Why cancer survivors are not getting enough exercise support

Many cancer survivors miss out on vital exercise for cancer survivors support due to challenges faced by healthcare providers. These include safety concerns, especially for patients with bone metastases, and limited time during consultations. Providers often lack up-to-date knowledge about exercise for cancer survivors guidelines or feel uncertain about referring patients to suitable programs. Additional barriers arise from under-resourced health systems, lack of government support, and the common belief among families that rest is better than activity. This gap between what is known and what is practiced leaves many survivors without the proven benefits of exercise for cancer survivors.
Key Takeaways
Exercise helps cancer survivors improve their health, mood, and chances of living longer.
Many healthcare providers know exercise is important but lack training and time to support survivors properly.
Limited resources and unclear referral systems make it hard for survivors to access exercise programs.
System changes, clear referral paths, and better provider training can increase exercise support for survivors.
Making exercise a routine part of cancer care can help survivors feel stronger and live better lives.
Exercise for Cancer Survivors

Health and Quality of Life
Exercise for cancer survivors offers a wide range of health and quality of life improvements. Regular physical activity helps reduce symptoms and enhances functional capacity. Many survivors report better perceptions of their health and increased bone density, especially when resistance training is included. Pain management becomes more effective, and physical functioning improves, making daily activities easier after treatment.
Survivors often notice mental health benefits, such as lower levels of depression and anxiety. Exercise also encourages positive social engagement, which can boost mood and energy. Many find that staying active serves as a valuable coping mechanism and a source of personal satisfaction. For those managing long-term effects of cancer treatment, regular exercise becomes an essential part of their routine.
Some of the most significant benefits include:
Improved bone density and muscle strength
Enhanced recovery after surgery or treatment
Reduced fatigue and emotional distress
Better management of lymphedema symptoms
Increased energy and positive mood
Tailored exercise prescriptions address the unique needs of different cancer populations. Ongoing research continues to support the safety and effectiveness of exercise interventions across the cancer journey.
Survival Benefits
Exercise for cancer survivors does more than improve daily life; it can also extend survival. Studies involving thousands of survivors show that higher levels of physical activity after treatment are linked to survival rates similar to or even better than those of the general population. For example, colon cancer patients who engaged in regular exercise had much higher survival rates than those who remained inactive.
A large analysis of nearly 91,000 survivors found that moderate to vigorous activity, such as brisk walking for a few hours each week, improved overall survival across many cancer types. Even modest amounts of exercise made a difference. Clinical trials have shown that structured exercise programs can reduce mortality by over a third compared to standard care alone. These findings highlight the importance of making exercise a standard part of cancer care.
Guidelines and Recommendations
COSA Statement
The Clinical Oncology Society of Australia (COSA) has issued a clear position statement on exercise for cancer survivors. COSA recommends that all survivors receive advice to avoid inactivity and return to daily activities as soon as possible after surgery or treatment. Oncology clinicians should encourage gradual progression and refer patients to supervised programs when needed. Despite strong agreement among healthcare professionals about the benefits of exercise, only a small portion routinely apply COSA recommendations in practice. Surveys show that while 94% of oncology professionals believe exercise helps cancer patients, only 35% use these guidelines regularly. Many organizations have not updated their practices to reflect COSA’s advice. Barriers such as limited resources, unclear roles, and financial constraints often prevent full adoption.
Standard of Care
Major health organizations, including the American College of Sports Medicine (ACSM), have developed detailed guidelines for exercise for cancer survivors. These recommendations focus on safety, individualization, and collaboration between oncology teams and exercise specialists. The table below summarizes key points:
Exercise Type | General ACSM & PAGA Recommendations for Cancer Survivors | Specific Modifications by Cancer Type |
|---|---|---|
Aerobic Activity | At least 150 minutes/week moderate-intensity or 75 minutes/week vigorous-intensity activity. Avoid inactivity. | Breast, prostate, and hematologic (no HSCT): follow general guidelines. Colon cancer with stoma: avoid abdominal strain. |
Resistance Training | Moderate- or high-intensity muscle-strengthening for all major muscle groups at least 2 days/week. | Breast cancer: start supervised, progress slowly. Colon cancer with stoma: lower resistance, slow progression. |
Flexibility | Stretch major muscle groups and tendons on days other activities are performed. | Colon cancer with ostomy: avoid excess abdominal pressure. Breast cancer: follow general guidelines. |
Exercise is safe for most survivors and does not interfere with treatment. Walking and stationary cycling are good starting points. Programs should be tailored to each survivor’s needs and treatment status.
