What Are Extragonadal Germ Cell Tumors and How Do They Develop

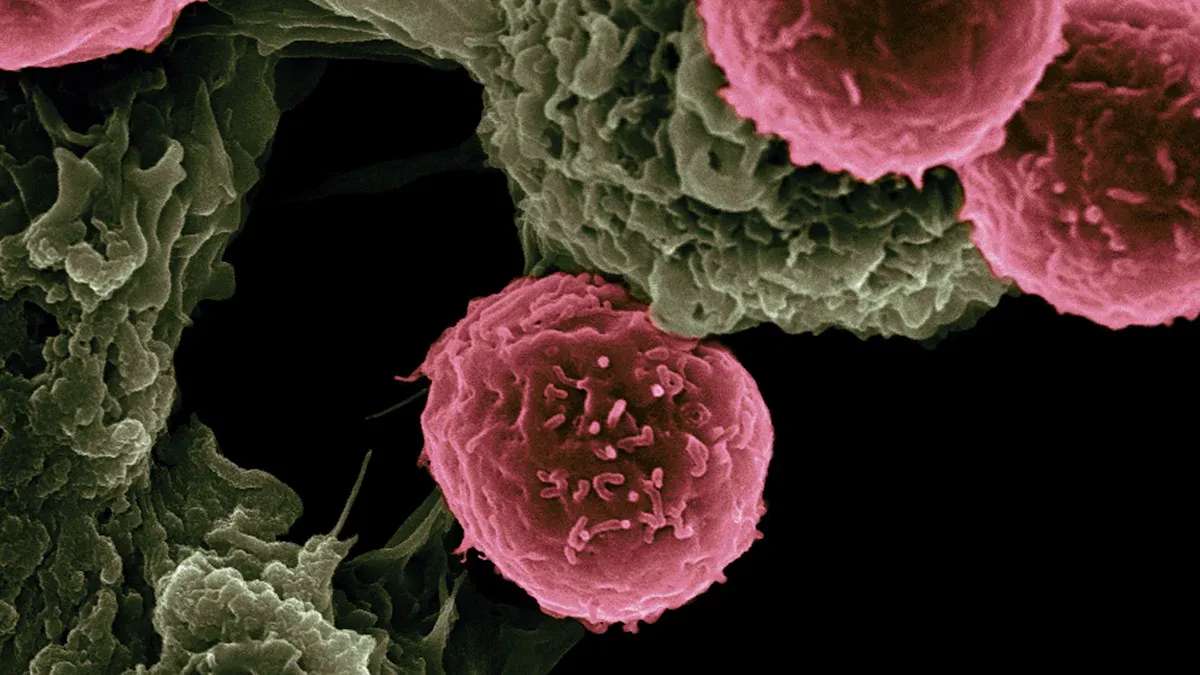
An extragonadal germ cell tumor is a rare type of cancer that forms from germ cells located outside the gonads, such as the testes or ovaries. These tumors account for about 5% of all germ cell tumors and can develop in areas like the mediastinum, retroperitoneum, or brain. Scientists believe they arise due to abnormal germ cell migration during early development or genetic mutations. For instance, mutations in the TP53 gene are often linked to mediastinal tumors, especially in older children, and can make these tumors resistant to chemotherapy.
Key Takeaways
Extragonadal germ cell tumors are rare cancers. They grow from germ cells outside the gonads, often in the chest or belly.
Symptoms may include pain, swelling, or trouble breathing. Finding them early with scans and blood tests helps treatment work better.
Treatment usually includes surgery and chemotherapy. Finding the cancer early can save lives and improve health.
Risks include being male, over 20 years old, or having genetic issues like Klinefelter syndrome. Knowing these risks can help find the cancer sooner.
After treatment, regular check-ups are important. They help watch for cancer returning and handle long-term health problems.
What Are Extragonadal Germ Cell Tumors?
Definition and Characteristics
An extragonadal germ cell tumor develops from germ cells located outside the gonads, such as the testes or ovaries. These tumors are rare and often found in midline areas of the body, including the mediastinum and retroperitoneum. They can be benign, like teratomas, or malignant, such as seminomatous and non-seminomatous tumors. Most cases occur in young males, and the tumors may vary in size and behavior.
Key characteristics of extragonadal germ cell tumors include:
They arise in locations other than the gonads.
