How Big Data Is Revolutionizing Cancer Research and Treatment
Big data and artificial intelligence now change how scientists study and treat cancer. The National Cancer Institute’s Genomic Data Commons holds information from over 32,000 patients with more than 60 cancer types. AI models can spot hidden signs in images and gene patterns, leading to earlier and more accurate diagnoses. Doctors use these tools for personalized therapies and smarter clinical trials. Harnessing Big Data for Breakthroughs in Cancer Research brings faster discoveries, better predictions, and improved patient care.
Key Takeaways
Big data and AI help doctors find cancer earlier and choose treatments tailored to each patient’s unique disease.
Different types of data, like genetics, images, and clinical records, work together to improve cancer research and care.
AI speeds up discoveries by spotting hidden patterns in cancer cells and patient information that humans might miss.
Using big data makes clinical trials faster and more successful by matching the right patients with the right treatments.
Decision support tools powered by big data help doctors and patients make smarter, more confident choices about cancer care.
What Is Big Data?
Big data in cancer research means working with huge amounts of information that come in quickly and from many different sources. Scientists call this the “three Vs”: volume, velocity, and variety. These large datasets need special computer tools and methods to turn them into useful knowledge. For example, The Cancer Genome Atlas (TCGA) holds 2.5 petabytes of raw data, which is about 2,500 times more than a modern laptop can store. This data includes many types, such as DNA, proteins, and even images of cancer cells. Researchers cannot handle this much information alone, so they use advanced computers and artificial intelligence to help.
Data Types in Oncology
Cancer research uses many kinds of data to understand the disease and find better treatments. Some of the most important data types include:
Genomics: DNA information helps scientists find mutations that cause cancer, like changes in the EGFR or KRAS genes.
Proteomics and Metabolomics: These show which proteins and chemicals are active in cancer cells, helping to discover new drug targets.
Single-cell Data: This type reveals differences between individual cancer cells, showing how tumors change and grow.
Imaging: Pictures from scans and microscopes help doctors see tumors and track how they respond to treatment.
Clinical Trials Data: Information from studies tests new treatments and finds which patients benefit most.
Real-world Data: Electronic health records and data from wearable devices show how treatments work in everyday life.
These data types work together to give a full picture of cancer and its treatment.
Why It Matters
Big data changes how doctors and scientists fight cancer. It helps them find new cancer types, match patients with the best treatments, and predict how well therapies will work. The table below shows how different data types help at each stage of research and care:
Research Phase | Data Type | Impact on Cancer Care |
|---|---|---|
Genomics | Finds new cancer subtypes and guides drug discovery | |
Translation | Multiomics | Improves understanding of tumors and helps design better studies |
Clinical Trials | Biomarker Data | Tests new drugs for specific patient groups |
Delivery | Real-world and AI Data | Helps doctors choose the best treatment for each patient |
Big data gives researchers and doctors the power to make smarter decisions, leading to better outcomes for people with cancer.
Harnessing Big Data for Breakthroughs in Cancer Research
AI and Pattern Discovery
Researchers use AI and big data to find new patterns in cancer that people cannot see with the naked eye. AI tools can look at thousands of images, genetic codes, and patient records in seconds. This helps scientists spot tiny changes in cells or genes that signal cancer. By harnessing big data for breakthroughs in cancer research, teams can discover new biomarkers. Biomarkers are signs in the body that show if cancer is present or how it might behave.
AI-driven radiomics, for example, uses computer programs to study CT scans of lung cancer. These programs find patterns that doctors might miss. PathAI uses AI to look at breast cancer tissue slides. It finds cancer more accurately than many pathologists. Tempus uses AI to combine genetic and clinical data. This helps doctors choose the best treatment for each patient. IBM Watson for Oncology reviews health records and clinical trial data to suggest treatments for prostate cancer. Guardant Health uses AI to study tumor DNA in blood, helping doctors track cancer without surgery.
AI and big data work together to speed up discoveries and improve accuracy in cancer research.