International guidelines reflect a global effort to make exercise a standard part of cancer care. Organizations like the International Society of Exercise Oncology (ISEO) work to translate research into practice and train professionals worldwide. These efforts highlight the importance of integrating exercise for cancer survivors into routine care to improve outcomes and quality of life.
Knowledge-Practice Gap
Provider Awareness
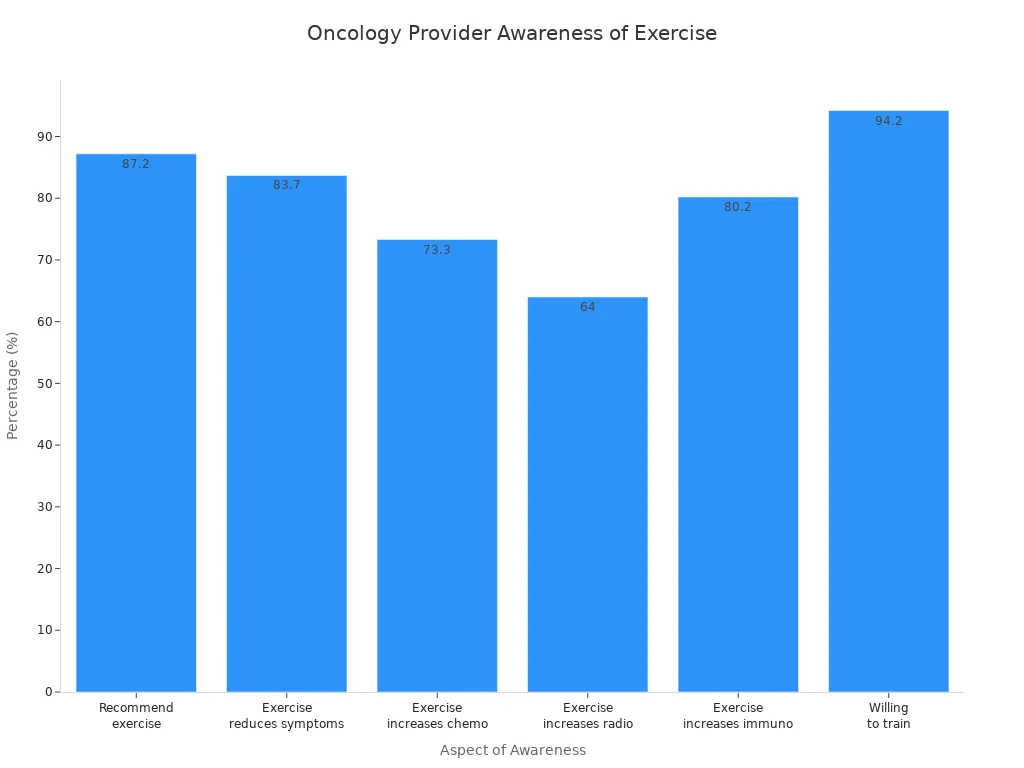
Many oncology providers recognize the value of exercise for cancer survivors. Most recommend physical activity to their patients and believe it can reduce symptoms and improve treatment outcomes. However, gaps remain in their training and confidence, especially regarding specific exercise guidelines and safety. The following table highlights key findings from recent surveys:
Aspect | Finding |
|---|---|
Percentage of oncology physicians recommending exercise to cancer patients | |
Physicians who believe exercise reduces cancer-related symptoms | 83.7% |
Physicians who believe exercise increases chemotherapy effectiveness | 73.3% |
Physicians who believe exercise increases radiotherapy effectiveness | 64% |
Physicians who believe exercise increases immunotherapy effectiveness | 80.2% |
Physicians willing to receive training on exercise effects in cancer | 94.2% |
Main reasons for not recommending exercise | Lack of training, uncertainty about exercise type, safety concerns |
Experts call for a shift in oncology similar to changes seen in cardiology. Initiatives like the American College of Sports Medicine's 'Moving Through Cancer' aim to make exercise a standard part of cancer care by 2029. Providers often lack time and training to discuss exercise, so these programs offer resources and referral pathways to help bridge the gap.
