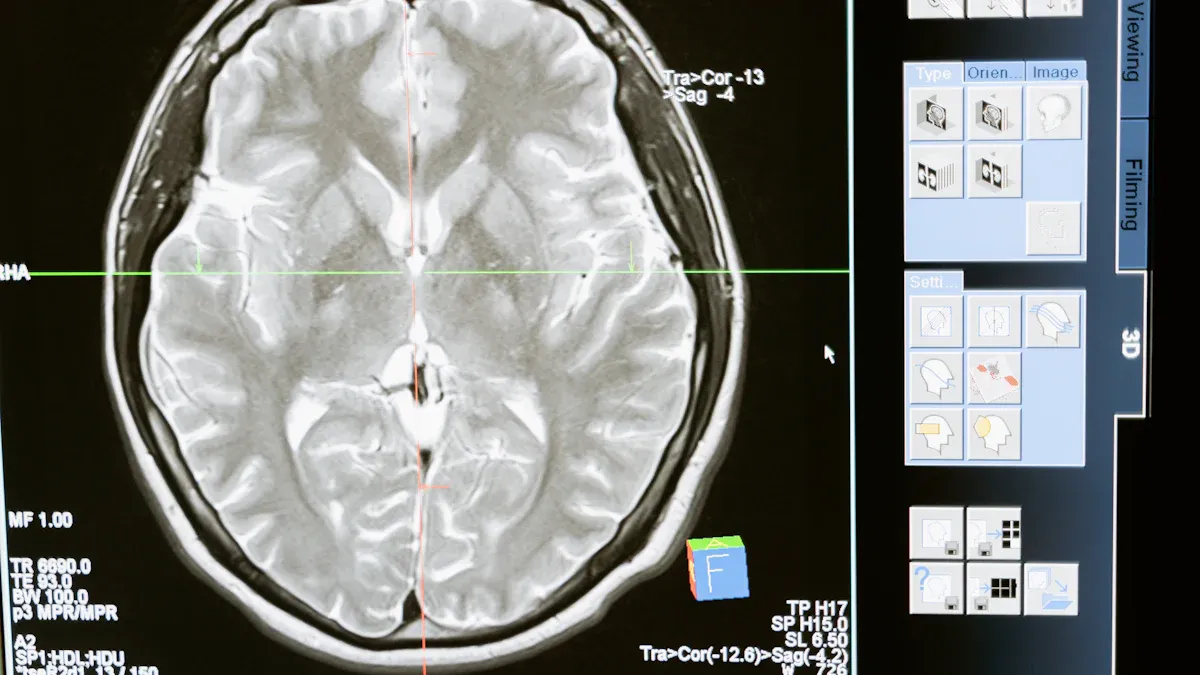
Whole-body MRI for comprehensive diagnostics
Whole-body MRI (WB-MRI) is revolutionizing cancer diagnostics by providing a non-invasive, radiation-free imaging solution. This technology uses strong magnetic fields and radiofrequency bursts to create detailed images of internal structures, making it ideal for comprehensive cancer screening.
Advantages of WB-MRI:
Non-ionizing technology ensures patient safety.
Superior soft tissue contrast resolution.
Effective in detecting a variety of cancers, including multiple myeloma and bone metastases.
Allows whole-body scanning in a single session.
WB-MRI has proven effective in detecting renal, hepatic, pulmonary, and colonic malignancies. It offers high-resolution imaging, enabling early detection of both benign and malignant lesions. For high-risk individuals, WB-MRI provides a convenient and thorough screening option.
This imaging modality also avoids the use of ionizing radiation, preserving a higher signal-to-noise ratio (SNR) for clearer images. However, it may require anti-aliasing pre-processing to reduce distortions. By choosing WB-MRI, you gain access to a safe and comprehensive diagnostic tool.
Emerging technologies in cancer imaging, such as photon-counting CT, digital SPECT, and whole-body MRI, are paving the way for more accurate and accessible cancer care. These innovations empower you with better tools for early detection and diagnosis, ultimately improving treatment outcomes.