Here is a table showing how different AI approaches help in harnessing big data for breakthroughs in cancer research:
Study / Application | AI Approach | Data Types | Outcomes / Statistical Evidence |
|---|---|---|---|
AI-driven Radiomics for Lung Cancer | AI algorithms analyzing CT radiomic features | CT imaging data | Improved early detection rates; found patterns missed by clinicians |
PathAI Breast Cancer Diagnosis | AI analysis of histopathological images | Histopathology images | Higher accuracy than pathologists; reduced diagnostic errors |
Tempus Genomic Profiling | AI platform integrating genomic and clinical data | Genomic profiles and clinical outcomes | Identified biomarkers for personalized treatments; improved response rates and survival |
IBM Watson for Oncology in Prostate Cancer | AI analyzing EHR and clinical trials data | Electronic health records and clinical trial data | Provided evidence-based treatment recommendations |
Guardant Health Liquid Biopsy | AI-powered analysis of tumor DNA in blood | Liquid biopsy (circulating tumor DNA) | Detected mutations and monitored treatment response in colorectal cancer |
Scientists also use deep learning to study data from many sources. Qi and his team used deep learning with Raman spectroscopy to tell healthy lung tissue from cancerous tissue with 95% accuracy. Sakda Khoomrung’s group combined different types of data to find new cancer biomarkers. Ken Bloom’s team used AI to help pathologists find tissue biomarkers more precisely. Takuji Yamada’s research found bacteria in the gut that signal colorectal cancer risk. Kountay Dwivedi’s group built an explainable AI system to help doctors trust the results.
Study / Research Group | AI Methodology | Data Type | Key Findings / Statistical Results |
|---|---|---|---|
Qi et al. | Deep learning with Raman encoding | Raman spectroscopy data | 95% accuracy in telling healthy from cancerous lung tissue |
Sakda Khoomrung et al. | Deep learning with multi-omic and clinical data | Multi-omic and clinical datasets | Found new cancer biomarkers; classified disease types |
Ken Bloom, Nucleai | AI-powered tissue biomarker analysis | Histology slides | Improved precision and reproducibility in biomarker detection |
Takuji Yamada et al. | AI analysis of gut microbiome data | Microbiome data in colorectal cancer | Found bacterial patterns as biomarkers for colorectal cancer risk |
Kountay Dwivedi et al. | Explainable AI (XAI) framework | Molecular and imaging data for NSCLC | Improved workflow for biomarker discovery with better interpretability |
Harnessing big data for breakthroughs in cancer research allows teams to move faster and find answers that save lives.
Clinical Trials and Predictive Analytics
Clinical trials test new cancer treatments. In the past, these trials took a long time and often failed because they could not find the right patients or predict who would benefit. Now, harnessing big data for breakthroughs in cancer research changes how trials work. AI and predictive analytics help researchers design better studies, pick the best patients, and spot problems early.
Predictive models use big data to guess which patients will respond to a treatment. These models look at genetic data, health records, and even data from wearable devices. They help doctors match patients to the right trial. This makes trials faster and more successful.
A recent study showed that using predictive analytics improved trial results. The model had an area under the ROC curve (AUC) of 80%, which means it could tell who would benefit from a treatment most of the time. The balanced accuracy was 70%, and the F1 score was 42%. These numbers show that AI can help researchers make better choices during trials.
Performance Metric | Value | Description |
|---|---|---|
ROC-AUC | 80% | Shows strong ability to tell who will benefit from treatment |
Balanced Accuracy | 70% | Measures how well the model works with different patient groups |
F1 Score | 42% | Combines precision and recall to show overall predictive power |
Harnessing big data for breakthroughs in cancer research also improves how trials run. Integrated data systems cut protocol deviations by 42% and reduced data queries by 36%. Adaptive trials, which change as they go, were 60% more likely to move new drugs to the next phase. Predictive analytics shortened recruitment by 30%. AstraZeneca used an AI platform that cut enrollment time by 45% and brought in more diverse patients. Most drug companies now use cloud systems for trials, with 78% adopting this technology. About 67% of companies said their data quality improved.