Real-World Practice
In clinical settings, the delivery of exercise for cancer survivors often falls short of evidence-based recommendations. Several factors contribute to this gap:
Healthcare professionals have broad knowledge but limited specialized training in exercise oncology.
Safety concerns about unsupervised home-based exercise persist, even though home programs are convenient and affordable.
Many survivors do not know about or cannot access exercise-related services.
Misconceptions remain that patients undergoing intensive treatment should avoid physical activity.
Guidelines describe what to do but rarely explain how to implement exercise in real-world care.
Multidisciplinary teams, patient education, and investment in facilities are needed to improve access.
Public education can help change beliefs about the safety and benefits of exercise during cancer treatment.
Structured, personalized exercise programs improve survival and quality of life, but real-world practice still lags behind. Collaboration among oncologists, nurses, and exercise professionals, along with clear referral systems, can help close the knowledge-practice gap.
Barriers in Oncology Care

Training and Confidence
Oncology providers face significant challenges in delivering exercise support to cancer survivors. Many lack specialized training in exercise oncology. This gap in education leads to uncertainty about which types of exercise are safe and effective. Providers often feel unsure about how to screen patients for suitability or how to tailor recommendations. Safety concerns, especially for those with bone metastases, add to this hesitation. Providers may avoid discussing exercise if they do not feel confident in their knowledge or ability to refer patients to appropriate programs.
A nurse described the impact of limited resources and training: “It’s not worth bringing it up. You don’t plant the seed unless you can water it.” This statement highlights how lack of confidence and support can prevent providers from even starting conversations about exercise.
Time constraints during clinical visits also reduce opportunities for providers to educate patients. Without adequate training and support, many providers miss the chance to encourage exercise for cancer survivors.
Resource Limitations
Resource limitations create major obstacles for integrating exercise into standard cancer care. Many exercise oncology programs do not receive comprehensive Medicare or third-party payer coverage. Programs often depend on philanthropic or health system funding, which leads to inconsistent and inequitable access. Staffing shortages and lack of sustainable funding restrict program expansion, especially in regional and rural areas.
Programs struggle to hire qualified personnel and purchase necessary equipment.
Economic barriers, such as the absence of reimbursement policies for exercise professionals, threaten program sustainability.
Lack of systematic integration into medical care models limits referral options for oncology clinicians.
Programs that succeed often align with healthcare leadership priorities and secure resources for workforce sustainability.
Funding challenges remain a critical issue, highlighting the need for policy changes and third-party payer reimbursement.
These resource constraints limit the reach of exercise programs and make it difficult for survivors to access consistent support.
Referral Challenges
Referral pathways for exercise programs remain fragmented and difficult to navigate. Many oncology providers lack clear guidance on how to refer patients. Health systems often do not have infrastructure for assessment, triage, and referral to exercise programs. Referral processes are rarely integrated into electronic medical records, making them cumbersome and time-consuming.
Providers face time constraints and skepticism about the feasibility of referrals.
Poor knowledge about screening and referral pathways hinders effective referrals.
Institutional support and leadership buy-in are often missing, impeding adoption of exercise referral practices.
Geographic inequities mean that patients in rural or socioeconomically disadvantaged areas have less access to exercise oncology programs.
Patient-level barriers, such as fatigue, misconceptions, and logistical challenges, also affect referral uptake.
Low organizational buy-in leads to poor service penetration and utilization, with service reach as low as 10-14%. Despite guidelines, only a small percentage of patients receive referrals to exercise programs. These interrelated barriers across organizational, provider, and patient levels prevent the integration of exercise for cancer survivors into routine care.
Why Barriers Persist
Systemic Issues
Healthcare organizations face several systemic issues that make it hard to provide ongoing exercise support for cancer survivors. Many survivors do not have the knowledge or skills to move from supervised therapy to exercising on their own. Financial resources are often limited, and municipal subsidies for exercise programs can be inconsistent. Work and family responsibilities also create barriers, making it difficult for survivors to find time for physical activity.
Physical therapists sometimes feel unprepared to guide survivors after therapy ends. Most regular fitness settings do not have staff with oncology expertise. Postgraduate education for physical therapists only covers some behavioral change techniques, so there are gaps in helping survivors stick with exercise long-term. Insurance and reimbursement policies can also cut therapy short, ending support before survivors are ready to continue on their own.