They can be either benign or malignant.
They are more common in young males.
They often appear in midline regions of the body.
Types of Extragonadal Germ Cell Tumors
Extragonadal germ cell tumors are classified into several types based on their histology. These include seminomatous, non-seminomatous, and mixed germ cell tumors. Below is a table summarizing the primary types and their subtypes:
Type of Tumor | Subtypes |
|---|---|
Seminomatous Tumors | Classical seminoma |
Non-Seminomatous Tumors | Embryonal carcinoma, teratoma (mature/immature), yolk sac carcinoma, choriocarcinoma |
Mixed Germ Cell Tumors | Composed of two or more histotypes |
Mediastinal Tumors
Mediastinal tumors are the most common extragonadal germ cell tumors. They develop in the chest cavity, often near the heart. These tumors may cause symptoms like chest pain, coughing, or difficulty breathing.
Retroperitoneal Tumors
Retroperitoneal tumors form in the abdominal cavity, behind the peritoneum. They can grow large before causing noticeable symptoms, such as abdominal pain or swelling.
Other Rare Locations
In rare cases, extragonadal germ cell tumors may arise in the brain, neck, or other unusual locations. These tumors often present unique challenges in diagnosis and treatment.
Differences Between Extragonadal and Gonadal Germ Cell Tumors
Extragonadal germ cell tumors differ from gonadal tumors in several ways:
They often present as larger masses at diagnosis.
They may lead to a broader range of symptoms due to their location.
They exhibit unique molecular and pathological features.
They are considered a special subgroup with a poorer prognosis.
Malignant extragonadal tumors, especially non-seminomas, tend to grow and spread more quickly.
These differences highlight the importance of understanding the unique nature of extragonadal germ cell tumors for accurate diagnosis and effective treatment.
How Do Extragonadal Germ Cell Tumors Develop?
Causes of Tumor Development
Genetic Mutations
Genetic mutations play a significant role in the development of extragonadal germ cell tumors. For example, mutations in the ARF gene disrupt the interaction between p53 and mdm2, leading to the accumulation of mdm2 and impaired p53 function. This mutation is found in 71% of intracranial germ cell tumors (ICGCTs) and is common in 90% of seminomatous and 55% of non-seminomatous ICGCTs. These findings highlight how genetic changes can drive tumor formation.
Abnormal Germ Cell Migration
During embryonic development, germ cells migrate to the gonads along the body’s midline. Sometimes, these cells fail to reach their destination and become "misplaced." This abnormal migration can lead to the formation of tumors in areas like the mediastinum or retroperitoneum. These misplaced cells may undergo transformations that result in tumor growth.
Risk Factors
Age and Gender
Your age and gender significantly influence the likelihood of developing an extragonadal germ cell tumor. Males, especially those aged 20 or older, face a much higher risk. In older children and adolescents, the incidence of malignant tumors is 11.4 per million in males compared to just 1 per million in females. This trend continues into adulthood, where over 90% of malignant cases occur in males.
Family History
Certain inherited conditions, such as Klinefelter syndrome, increase the risk of developing these tumors. This syndrome, characterized by an extra X chromosome (47XXY), is particularly associated with mediastinal non-seminomatous germ cell tumors. A family history of similar conditions may also elevate your risk.
Risk Factor | Description |
|---|---|
Associated with mediastinal non-seminomatous germ cell tumors, located on the midline from the pineal gland to the coccyx. |
Theories on Tumorigenesis
Misplaced Germ Cells
One theory suggests that extragonadal germ cell tumors arise from primordial germ cells that become arrested during their migration to the gonads. These cells, instead of reaching the genital ridge, remain in other parts of the body, such as the chest or abdomen. Over time, these misplaced cells may transform into tumors.
Environmental and Hormonal Factors
Environmental exposures and hormonal imbalances may also contribute to tumor development. Factors like radiation, toxins, or abnormal hormone levels during critical periods of development could influence the transformation of germ cells into tumors. While research continues, these factors are believed to interact with genetic predispositions to increase the risk.
Symptoms and Diagnosis of Extragonadal Germ Cell Tumors
Common Symptoms
Pain or Swelling
Pain or swelling often occurs near the tumor site. For example, retroperitoneal tumors may cause abdominal discomfort, while mediastinal tumors can lead to chest pain. These symptoms usually worsen as the tumor grows, pressing against nearby structures.