Improvement Metric | Numerical Value | Description |
|---|---|---|
Reduction in protocol deviations | 42% | Fewer mistakes in trial procedures |
Decrease in data queries | 36% | Less time spent fixing data problems |
Higher success rate in adaptive trials | 60% | More new drugs moved to the next phase |
Reduction in recruitment phase duration | 30% | Trials found patients faster |
Enrollment time reduction (AstraZeneca) | 45% | AI helped enroll patients quicker and increased diversity |
Adoption of cloud infrastructure | 78% | Most companies now use cloud systems for trials |
Reported improvement in data quality | 67% | Companies saw better data quality and easier access |
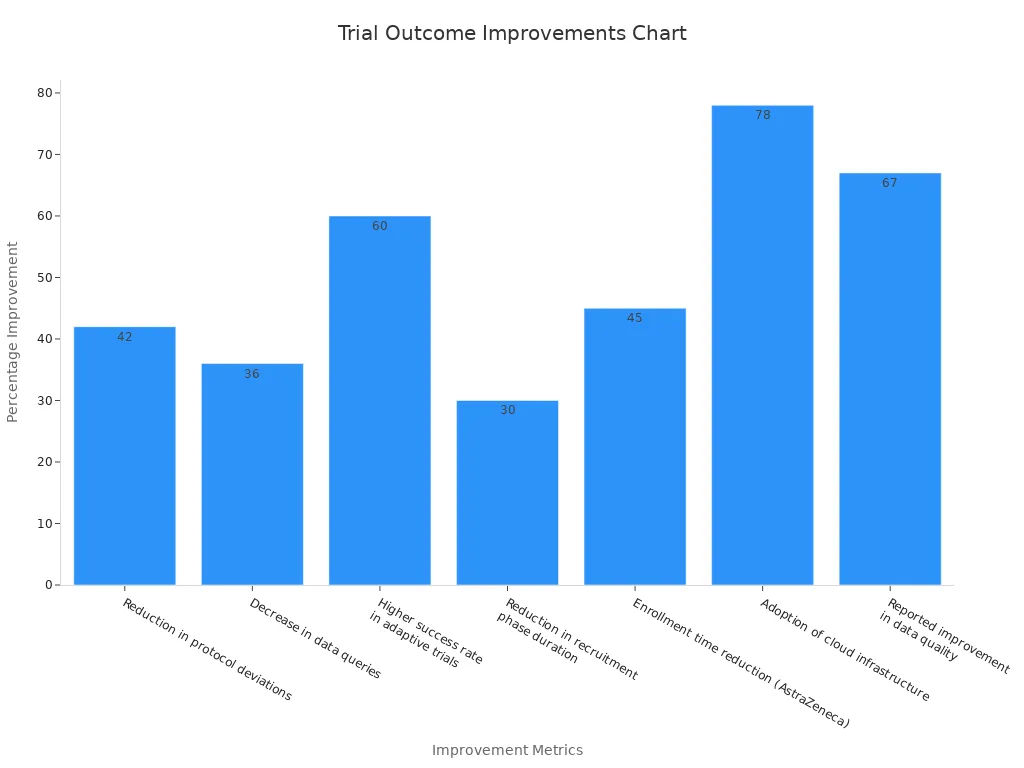
Harnessing big data for breakthroughs in cancer research leads to smarter, faster, and more successful clinical trials. Patients get access to new treatments sooner, and doctors learn what works best for each person.
Big Data in Cancer Treatment
Precision and Personalized Medicine
Big data has changed how doctors treat cancer. Precision medicine uses information from each patient to find the best treatment. Doctors look at genes, proteins, and even lifestyle habits. They use this data to match patients with therapies that work best for them.
Personalized medicine stands out from older methods. In the past, doctors gave the same treatment to everyone with the same cancer type. Now, they can find small differences in tumors. These differences help doctors choose drugs that target the cancer more directly.
Recent studies show how big data improves patient outcomes:
A Phase II clinical trial found that targeted therapy based on genomic analysis helped patients with metastatic breast cancer live longer.
Machine learning on large pathology datasets reduced misdiagnosis and unnecessary biopsies. This lowered medical costs for patients.
Radiology models using data from many hospitals predicted which patients would respond to chemotherapy. This guided doctors to choose the right treatment.
Big data analytics helped doctors sort breast cancer patients into groups. They could quickly adjust treatment plans and reduce side effects.
Combining genetic, clinical, and lifestyle data improved survival rates, cut healthcare costs, and shortened hospital stays.
Doctors now use precision medicine to give each patient a treatment plan that fits their unique cancer.
