How Genetic Testing Drives Personalized Cancer Treatment
Genetic testing has transformed how you approach cancer treatment, particularly in the context of 'Personalized Cancer Treatment: The Role of Genetic Testing.' By identifying unique mutations in tumors, it enables therapies tailored to your specific needs. This approach improves survival rates and reduces side effects. For example, a study of over 78,000 patients found nearly 800 genetic changes that directly impacted outcomes. Adjusting treatments based on these insights has saved lives. In one case, genetic testing helped reduce a chemotherapy dose by 50%, preventing severe complications. Understanding the genetic profile of cancer cells empowers you to receive more precise and effective care, highlighting the importance of personalized cancer treatment.
Key Takeaways
Genetic testing finds special changes in tumors. This helps create cancer treatments that work better and cause fewer side effects.
Germline testing shows inherited genetic risks. Somatic testing finds changes in tumor cells to guide specific treatments.
Useful mutations found by genetic testing help doctors choose the best treatments. This avoids extra therapies and reduces side effects.
Liquid biopsies are simple tests that check tumor changes without surgery. They help doctors adjust treatments as cancer changes.
New genetic testing tools, like next-generation sequencing, make cancer care quicker and easier for more people.
Personalized Cancer Treatment: The Role of Genetic Testing
What Is Genetic Testing in Cancer Care?
Definition and purpose of genetic testing.
Genetic testing in cancer care involves analyzing your DNA to identify mutations that may contribute to cancer development. These tests help uncover whether the mutations are inherited or acquired, providing critical insights into your cancer's behavior. By understanding these genetic changes, doctors can create a treatment plan tailored to your specific needs. This approach ensures that therapies target the root cause of your cancer, improving outcomes and reducing unnecessary treatments.
Genetic testing serves multiple purposes. It can predict your risk of developing cancer, confirm a diagnosis, or guide treatment decisions. For example, predictive genetic testing identifies inherited mutations, such as BRCA1 and BRCA2, which increase the risk of breast and ovarian cancers. Testing for diagnosed patients helps determine if their cancer is linked to inherited mutations, which can guide family members in assessing their own risks.
How genetic testing works in cancer diagnosis and treatment.
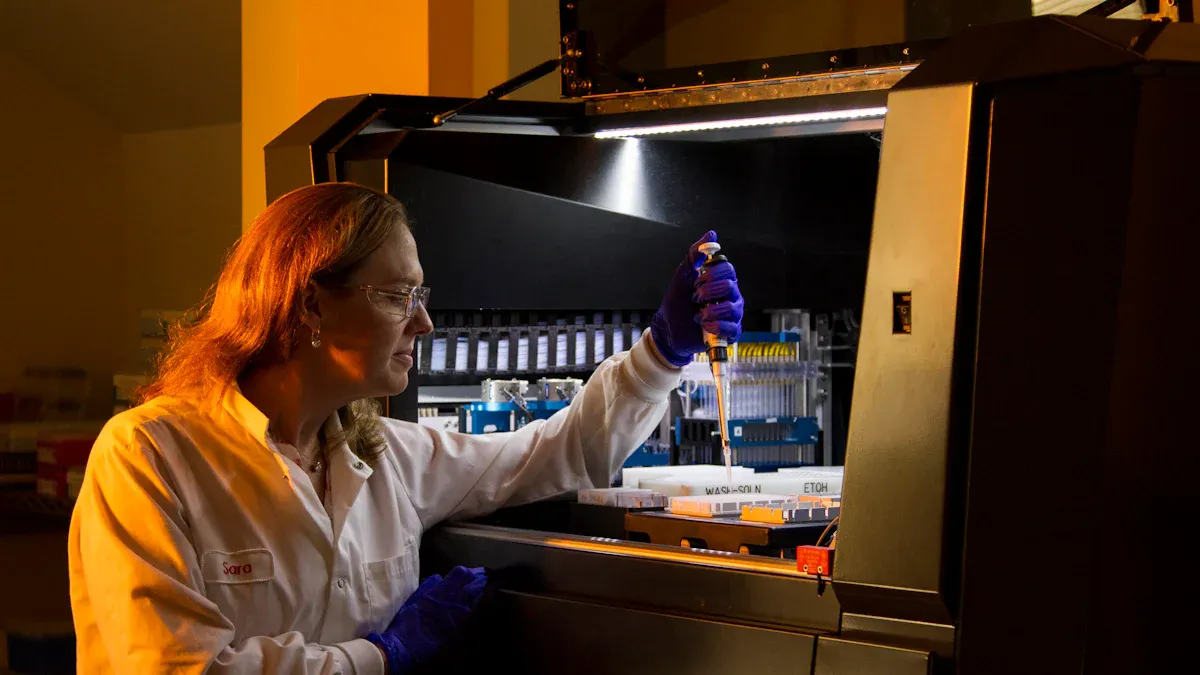
The process begins with a sample of your blood, saliva, or tumor tissue. Scientists analyze this sample to detect genetic mutations. Advanced techniques like next-generation sequencing (NGS) allow for comprehensive profiling of your tumor's genetic makeup. This technology identifies actionable mutations, which are changes that can be targeted with specific therapies. For instance, mutations in the EGFR gene in lung cancer patients can guide the use of EGFR inhibitors, a type of targeted therapy.