Technological Innovations
Fluorescent imaging systems for real-time surgical precision
Fluorescent imaging systems are transforming cancer surgeries by providing real-time intraoperative guidance. These systems enhance surgical precision without disrupting the workflow. For example:
Fluorescence-guided surgery (FGS) improves decision-making during procedures.
Techniques like fluorescence cholangiography help assess blood flow and identify cancerous tissues.
Fluorescence-based angiography aids in detecting tumors with high accuracy.
A phase II clinical trial using the CEA-targeting agent SGM-101 demonstrated the effectiveness of these systems. The trial achieved a sensitivity of 96% and a specificity of 63% in detecting primary tumors in colorectal cancer patients. In over 20% of cases, surgeons altered their plans based on fluorescence imaging results. This highlights how these systems improve outcomes by enabling more precise tumor removal.
Mobile 3D CT imaging for early lung cancer detection
Mobile 3D CT imaging is a game-changer for early lung cancer detection. Unlike traditional CT scanners, mobile units bring advanced imaging capabilities directly to patients. This innovation allows you to access high-quality scans in outpatient settings or even remote areas. The portability of these devices ensures faster diagnoses and reduces the need for hospital visits. By detecting lung cancer at earlier stages, mobile 3D CT imaging improves survival rates and enhances treatment planning.
Image-guided injection systems for targeted treatments
Image-guided injection systems are revolutionizing cancer treatment by enabling precise drug delivery. Conventional treatments often affect healthy tissues, causing side effects. These systems use molecular imaging to locate tumors and guide injections directly to the target area. Key benefits include:
Reduced systemic side effects.
Enhanced drug efficacy through targeted delivery.
Earlier assessment of treatment responses using contrast agents.
By visualizing molecular features of tumors, these systems support personalized treatment approaches. They also allow you to monitor progress more effectively, ensuring optimal care.
Emerging technologies in cancer imaging, such as fluorescent imaging systems, mobile 3D CT imaging, and image-guided injection systems, are paving the way for more precise and accessible cancer care. These innovations empower you with tools that improve detection, diagnosis, and treatment outcomes.
Personalized Imaging
Precision medicine through tailored imaging
Tailored imaging is at the heart of precision medicine, offering you a personalized approach to cancer care. By combining molecular imaging with systems biology, healthcare providers can evaluate the unique biological components of your tumor. This enables the development of treatment strategies specifically designed for your condition. High-throughput technologies, such as radiogenomics and radiomics, play a pivotal role in identifying disease-specific imaging features. These features help categorize patients into subgroups that benefit from targeted therapies.
Imaging also supports initial staging and treatment planning. It assesses tumor burden and prognosis, ensuring that your therapy aligns with your specific needs. For example, metabolic imaging, enhanced by artificial intelligence, predicts patient outcomes more effectively. This integration of imaging and AI addresses clinical challenges, improving the precision of treatment targeting.
Did you know? Radiomics extracts data from medical images to uncover patterns that might not be visible to the human eye. This technology bridges the gap between imaging and personalized care.
Integration of genomics and imaging for personalized care
The fusion of genomics and imaging has transformed cancer diagnostics and treatment. This integration allows doctors to develop personalized strategies that significantly improve your outcomes. For instance, radiogenomics links imaging phenotypes with genetic expressions, creating predictive models based on imaging features.
The measurable benefits of this approach are evident in clinical outcomes:
Outcome Type | Precision Medicine Arm | Non-Personalized Treatment Arm |
|---|---|---|
Response Rates | 4.9% | |
Progression-Free Survival | 5.7 months | 2.95 months |
Objective Response Rates | 16.4% | 5.4% |
10-Year Overall Survival Rates | 6% | 1% |
This integration also enhances patient stratification, treatment planning, and noninvasive predictions. By combining imaging features with genomic data, doctors can create more accurate prognostic models, ensuring you receive the most effective care.
Patient-centric imaging approaches for better outcomes
Patient-centric imaging focuses on improving your experience and outcomes. Advanced imaging techniques enable earlier diagnosis and intervention, helping identify the best treatment options for you. These methods also monitor therapy progress, allowing timely adjustments to ineffective treatments.
