How AI is Transforming Cancer Detection and Treatment in 2025
AI has become a powerful ally in the fight against cancer. You now have access to tools that can detect tumors with remarkable accuracy. For instance, AI algorithms identify cancers in scans with 94% precision, outperforming professional radiologists. In mammography, AI-assisted screening detects 29% more breast cancers, including early-stage tumors, compared to traditional methods. These advancements reduce diagnostic errors, which affect over 12 million Americans annually. With AI analyzing complex datasets, you benefit from personalized treatments and improved survival predictions. Harnessing AI in cancer detection and treatment offers a future where outcomes improve and hope grows.
Key Takeaways
AI tools find tumors with 94% accuracy, helping doctors catch cancer early and make fewer mistakes.
Predictive tools spot high-risk patients, so doctors can act sooner and improve treatments.
AI customizes cancer care by studying genes and health records, making treatments fit each person better.
AI speeds up making new drugs, cutting costs and time, so patients get new medicines faster.
Fixing biases and keeping data private are key for fair and safe AI use in cancer care.
Harnessing AI in Early Cancer Detection

AI-powered diagnostic tools and imaging advancements
AI-powered diagnostic tools have revolutionized how you detect cancer. These tools analyze medical images with remarkable precision, identifying abnormalities that might go unnoticed by the human eye. For example, AI enhances mammogram reviews, increasing sensitivity and detecting more cancers. It also reduces false positives, ensuring you receive accurate diagnoses. Consistent assessments of breast density, a critical factor in early detection, further highlight AI's role in improving imaging accuracy.
Clinical studies back these advancements. In the MASAI study, AI detected 6.7 cancers per 1,000 screenings compared to 5.7 by traditional methods. It also improved the positive predictive value (PPV) of biopsies, achieving 64.5% compared to 59.2% in the control group. These results demonstrate how AI-powered imaging tools enhance early cancer detection, giving you a better chance at timely treatment.
Predictive analytics for identifying high-risk patients
Predictive analytics uses AI to identify patients at high risk of developing cancer. By analyzing patterns in electronic health records (EHRs), AI models predict potential risks and enable earlier interventions. These models outperform traditional statistical methods by leveraging retrospective data collected during patient care.
Predictive analytics models can identify 83% of high-risk readmissions with a false positive rate of only 9%. This accuracy ensures that you receive timely care without unnecessary alarms.
AI also uses statistical methods, data mining, and machine learning to forecast outcomes. This approach helps healthcare providers identify high-risk patients and take preventive measures. For you, this means earlier detection and a higher likelihood of successful treatment.
Enhancing accuracy in pathology and genetic analysis
AI has transformed pathology and genetic analysis, making them faster and more accurate. Algorithms now analyze genetic markers to provide insights into your cancer risk and potential treatment responses. Tools like AlphaMissense and PrimateAI-3D outperform human experts in predicting the pathogenicity of genetic variants. This ensures you receive precise diagnoses and tailored care.
Experts like Dr. Danielle Elliott Range emphasize that AI enhances diagnostic accuracy when combined with human expertise. At Duke University, researchers refine predictive models to improve the reliability of disease progression forecasts. These advancements ensure that your treatment plan is based on the most accurate and up-to-date information available.
Harnessing AI for Personalized Cancer Treatment

Tailoring therapies to individual patients using AI
AI has made it possible to design cancer treatments that are as unique as you are. By analyzing vast amounts of data, including your genetic profile, medical history, and tumor characteristics, AI helps oncologists create therapies tailored specifically to your needs. This approach ensures that you receive treatments that are more effective and less likely to cause unnecessary side effects.
For instance, AI can identify tumor borders with remarkable precision, enabling targeted therapies that minimize damage to healthy tissues. It also uses pattern recognition to predict how your body might respond to immunotherapy, a treatment that boosts your immune system to fight cancer. This means you can benefit from therapies that are not only personalized but also optimized for your specific condition.