These systemic challenges combine to limit access and make it hard for survivors to maintain healthy activity levels after treatment.
Role Perceptions
Provider attitudes and beliefs play a big role in the delivery of exercise support. Many providers know that physical activity helps cancer patients, but they often hesitate to start conversations about it. They may feel they lack the right expertise or do not have enough time during clinic visits. Some providers feel unsure about how to recommend the right exercise for each patient, so they rarely document or discuss exercise plans.
Most providers prefer to refer patients to exercise specialists instead of giving advice themselves. However, patients often want guidance from their oncologists, who they trust and see as experts in their care. The lack of integrated exercise professionals in oncology clinics and limited clinic time make it even harder to meet patient needs.
Providers often see exercise counseling as outside their main job or less important than other treatments. This view leads to fewer routine discussions about exercise. Improving education, building shared-care models, and adding exercise professionals to clinics could help bridge this gap. When providers encourage and support patients, it boosts motivation and helps survivors stay active.
Impact on Survivors
Missed Benefits
Many cancer survivors do not receive enough support for physical activity. They miss out on important health improvements that regular movement can provide. Survivors who remain inactive face higher risks of death from cancer and other causes. They often experience more anxiety, depression, and fatigue. Sleep quality tends to decline, and bone health suffers. Side effects such as joint pain and lymphedema can worsen without exercise.
Increased risk of death from cancer and other illnesses
Higher rates of anxiety, depression, and fatigue
Poor sleep and reduced bone strength
Worsening of joint pain and lymphedema
Prolonged sitting adds to these risks. Each extra hour spent sitting daily raises the chance of dying from any cause by 7%. Cancer-related deaths increase by 9%, and deaths from other causes rise by 5%. Survivors who exercise less than 150 minutes per week and sit more than eight hours daily have a 5.38% higher risk of death compared to those who meet activity guidelines. Most survivors do not reach recommended levels of exercise, which means they lose out on better survival rates and quality of life.
Survivors who lack exercise support often struggle with persistent symptoms like muscle wasting, heart problems, fatigue, and cognitive issues. These symptoms can cluster together, making daily life much harder. Regular exercise helps build muscle, improve heart health, and reduce inflammation, but many survivors do not get these benefits.
Access Inequities
Not all cancer survivors have the same chance to receive exercise support. Older adults, especially those over 65, often find it hard to stay active due to other health problems and loss of strength. Racial and ethnic minorities, including non-Hispanic Black, Hispanic, and Asian survivors, show lower rates of physical activity. Factors such as unsafe neighborhoods and limited access to parks or gyms make it harder for them to exercise.
Survivors with lower income, less education, or no insurance face more barriers to staying active.
Rural and remote survivors struggle with fewer exercise programs, long travel distances, and lack of tailored guidance.
Many survivors need childcare, flexible work schedules, and safe places to exercise, but these are not always available.
These differences lead to poorer health outcomes for underserved groups. Rural survivors often do physical tasks instead of structured exercise because of fatigue and geographic challenges. Digital solutions, such as mobile exercise apps, can help bridge the gap by offering personalized guidance and support. Social connections, like exercising with a partner or trainer, also boost motivation and help survivors stick with healthy habits.
Access inequities mean some survivors face higher symptom burdens, more fatigue, and increased mortality rates. Making exercise support more available and tailored can help reduce these disparities and improve outcomes for all survivors.
Improving Exercise Support
System Reforms
Healthcare organizations can improve access to exercise for cancer survivors by adopting system-level reforms. Programs like ACCESS show that building networks between clinics and community organizations helps survivors find exercise support. These networks connect survivors with Clinical Exercise Physiologists who screen and guide them to the right exercise programs. Specialized training for exercise professionals ensures that survivors receive safe and effective care. Creating both clinician and self-referral pathways allows more survivors to join programs that fit their needs.
System reforms also include embedding exercise programming into standard oncology care. This approach addresses common barriers such as limited resources and low awareness. Organizations that use real-world models see better recruitment, retention, and outcomes for survivors. Policy changes play a key role in making exercise support routine. Defining clear protocols for different cancer types and treatment stages helps payers understand the value of these programs. Expanding third-party payer coverage and aligning advocacy with national initiatives, like the Cancer Moonshot, increase access and sustainability.