Evidence Type | Description |
|---|---|
Clinical Evidence | Advanced imaging techniques remain underutilized despite their potential. |
Simulation Analysis | Increased investment in imaging could yield better cancer management. |
Patient Engagement | Collaborative goal setting enhances the value of imaging in treatment. |
Early diagnosis improves survival rates.
Imaging helps tailor treatments to your specific needs.
Therapy monitoring ensures timely modifications for better results.
By prioritizing your needs, patient-centric imaging ensures that cancer care becomes more effective and compassionate.
Accessibility and Global Impact
Portable imaging devices for underserved areas
Portable imaging devices are transforming cancer diagnostics in underserved regions. These innovations bring advanced imaging technologies directly to patients, eliminating the need for long-distance travel. Mobile mammography units and portable CT scanners, for example, provide critical diagnostic services in rural and disaster-stricken areas. Their mobility ensures immediate medical responses, reducing delays in care.
Low-cost solutions like the OVision framework further enhance access to precision diagnostics. This portable device classifies histologic subtypes, enabling personalized treatment plans even in resource-limited settings. Modular imaging suites also play a vital role by allowing outpatient clinics to offer advanced imaging locally. Upgrading older equipment in safety-net hospitals ensures that modern imaging technologies reach more communities.
Innovation Type | Description |
|---|---|
Mobile mammography coaches and portable CT scanners bring imaging services directly to patients. | |
Modular Imaging Suites | Smaller, scalable imaging systems allow outpatient clinics to provide advanced imaging locally. |
Equipment Updates | Upgrading older equipment in safety-net hospitals ensures access to modern imaging technology. |
These advancements bridge the gap in healthcare access, ensuring you receive timely and accurate cancer diagnostics.
Teleradiology for remote diagnostics and collaboration
Teleradiology has revolutionized remote cancer diagnostics by enabling real-time collaboration between specialists. This technology allows radiologists to interpret images from anywhere, ensuring faster and more accurate diagnoses. During the COVID-19 pandemic, teleradiology networks demonstrated resilience, handling increased demand for oncological imaging. Mobile mammography units equipped with teleradiology reduced diagnostic turnaround times to just 12 hours in India, significantly improving early detection rates.
Evidence Type | Description |
|---|---|
Improved Quality | Enhanced efficiency in treatment and image interpretation, reducing complications. |
Reduced Transfers | Fewer unnecessary patient transfers and trips. |
Reduced Imaging | Lower repeat imaging rates, improving patient safety. |
Reduced Waiting Time | Faster image interpretation for quicker diagnoses. |
Equivalent Diagnosis | Digital methods match conventional diagnostic accuracy. |
By enabling real-time comparisons with previous scans, teleradiology enhances treatment monitoring and recurrence detection. This approach ensures you receive precise and timely care, regardless of location.
Bridging healthcare disparities with innovative imaging solutions
Innovative imaging technologies are closing the gap in global healthcare disparities. AI-powered tools, for instance, improve early cancer detection in low- and middle-income countries (LMICs). These algorithms identify malignant nodules on chest X-rays with greater accuracy than experienced radiologists, addressing the shortage of specialists in these regions.
In Nepal, AI-powered diagnostic tools have been successfully deployed in remote health centers. This initiative demonstrates how technology can improve access to quality care. By integrating AI into imaging workflows, healthcare providers can offer accurate and affordable diagnostics to underserved populations.
AI enhances early cancer detection in LMICs.
Algorithms outperform radiologists in identifying malignant nodules on chest X-rays.
Remote health centers in Nepal benefit from AI-powered diagnostic tools.
These breakthroughs ensure that advanced cancer imaging becomes accessible to everyone, regardless of geographic or economic barriers.
Sustainability and Ethical Considerations
Eco-friendly imaging technologies for reduced environmental impact
Imaging technologies play a vital role in cancer care but significantly contribute to environmental challenges. CT and MRI scanners alone account for about 4% of a hospital's annual energy consumption. For perspective:
A single CT scanner uses as much energy annually as five households.