Genetic testing also evaluates the clinical utility of these findings. This means determining whether the test results will improve your treatment outcomes. For example, identifying mutations in DNA repair pathways can indicate whether immunotherapy might be effective for you. By integrating these insights, genetic testing ensures that your treatment is as precise and effective as possible.
Types of Genetic Testing
Germline testing: Identifying inherited genetic risks.
Germline testing focuses on the genetic mutations you inherit from your parents. These mutations exist in every cell of your body and can increase your risk of developing certain cancers. For example, mutations in the BRCA1 and BRCA2 genes are strongly linked to breast and ovarian cancers. Germline testing is particularly useful if you have a family history of cancer. It helps you understand your risk and take preventive measures, such as increased screening or preventive surgery.
Somatic testing: Detecting mutations in tumor cells.
Somatic testing examines the genetic changes that occur in your tumor cells but not in the rest of your body. These mutations develop over time due to factors like environmental exposure or aging. Somatic testing identifies mutations that drive cancer growth, such as KRAS or HER2 mutations. These findings guide the use of targeted therapies, ensuring that your treatment directly addresses the unique characteristics of your tumor.
Why Genetic Testing Is Essential
Understanding cancer biology through genetic insights.
Genetic testing provides a deeper understanding of how cancer develops and progresses. By analyzing your tumor's genetic profile, doctors can identify the pathways that fuel its growth. For example, mutations in the PI3K pathway can influence how your cancer responds to treatment. This knowledge allows for more informed decisions about your care.
Identifying actionable mutations for targeted therapies.
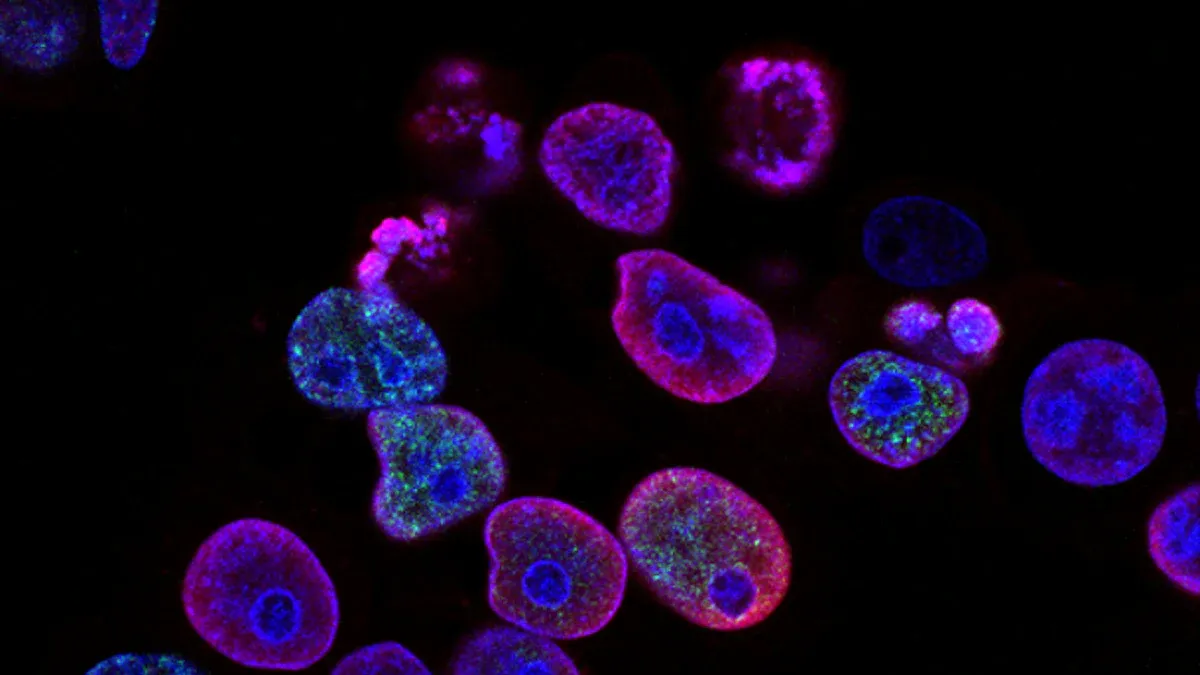
Actionable mutations are genetic changes that can be targeted with specific treatments. For instance, identifying a HER2 mutation in breast cancer can lead to the use of HER2 inhibitors, which block the protein's activity and slow tumor growth. Similarly, mutations in immune-related pathways can predict your response to immunotherapy. By pinpointing these mutations, genetic testing ensures that your treatment is both effective and personalized.
How Genetic Testing Guides Cancer Treatment
Targeted Therapy
Identifying specific genetic targets for treatment.
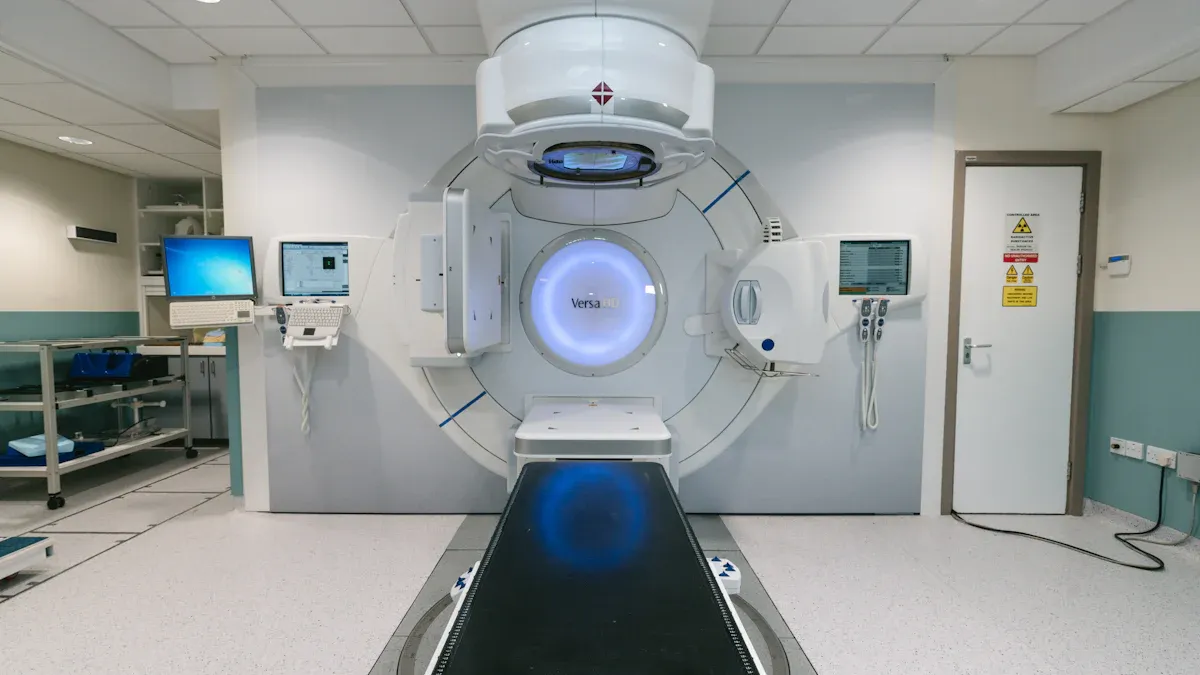
Genetic testing allows you to uncover specific mutations in your cancer cells, enabling doctors to target these changes directly. For example, mutations in the HER2 gene often drive aggressive breast cancer growth. By identifying this mutation, doctors can prescribe HER2 inhibitors, which block the protein's activity and slow tumor progression. Similarly, EGFR mutations in lung cancer can guide the use of EGFR inhibitors, offering a more precise treatment approach.