Here’s a breakdown of the types of data AI uses to personalize cancer treatments:
Data Type | Number of Articles | Percentage |
|---|---|---|
Patient Medical Records | 27 | |
Biological Samples | 4 | 1.847% |
Genomic Data | 14 | 30.4% |
Radiomic Data | 12 | 5.52% |
Radiogenomic Data | 3 | 1.38% |
Drug Response Data | 24 | 52.3% |
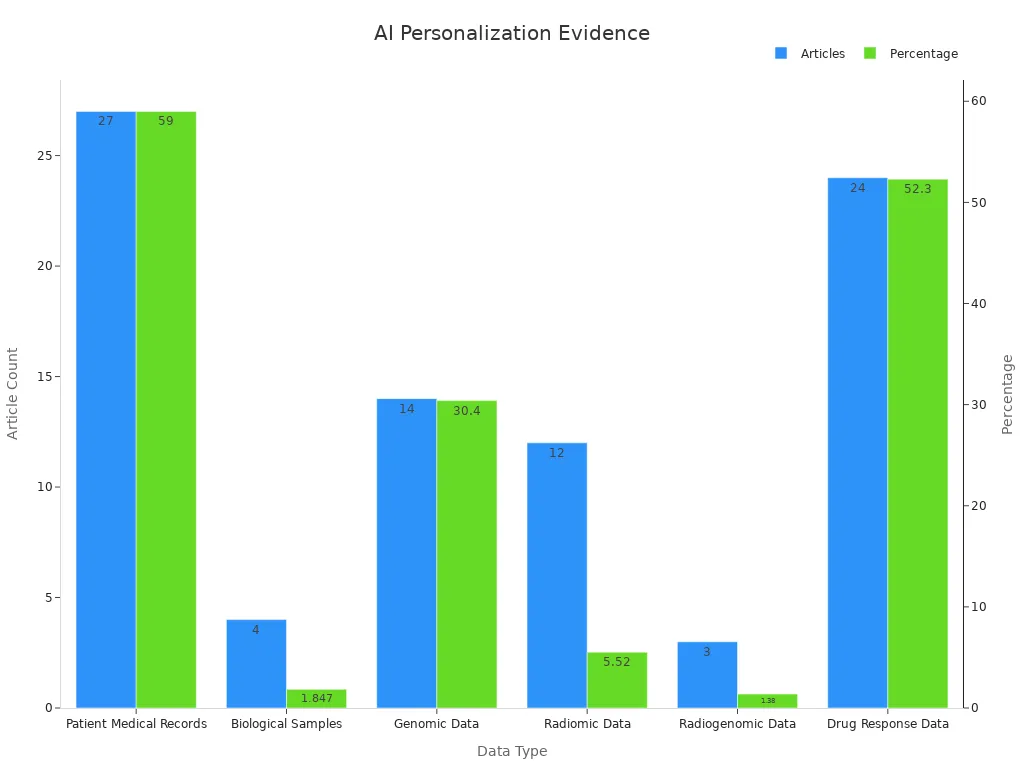
By leveraging these data types, AI ensures that your treatment plan is not only scientifically sound but also highly personalized.
Predicting treatment outcomes with AI algorithms
AI algorithms excel at predicting how well a treatment will work for you. These tools analyze patterns in clinical data to forecast outcomes, helping doctors make informed decisions about your care. For example, AI can evaluate genomic signatures to predict whether a specific drug will slow the progression of your cancer. This allows you to avoid ineffective treatments and focus on those with the highest likelihood of success.
Studies have validated the reliability of AI in predicting treatment outcomes. For instance:
Metric | Description | Example Value |
|---|---|---|
AUROC | Evaluates the discrimination ability of AI models | |
Precision | Indicates reliability of positive predictions | High |
Recall | Measures effectiveness in detecting actual cases | High |
F1-Score | Balances precision and recall | Essential in clinical applications |
Calibration Plots | Ensures predicted probabilities align with real outcomes | Critical for therapy decisions |
Clinical Impact Metrics | Relates directly to patient outcomes | Improvement in overall survival |
These metrics highlight how AI can guide your treatment journey with accuracy and confidence. For example, a study combining genomic sequencing and pathology image analysis improved prognostic accuracy across multiple cancer types. This means you can trust AI to provide insights that enhance your chances of recovery.
Real-world applications of AI in personalized oncology care
AI is already transforming cancer care in real-world settings. Platforms like next-generation sequencing (NGS) use AI to analyze genetic data, helping oncologists choose the most effective treatments for you. Dr. Douglas Flora, a leading oncologist, emphasizes that AI's pattern recognition capabilities reduce data overload and improve decision-making. This ensures that your treatment plan is both evidence-based and highly personalized.
AI also plays a crucial role in tracking your progress during treatment. It improves measurement consistency, allowing doctors to monitor how well your therapy is working. For example, AI can analyze imaging data to detect subtle changes in tumor size, helping your care team adjust your treatment plan as needed. This level of precision ensures that you receive the best possible care at every stage of your journey.
In addition, AI has revolutionized cancer screening by identifying early signs of the disease. This not only improves patient outcomes but also enhances clinical decision-making. By integrating AI into oncology, healthcare providers can offer you treatments that are not only effective but also tailored to your unique needs.