An MRI scanner consumes energy equivalent to 26 households.
Optimizing idle and off states in imaging equipment can reduce energy use without compromising the number of scans. This approach aligns with the growing demand for sustainable healthcare practices. In fact, 92% of patients in the UK prioritize eco-friendly solutions in medical care. Radiology departments, as major contributors to healthcare emissions, must adopt greener practices to reduce their carbon footprint. The healthcare sector collectively emits 748 million metric tons of CO2 annually across the US, Australia, England, and Canada. Transitioning to energy-efficient imaging systems can significantly lower this impact.
Data privacy challenges in AI-driven imaging
AI-driven imaging relies on vast datasets, including clinical and genomic information, to improve cancer diagnostics. However, protecting patient privacy remains a critical challenge. Establishing secure data-sharing frameworks is essential for research collaborations, but compliance with privacy regulations often complicates this process.
The implementation of differential privacy (DP) in medical AI highlights these challenges. Balancing diagnostic accuracy with privacy is difficult, especially when facing threats like data reconstruction attacks. These attacks pose a greater risk than membership inference attacks, as they can reconstruct sensitive patient information.
AI algorithms require extensive data, increasing the risk of privacy breaches. A 2018 study revealed that despite de-identification efforts, algorithms could re-identify 85.6% of adults and 69.8% of children.
Without centralized protocols for data encryption and sharing, the risk of re-identification remains significant. Public-private partnerships have also raised concerns about the control and use of patient data, emphasizing the need for systemic oversight.
Ensuring equitable access to advanced imaging technologies
Advanced imaging technologies often remain inaccessible to underserved populations. Bridging this gap requires innovative solutions. Portable imaging devices, such as mobile CT scanners, bring diagnostic tools to remote areas. These devices eliminate the need for long-distance travel, ensuring timely care.
AI-powered imaging tools also enhance accessibility. In Nepal, remote health centers use AI to detect cancer with high accuracy, addressing the shortage of specialists. By integrating AI into imaging workflows, healthcare providers can offer affordable diagnostics to low-income regions.
Equitable access to imaging technologies ensures that everyone, regardless of location or economic status, benefits from advancements in cancer care.
The breakthroughs in cancer imaging technologies in 2025 offer you unprecedented opportunities for earlier detection, precise diagnosis, and personalized treatment. Tools like AI-driven imaging, photon-counting CT, and portable devices are reshaping how you access and benefit from cancer care.
These advancements not only improve outcomes but also make diagnostics more accessible to underserved communities.
As these innovations continue to evolve, you can look forward to a future where cancer care becomes faster, more accurate, and universally available. The horizon of cancer imaging holds immense promise, empowering you with hope and better health outcomes.
FAQ
What is the role of AI in cancer imaging?
AI improves cancer imaging by analyzing data faster and more accurately than humans. It detects patterns, predicts outcomes, and reduces false positives. You benefit from earlier diagnoses and better treatment planning, which increases survival rates.
Are portable imaging devices reliable for cancer detection?
Yes, portable imaging devices provide accurate results comparable to traditional systems. They bring advanced diagnostics to underserved areas, ensuring you receive timely care. These devices are especially useful in rural or remote locations.
How does whole-body MRI differ from other imaging methods?
Whole-body MRI uses magnetic fields instead of radiation, making it safer for you. It provides detailed images of soft tissues and detects multiple cancers in one session. This method is ideal for comprehensive screening.
Can imaging technologies reduce treatment side effects?
Yes, image-guided systems deliver treatments directly to tumors, sparing healthy tissues. This targeted approach minimizes side effects and improves drug effectiveness. You experience better outcomes with fewer complications.
Are these technologies accessible to everyone?
Innovations like portable devices and AI-powered tools aim to make imaging accessible globally. They address healthcare disparities by reaching underserved areas. You can expect more equitable access as these technologies continue to evolve.
See Also
Recognizing Duodenal Cancer Symptoms And Available Treatments
Cholangiocarcinoma Overview: Key Features And Insights
Key Characteristics And Insights About Hemangioblastoma