This targeted strategy reduces harm to healthy tissues and increases the likelihood of success. A study analyzing over 78,000 cancer patients identified nearly 800 genetic changes that influenced survival outcomes. These findings highlight how genetic testing personalizes treatment, improving your chances of recovery.
Examples of targeted therapies like HER2 and EGFR inhibitors.
Targeted therapies have revolutionized cancer care. HER2 inhibitors, such as trastuzumab, specifically block the HER2 protein in breast cancer, reducing tumor growth. EGFR inhibitors, like erlotinib, target EGFR mutations in lung cancer, improving survival rates. These therapies demonstrate how genetic testing transforms treatment by focusing on the unique characteristics of your cancer.
Predicting Treatment Response
Using genetic data to predict drug effectiveness.
Genetic testing helps predict how your tumor will respond to different treatments. For instance, mutations in DNA repair genes like BRCA1 can indicate whether PARP inhibitors will work for you. This predictive ability ensures that you receive therapies with the highest chance of success, avoiding unnecessary treatments.
Avoiding ineffective treatments and minimizing side effects.
By identifying mutations that influence drug response, genetic testing spares you from ineffective therapies. For example, if your tumor lacks a specific mutation, doctors can avoid prescribing drugs that target it. This approach minimizes side effects and ensures a more comfortable treatment experience.
Optimizing Immunotherapy
Role of genetic markers in immunotherapy success.
Immunotherapy harnesses your immune system to fight cancer, but not all patients benefit equally. Genetic markers like PD-L1 expression or microsatellite instability (MSI) help determine if immunotherapy will work for you. These markers guide doctors in selecting the most effective treatment options.
Examples of biomarkers like PD-L1 and MSI.
PD-L1 is a protein that some tumors use to evade your immune system. High levels of PD-L1 suggest that immunotherapy drugs, such as checkpoint inhibitors, may be effective. MSI, another biomarker, indicates defects in DNA repair mechanisms, making tumors more responsive to immunotherapy. These examples show how genetic testing optimizes your treatment plan.
A groundbreaking study revealed how specific genetic mutations influence cancer treatment outcomes, helping doctors tailor treatments more effectively. The research analyzed data for over 78,000 cancer patients and identified nearly 800 genetic changes impacting survival outcomes, highlighting the crucial role of genetic profiling in personalizing cancer care.
Monitoring and Adapting Treatment
Liquid biopsies for tracking genetic changes
Liquid biopsies offer a non-invasive way to monitor your cancer's genetic profile. Instead of relying on traditional tissue biopsies, this method uses a simple blood sample to detect genetic material shed by tumor cells. These include circulating tumor DNA (ctDNA) and other biomarkers. Liquid biopsies allow doctors to track changes in your tumor's genetic makeup over time.
This approach provides several advantages. It reduces the need for painful procedures and helps detect mutations that may not appear in a single tissue sample. For example, if your tumor develops resistance to a targeted therapy, liquid biopsies can identify new mutations driving this resistance. This information helps your doctor adjust your treatment plan quickly, ensuring it remains effective.
Tip: Liquid biopsies are especially useful for cancers that are difficult to access through traditional biopsies, such as lung or brain tumors.
Adjusting treatment plans based on tumor evolution
Cancer evolves as it grows, often developing new mutations that make it resistant to current treatments. Genetic testing through liquid biopsies helps you stay ahead of these changes. By identifying new mutations, your doctor can modify your treatment plan to target the evolving tumor.