Respiratory Symptoms
If the tumor develops in the mediastinum, you might experience breathing difficulties. Symptoms like coughing, shortness of breath (dyspnea), or even superior vena cava syndrome can arise. These issues occur because the tumor compresses airways or blood vessels in the chest.
Other Nonspecific Symptoms
Some symptoms are less specific but still important to recognize. These include fatigue, weight loss, fever, or changes in bowel habits. In rare cases, tumors in the brain may cause headaches, vision problems, or difficulty walking. Below is a table summarizing common symptoms and their prevalence:
Symptom | Percentage |
|---|---|
Chest pain | |
Dyspnea | 29% |
Cough | 22% |
Weight loss | 19% |
Superior vena cava syndrome | 12% |
Nausea | 6% |
Fever | 6% |
Diagnostic Methods
Imaging Techniques
Doctors use imaging to locate and assess the tumor. A chest X-ray can reveal an enlarged mediastinum or anterior mass. CT scans and MRIs provide detailed images of the tumor and surrounding tissues. For example, they can identify brain tumors like pineal seminomas. PET scans are also helpful for detecting larger tumors, though they may miss smaller ones or nonseminomatous germ cell tumors.
Imaging Technique | Description |
|---|---|
Chest x-ray | Shows enlargement of the mediastinum and the anterior location of the mass. |
CT scan/MRI | Identifies discrete masses in the brain, such as pineal seminoma, and can indicate obstructive hydrocephalus. |
PET scan | More sensitive than CT for detecting larger masses but may miss smaller tumors and is inconsistent for nonseminomatous germ cell tumors. |
Tumor Markers
Tumor markers in your blood can help confirm the diagnosis. Alpha-fetoprotein (AFP) levels rise in yolk sac tumors and embryonal carcinoma. Beta-hCG is elevated in nonseminomatous tumors, while lactate dehydrogenase (LDH) correlates with tumor size. These markers guide doctors in identifying the tumor type.
Tumor Marker | Relevance |
|---|---|
Alpha Fetoprotein (AFP) | Elevated in yolk-sac tumors and embryonal carcinoma; not produced by pure seminomas or choriocarcinomas. |
Beta-hCG | Elevated in extragonadal nonseminomatous germ cell tumors; produced by choriocarcinoma, embryonal carcinoma, and some seminomas. |
Lactate Dehydrogenase (LDH) | Nonspecific marker; correlates with tumor burden. |
Biopsy
A biopsy provides the most definitive diagnosis. During this procedure, doctors remove a small tissue sample from the tumor. Pathologists then examine the sample under a microscope to determine the tumor's type and malignancy. This step is crucial for planning treatment.
Diagnosing an extragonadal germ cell tumor can be challenging due to its rarity and the need to rule out gonadal origins. Misdiagnosis is common, especially in young individuals with midline masses. Early and accurate diagnosis improves treatment outcomes.
Treatment Options for Extragonadal Germ Cell Tumors
Surgical Approaches
Indications for Surgery
Surgery plays a critical role in treating extragonadal germ cell tumors, especially when chemotherapy alone cannot eliminate the tumor. You may need surgery if the tumor is a teratoma, as these are often resistant to chemotherapy. For nonseminomatous tumors, surgery is essential for removing residual masses after chemotherapy. In cases of mediastinal or retroperitoneal tumors, surgery is often the first step to ensure complete tumor removal.
Types of Procedures
The type of surgical procedure depends on the tumor's location. Below is a table summarizing common approaches:
Tumor Location | Surgical Approach |
|---|---|
Teratomas | Surgery is the primary treatment modality. |
Nonseminomatous Germ Cell Tumors | Surgery is used as primary or secondary treatment, especially for residual masses after chemotherapy. |
Mediastinal Germ Cell Tumors | Midline sternotomy is common; thymectomy and partial pericardial resection are often required. |
Retroperitoneal Germ Cell Tumors | Midline, transverse, or oblique transperitoneal approaches are utilized. |
Pineal Germ Cell Tumors | En bloc resection via the supracerebellar infratentorial approach is performed. |
Surgical intervention not only removes the tumor but also improves survival rates when combined with chemotherapy.