System reforms create a foundation for lasting change. When organizations invest in training, partnerships, and policy updates, survivors benefit from consistent and high-quality exercise support.
Better Referrals
Optimizing referral pathways increases participation in exercise programs among cancer survivors. Structured referral systems help providers match survivors with the right level of support. The following table shows how triage levels guide referral decisions:
Triage Level | Criteria | Referral Pathway |
|---|---|---|
Level 1 | Patients meeting recommended exercise levels | Continue current exercise; no referral needed. |
Level 2 | Patients not meeting exercise levels, no medical supervision needed | Referral to local exercise services led by fitness professionals; choice based on patient preference and accessibility. |
Level 3 | Patients not meeting exercise levels, require medical supervision | Referral to clinical specialist physiotherapist for individualized assessment and supervised exercise programs. |
Referral success depends on survivor willingness and acceptance. Providers should explain the purpose and benefits of exercise referrals to encourage participation. Early referrals, ideally within two weeks of assessment, prevent deconditioning and improve outcomes. Interdisciplinary teams, including oncologists and physiotherapists, coordinate referrals and monitor progress. Integrated Care Coordinators make the process easier and more acceptable for survivors.
Referral pathways must adapt to local healthcare infrastructure and resources. Community programs offer safe exercise options for survivors who do not need medical supervision. Continuous communication among providers ensures that referrals remain appropriate as survivor needs change.
Clear and tailored referral pathways help more survivors access exercise support, improving their health and quality of life.
Provider Training
Provider training is essential for integrating exercise support into standard cancer care. Multidisciplinary approaches combine exercise training with support for mental health, nutrition, and work reintegration. These programs address complex survivor needs more effectively than exercise alone. Studies show that supervised, group-based exercise programs within multidisciplinary settings improve aerobic capacity, muscle strength, and quality of life.
Continuous assessment and collaboration among oncology, rehabilitation, nursing, and support services allow care plans to evolve with survivor needs. Telehealth expands access to personalized exercise support, especially for survivors in remote areas. Real-time monitoring and adjustment of exercise regimens help survivors stay engaged and safe. Platforms like Vitala Health deliver tailored exercise prescriptions and track outcomes, supporting scalability and sustainability.
Provider training should cover behavioral change techniques, telehealth delivery, and collaboration with exercise professionals. Organizations must invest in robust technology and training for both providers and survivors. Policy changes, such as expanding payer coverage and clarifying provider roles, support the integration of exercise programs into routine care.
Provider training and multidisciplinary collaboration ensure that survivors receive personalized, effective exercise support throughout their cancer journey.
Significant gaps remain between research and real-world care. Many survivors do not receive consistent exercise support due to system inefficiencies, uneven professional training, and limited resources. Providers often lack confidence and awareness of referral pathways. Organizations can drive change by updating policies, investing in workforce training, and integrating exercise into clinical routines. By addressing these barriers, healthcare teams can help more survivors benefit from safe, effective physical activity.
FAQ
What types of exercise are safe for cancer survivors?
Most survivors can safely do aerobic, resistance, and flexibility exercises. A healthcare provider or exercise specialist should help choose the right activities. They will consider the survivor’s health, treatment history, and any side effects.
How soon after treatment can a survivor start exercising?
Survivors can often begin gentle activity soon after treatment ends. A doctor or physical therapist should guide the timing and intensity. Early movement helps reduce fatigue and improves recovery.
Who provides exercise support for cancer survivors?
Certified exercise physiologists, physical therapists, and some oncology nurses offer exercise support. They work with oncology teams to create safe, personalized plans. Survivors should ask their care team for referrals.
What if a survivor feels too tired to exercise?
Even small amounts of movement help. Short walks or light stretching can boost energy and mood. Survivors should listen to their bodies and increase activity slowly.
Are there programs for survivors in rural or remote areas?
Many programs now offer telehealth or online options. Survivors in rural areas can join virtual classes or use mobile apps. Local community centers may also provide group activities.
See Also
Recognizing The Signs And Causes Of Esophageal Cancer
A Comprehensive Guide To Symptoms And Treatment Of Duodenal Cancer
Exploring Various Cancer Types Associated With AIDS
An Introduction To The Rare Cancer Called Angiosarcoma
Insights Into Bone Cancers Malignant Fibrous Histiocytoma And Osteosarcoma