For instance, if your tumor develops a mutation that makes it resistant to one drug, genetic testing can guide the switch to another therapy. This adaptive approach ensures your treatment remains effective even as your cancer changes.
Doctors also use this information to monitor how well your treatment is working. If genetic markers show that your tumor is shrinking, your current therapy is likely effective. If not, adjustments can be made to improve outcomes. This dynamic process ensures that your care evolves alongside your cancer, giving you the best chance for success.
Real-World Impact of Genetic Testing
Case Studies
Lung cancer patient benefiting from EGFR-targeted therapy
Genetic testing has transformed lung cancer treatment by identifying mutations like EGFR. For example, a patient with advanced lung cancer underwent genetic testing, revealing an EGFR mutation. This discovery allowed doctors to prescribe EGFR inhibitors, such as erlotinib, which specifically target the mutation. The patient experienced significant tumor shrinkage and improved quality of life. Without genetic testing, this targeted therapy would not have been possible, and the patient might have endured less effective treatments.
Melanoma patient responding to immunotherapy guided by genetic testing
In another case, a melanoma patient benefited from immunotherapy thanks to genetic testing. The test identified high levels of PD-L1 expression, a biomarker indicating potential success with checkpoint inhibitors. Based on this insight, doctors recommended pembrolizumab, an immunotherapy drug. The patient’s immune system responded effectively, leading to tumor reduction and prolonged survival. This case highlights how genetic testing personalizes treatment, ensuring you receive therapies that work best for your cancer.
Success Stories
Improved survival rates with personalized approaches
A large study analyzed data from over 78,000 cancer patients across 20 types. Researchers identified nearly 800 genetic changes that directly impacted survival outcomes. These findings enabled doctors to select effective therapies while avoiding ineffective ones. The table below summarizes the study's impact:
Study Overview | Findings | Impact on Treatment |
|---|---|---|
Analyzed data from over 78,000 cancer patients across 20 types | Identified nearly 800 genetic changes affecting survival outcomes | Enabled selection of effective therapies, reducing ineffective treatments |
Reduced side effects through targeted treatments
Personalized cancer treatment reduces side effects by tailoring therapies to your genetic profile. For instance:
A patient named John had his chemotherapy dose reduced by 50% due to genetic testing, preventing severe complications.
Doctors monitored and adjusted his treatment plan based on his tolerance, ensuring adaptability.
Although John experienced some side effects, the medical team managed them effectively, showcasing the benefits of personalized care.
These examples demonstrate how genetic testing improves outcomes and enhances your quality of life. Personalized Cancer Treatment: The Role of Genetic Testing continues to revolutionize cancer care by making therapies safer and more effective.
Advancements in Genetic Testing Technologies
Next-Generation Sequencing (NGS)
Comprehensive genetic profiling with NGS
Next-generation sequencing (NGS) has revolutionized how you can understand cancer at a genetic level. This technology allows for comprehensive profiling of your tumor's genetic makeup, identifying mutations that drive cancer growth. By analyzing multiple genes simultaneously, NGS provides a detailed map of your cancer's unique characteristics.
A large-scale study involving 78,287 patients across 20 cancer types identified 95 genes significantly associated with survival. It also uncovered 776 gene-treatment interactions that directly impacted outcomes. These findings highlight the power of NGS in uncovering actionable genetic changes.
Evidence Type | Description |
|---|---|
Large-Scale Analysis | A study involving 78,287 patients across 20 cancer types, identifying 95 genes linked to survival. |
Gene-Treatment Interactions | 776 gene-treatment interactions were found to influence survival outcomes. |
Real-World Data Utilization | Emphasizes the importance of real-world data from electronic health records. |
Faster and more affordable testing methods
NGS has become faster and more cost-effective over time. Early sequencing methods took years to complete and cost millions of dollars. Today, NGS can deliver results in days at a fraction of the cost. This efficiency makes genetic testing more accessible, allowing you to benefit from personalized cancer care without long delays or high expenses.