Chemotherapy
Common Regimens
Chemotherapy is a cornerstone of treatment for extragonadal germ cell tumors. Doctors often use specific regimens based on the tumor type and stage. Below is a table of commonly used regimens:
Regimen | Components | Notes |
|---|---|---|
BEP | Bleomycin, Etoposide, Cisplatin | Standard therapy |
VIP | Etoposide, Ifosfamide, Cisplatin | Salvage therapy |
BOP | Bleomycin, Vincristine, Cisplatin | Initial regimen |
CISCA | Cisplatin, Cyclophosphamide, Doxorubicin | Follow-up regimen |
POMB | Cisplatin, Vincristine, Methotrexate, Bleomycin | Subsequent regimen |
BEP is the most widely used regimen due to its effectiveness and high survival rates.
Managing Side Effects
Chemotherapy can cause side effects, including fatigue, nausea, and an increased risk of infections. You may also experience thromboembolic events, which occur in about 8.4% of patients. To manage these effects, doctors may prescribe medications to reduce nausea or adjust dosages to minimize complications. Staying hydrated and maintaining a balanced diet can also help your body recover during treatment.
Follow-Up Care
Monitoring for Recurrence
After treatment, regular follow-up care is essential to monitor for recurrence. Your doctor may recommend clinical exams, imaging tests like CT or MRI scans, and blood tests to check tumor markers. Ultrasounds of the testicles may also be part of the follow-up plan. These steps help detect any signs of the tumor returning early, improving your chances of successful treatment.
Long-Term Health Considerations
Survivors of extragonadal germ cell tumors face unique long-term health challenges. Below is a table summarizing potential complications:
Complication Type | Description |
|---|---|
Cardiovascular Issues | Increased risk of coronary artery disease due to treatment. |
Cognitive Effects | Potential intellectual and endocrine function issues, especially from cranial radiation. |
Risk of Second Malignancies | Elevated risk of developing additional cancers later in life. |
Hormonal Deficiencies | Hormonal imbalances requiring ongoing management. |
Personality Changes | Notable changes in personality may occur as a result of treatment. |
Regular monitoring and participation in survivorship programs can help you manage these risks effectively.
Extragonadal germ cell tumors are rare cancers that develop from misplaced germ cells outside the gonads. These tumors often arise due to factors like Klinefelter syndrome or abnormal germ cell migration during embryogenesis. Symptoms vary based on tumor location but may include pain, swelling, or respiratory issues. Early diagnosis through imaging, tumor markers, and biopsy is crucial for effective treatment.
Treatment options include surgery, chemotherapy, and emerging therapies like immunotherapy. Surgery often serves as the first step, while chemotherapy plays a vital role in managing malignant cases. Advances in targeted therapies and minimally invasive techniques continue to improve outcomes. Early detection and prompt treatment significantly enhance survival rates and quality of life.
FAQ
What makes extragonadal germ cell tumors different from other tumors?
Extragonadal germ cell tumors develop from germ cells outside the gonads, unlike most tumors that originate in specific organs. These tumors often appear in midline areas like the chest or abdomen. Their unique origin and location make them distinct in diagnosis and treatment.
Can extragonadal germ cell tumors spread to other parts of the body?
Yes, malignant extragonadal germ cell tumors can spread (metastasize) to other areas, including the lungs, liver, or brain. Early detection and treatment reduce the risk of metastasis and improve outcomes.
Are extragonadal germ cell tumors curable?
Many extragonadal germ cell tumors are treatable, especially when diagnosed early. Treatment options like surgery and chemotherapy offer high success rates. Your prognosis depends on factors like tumor type, location, and stage.
Who is most at risk for developing these tumors?
Young males, particularly those aged 20 or older, face the highest risk. Certain genetic conditions, like Klinefelter syndrome, also increase your likelihood of developing these tumors.
How can you detect extragonadal germ cell tumors early?
Pay attention to symptoms like pain, swelling, or breathing difficulties. Regular check-ups and imaging tests help detect tumors early. If you have risk factors, discuss screening options with your doctor.
Tip: Early diagnosis improves treatment success. Don’t ignore persistent or unusual symptoms.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Understanding Embryonal Carcinoma: Essential Information You Should Know
Choriocarcinoma Overview: Definition and Treatment Options Available
Exploring Astrocytoma: Types and Their Distinct Characteristics
Anaplastic Large Cell Lymphoma: Definition and Treatment Approaches