Harnessing AI in Drug Discovery for Cancer Treatment
Accelerating the development of innovative cancer drugs
AI is reshaping how cancer drugs are developed. By analyzing massive datasets, AI identifies potential drug targets faster than traditional methods. This means researchers can pinpoint therapeutic improvements and streamline the drug approval process. For you, this translates to quicker access to life-saving treatments.
AI also integrates with clinical genomics to revolutionize drug development. It helps identify genetic targets and designs clinical trials with higher success rates. This approach ensures that new drugs reach patients like you more efficiently. The ability to predict outcomes and refine drug candidates early in the process reduces delays, making treatments available sooner.
Reducing costs and timelines in drug research
AI significantly lowers the cost of cancer drug development. It optimizes processes like study design and patient recruitment, which are often time-consuming and expensive. For example, AI can save up to 50% of costs when a drug reaches the clinical phase. It also shortens recruitment time by 20-40%, ensuring trials progress faster.
Evidence Description | Impact on Research Costs | Source |
|---|---|---|
AI can save 25-50% of costs when a drug reaches the clinical phase. | 25-50% | Sobhani, D'Angelo, Pittacolo, Mondani, & Generali, 2024 (Nature, 2023) |
AI reduces recruitment time by 20-40%. | 20-40% | Hutson, 2024 |
AI optimizes study design, shortening planning by up to 50%. | 50% | N/A |
These advancements mean you benefit from innovative treatments without the long wait or high costs traditionally associated with drug development.
Success stories of AI-driven breakthroughs in oncology
AI has already achieved remarkable milestones in oncology drug discovery. For instance:
IBM Watson for Oncology aimed to assist oncologists by analyzing vast datasets to recommend personalized treatments. While it faced challenges in real-world applications, it highlighted the potential of AI in transforming cancer care.
AI-driven platforms have successfully identified promising drug candidates, accelerating their journey from research to clinical trials.
These examples show how AI is paving the way for breakthroughs that could improve your treatment options and outcomes.
Addressing Challenges in AI for Cancer Care
Mitigating biases in AI algorithms
AI algorithms can unintentionally reflect biases present in their training data. These biases can lead to misdiagnoses or unequal treatment outcomes. For example, some algorithms have shown disparities in resource allocation for black patients and underperformance in detecting skin conditions on darker skin tones. You might wonder how these issues arise. They often stem from datasets that lack diversity or fail to represent all demographics equally.
To address this, researchers use strategies like statistical analysis and auditing tools. Diverse datasets play a crucial role in ensuring fairness. When AI systems undergo regular audits, they become more transparent and reliable. By incorporating these practices, healthcare providers can reduce bias and improve equity in cancer care.
Tip: Diverse datasets and regular audits are essential for creating fair and unbiased AI systems.
Ensuring data privacy and security in AI applications
AI applications in oncology rely on sensitive patient data, making privacy and security critical concerns. Regulations like HIPAA and GDPR protect your information, ensuring it remains confidential. Non-compliance with these laws can result in hefty fines for healthcare organizations. For example, hospitals have faced penalties for failing to safeguard patient data.
Differential privacy (DP) offers a solution by enabling AI models to learn from data without exposing individual details. This technique prevents data reconstruction and ensures compliance with privacy regulations. Healthcare organizations also develop cybersecurity frameworks to proactively protect your information from breaches.
Note: Continuous education and adherence to regulatory frameworks help maintain trust in AI-driven healthcare.
Promoting equitable access to AI-driven cancer technologies
AI has the potential to transform cancer care, but not everyone benefits equally. Access to AI-driven technologies often depends on factors like geographic location, healthcare infrastructure, and socioeconomic status. You might face challenges accessing these innovations if you live in underserved areas or lack financial resources.
To promote equity, healthcare systems must prioritize affordability and accessibility. Governments and organizations can invest in infrastructure and subsidize costs for low-income patients. By ensuring equitable access, AI can truly revolutionize cancer care for everyone, regardless of their circumstances.
Callout: Equitable access to AI technologies ensures that advancements in cancer care benefit all patients, not just a privileged few.
The Future of Harnessing AI in Cancer Detection and Treatment
Emerging trends in AI for oncology
AI continues to evolve, bringing exciting advancements to oncology. You can expect models that predict cancer risk with accuracy comparable to human experts. These tools will enable more targeted screening and prevention trials, improving early detection rates. Multimodal data analysis is another promising trend. By combining information from imaging, genomics, and pathology, AI can provide a more comprehensive understanding of your condition, leading to better treatment decisions.