Emerging Technologies
CRISPR and its potential in cancer research
CRISPR technology offers exciting possibilities for cancer research. It allows scientists to edit genes with precision, enabling them to study how specific mutations contribute to cancer. This tool could lead to breakthroughs in developing therapies that target genetic changes directly. For example, researchers have used CRISPR to validate the role of genes like TP53 and CDKN2A in treatment outcomes, paving the way for more effective treatments.
AI and machine learning in genetic data analysis
Artificial intelligence (AI) and machine learning are transforming how you analyze genetic data. These technologies can process vast amounts of information quickly, identifying patterns that might be missed by traditional methods. A machine learning tool recently predicted immunotherapy responses in advanced lung cancer patients, helping doctors choose the most effective treatments.
Findings | Details |
|---|---|
Precision Medicine | Highlights the shift to personalized approaches based on genetic makeup. |
Key Genes | Identified critical roles of genes like TP53, CDKN2A, and CDKN2B. |
Machine Learning Tool | Developed to predict responses to immunotherapy in advanced lung cancer. |
Future Potential
Expanding access to genetic testing for all patients
Expanding access to genetic testing remains a critical goal. Many patients still lack access to these advanced technologies due to cost or availability. Efforts to make testing more affordable and widely available could ensure that everyone benefits from personalized cancer care.
Integrating genetic data into routine cancer care
The integration of genetic data into standard cancer treatment is on the horizon. Researchers suggest that large-scale genomic studies could help doctors use genetic information to guide treatment decisions. For example, a study analyzing 78,287 patients across 20 cancer types demonstrated how clinico-genomics data could identify biomarkers predicting treatment responses. This approach could transform cancer care, making it more precise and effective for you.
Note: As genetic testing becomes more accessible, it has the potential to become a routine part of cancer care, ensuring that every patient receives the most effective treatment.
Genetic testing has revolutionized cancer care by enabling personalized treatment strategies tailored to your unique genetic profile. It identifies actionable mutations, improving therapies and reducing side effects. For example, studies show that patients with DPYD genetic variants who received adjusted chemotherapy doses experienced fewer toxicities.
Application | Description |
|---|---|
Personalized Medicine | Tailored therapies based on individual genetic profiles improve outcomes. |
Tumor Classification | Accurate tumor classification identifies new subtypes for better care. |
Multigene Testing | Simultaneous assessment of multiple genes enhances data interpretation. |
Advancements like complete cancer genome sequencing promise a future where cancer care becomes even more precise and accessible. Genetic testing ensures you receive the most effective treatment possible.
FAQ
1. What is the difference between germline and somatic genetic testing?
Germline testing identifies inherited mutations present in all your cells. Somatic testing detects mutations specific to your tumor cells. Germline testing helps assess cancer risk, while somatic testing guides treatment by identifying actionable mutations in your tumor.
2. How does genetic testing improve cancer treatment?
Genetic testing tailors your treatment by identifying mutations that drive your cancer. This allows doctors to select therapies targeting these mutations, improving effectiveness and reducing side effects. It also helps predict how well you might respond to specific treatments.
3. Is genetic testing painful or invasive?
No, genetic testing is not painful. It typically involves a blood, saliva, or tissue sample. Liquid biopsies, which use a simple blood draw, offer a non-invasive option for tracking genetic changes in your tumor over time.
4. Can genetic testing benefit all cancer patients?
Yes, genetic testing benefits most cancer patients. It identifies mutations that guide treatment decisions. However, its usefulness depends on your cancer type and stage. Discuss with your doctor to determine if it’s right for you.
5. How long does it take to get genetic testing results?
The time varies based on the test type. Next-generation sequencing (NGS) often provides results within days. Simpler tests may take less time. Your doctor will inform you about the expected timeline for your specific test.
Tip: Ask your healthcare provider about the testing process and how it fits into your treatment plan.
See Also
An In-Depth Overview of Various Cancer Types
Key Characteristics of Glioblastoma You Need to Know
Recognizing Symptoms and Treatments for Duodenal Cancer
Understanding Leydig Cell Tumors and Their Causes
Essential Information About Carcinoid Tumors You Should Know