Collaboration between AI researchers and clinicians is becoming essential. This partnership ensures that AI tools are effectively implemented in clinical settings and understood by healthcare providers. Efforts to address biases in AI are also gaining momentum. Large-scale testing on diverse populations will help ensure equitable care for everyone.
Here are some key developments shaping the future of AI in oncology:
The AI in oncology market is projected to grow at a compound annual growth rate (CAGR) of 21.4% until 2035.
Global spending on artificial intelligence is expected to exceed USD 110 billion by 2024.
Nearly USD 6 billion has been invested in AI in oncology over the past five years.
Recent collaborations, such as Lunit's partnership with Japan National Cancer Center Hospital East and Roche's work with Ibex Medical Analytics, highlight the growing focus on precision oncology.
AI's role in preventive cancer care
AI is transforming preventive cancer care by identifying risks before symptoms appear. Predictive models analyze your health data to forecast potential cancer development. These tools allow healthcare providers to intervene early, reducing your chances of developing advanced-stage cancer. For example, AI can assess lifestyle factors, genetic predispositions, and environmental exposures to create personalized prevention plans tailored to your needs.
Preventive care also benefits from AI's ability to monitor trends across populations. By analyzing large datasets, AI identifies patterns that help public health officials design effective cancer prevention campaigns. This proactive approach ensures that you and others receive the resources needed to stay healthy.
Ethical considerations for AI in healthcare
The ethical use of AI in healthcare requires careful planning and ongoing dialogue. You might wonder how AI recommendations impact vulnerable populations. Studies emphasize the importance of monitoring these effects and documenting override decisions when healthcare providers disagree with AI suggestions. Transparency and accountability are critical for building trust in AI-driven systems.
Equity remains a central concern. AI tools must be designed to serve all patients fairly, regardless of their background. Training programs for healthcare providers, often called "AI literacy," are essential. These programs help doctors understand AI's strengths and limitations, ensuring that you receive care informed by both human expertise and advanced technology.
Note: Ethical frameworks should prioritize equity, transparency, and accountability to guide the responsible use of AI in healthcare.
AI is reshaping cancer care, offering you earlier diagnoses, personalized therapies, and faster drug development. Its ability to analyze blood vessel patterns around lung tumors helps predict treatment resistance, giving you insights into potential outcomes sooner. Experts like Elizabeth Krupinski highlight how AI improves mammogram accuracy, allowing radiologists to focus on critical cases. By identifying tumor borders with precision, AI enables targeted therapies that reduce side effects and improve your quality of life.
While challenges like bias and data privacy persist, ongoing advancements and ethical practices will guide AI's growth in oncology. By 2025 and beyond, AI holds the promise to revolutionize cancer care, improving outcomes for patients like you worldwide.
FAQ
What role does AI play in cancer detection?
AI helps detect cancer early by analyzing medical images and identifying abnormalities. It improves accuracy, reduces false positives, and ensures faster diagnoses. For example, AI-powered tools can detect subtle changes in mammograms or CT scans that might go unnoticed by human experts.
How does AI personalize cancer treatments?
AI tailors treatments by analyzing your genetic data, medical history, and tumor characteristics. It predicts how your body will respond to therapies like immunotherapy. This ensures you receive treatments that are more effective and cause fewer side effects, improving your overall care experience.
Can AI predict cancer risks?
Yes, AI uses predictive analytics to assess your risk of developing cancer. It analyzes patterns in your health data, such as genetic predispositions and lifestyle factors. This allows healthcare providers to intervene early, offering you preventive care and reducing the likelihood of advanced-stage cancer.
Is AI reliable in drug discovery for cancer?
AI accelerates drug discovery by analyzing large datasets to identify potential drug targets. It reduces research costs and timelines, ensuring faster access to innovative treatments. AI also improves the success rate of clinical trials by designing better study protocols and identifying suitable candidates.
Are there ethical concerns with AI in cancer care?
Yes, ethical concerns include biases in AI algorithms, data privacy, and equitable access to AI technologies. Researchers address these issues by using diverse datasets, ensuring compliance with privacy laws, and promoting affordability. These efforts aim to make AI-driven cancer care fair and trustworthy for everyone.
See Also
Recognizing Symptoms and Treatment Options for Duodenal Cancer
An In-Depth Overview of Various Cancer Types Available
Identifying Symptoms and Treatment Approaches for Conjunctival Melanoma
Exploring Cancer Types Associated with AIDS and Their Impact