Clinical studies provide more details about these advances. The table below shows how different programs and studies have used big data to improve care for lung cancer patients:
Study / Program | Patient Population | Intervention / Focus | Numerical Evidence | Limitations |
|---|---|---|---|---|
Multiple RWD studies | Advanced non-small cell lung cancer (aNSCLC) patients with driver mutations | Broad molecular testing and genotype-directed therapy | Improved overall survival in patients with driver-mutation positive tumors | Did not assess impact of nationwide precision medicine program implementation |
Bruno et al. | Stage IV NSCLC patients in academic-community network | Precision medicine thoracic service with increased NGS testing | Higher NGS testing rates; more actionable alterations found | Control group pre-implementation; no survival data studied |
Presley et al. | aNSCLC patients with broad genomic sequencing vs. routine EGFR/ALK testing | Comparison of broad genomic sequencing vs. routine testing | Comparable survival rates between groups | Study population not fully representative; effectiveness of program not directly studied |
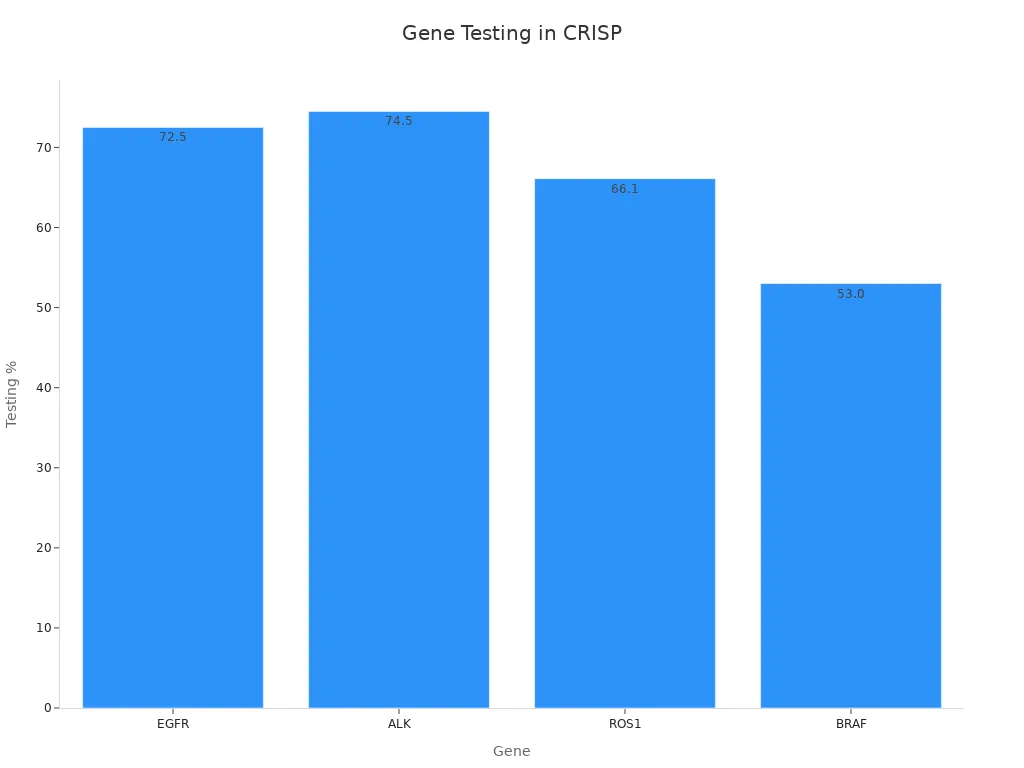
German registry (CRISP) | Non-squamous aNSCLC patients | Molecular testing rates for driver mutations (EGFR, ALK, ROS1, BRAF) | Testing rates: EGFR 72.5%, ALK 74.5%, ROS1 66.1%, BRAF 53.0% | Low percentage tested for all mutations; challenges in routine care |
nNGM program | aNSCLC patients in Germany | NGS-based diagnostics, decision support, trial matching | Cost coverage for ~93% of insured lung cancer patients; nationwide program | Full impact on survival outcomes still under evaluation |
Doctors and scientists continue to improve these methods. Clinical trials now use omics tests to find new biomarkers. These tests help doctors know which treatments will work best. Experts use strict rules and advanced statistics to make sure these tests are reliable. As more teams work together, the number of successful precision medicine trials will grow.
Personalized medicine also changes how doctors spend money and time. Spending on precision medicine is rising. Clinical trials now focus on finding the right patients for each drug. Machine learning helps doctors find patterns in large datasets. This makes treatments more effective and efficient. Doctors now use genetic, lifestyle, and environmental data to choose the best care for each person.
Decision Support Tools
Big data also powers decision support tools in cancer care. These tools help doctors and patients make better choices. They use information from thousands of patients to predict what might happen next.
Researchers build models using data from many cancer types. For example:
Prognostic models use data from about 17,000 melanoma, 186,000 breast cancer, and 34,000 prostate cancer patients. These models include clinical, tumor, imaging, biomarker, and treatment data.
The models predict outcomes like survival and quality of life. This helps doctors and patients choose treatments that match patient goals.
The PATH framework helps doctors see how different treatments work for different people. It gives personalized predictions for each patient.
Prognostic algorithms measure uncertainty and include patient preferences. This supports shared decision-making between doctors and patients.
The 4D PICTURE project develops algorithms to improve prediction accuracy. These tools help doctors and patients understand risks and benefits.
Decision support tools give doctors and patients more confidence when choosing cancer treatments.
Breast cancer tools use strong math and statistics. Fourteen out of twenty-one reviewed tools were validated, showing they work well. Most tools use age, tumor size, grade, and lymph node status to personalize advice. Some tools, like the 'Age Gap Decision Tools,' were tested in real-world clinics. These tools increased patient knowledge and helped patients and doctors make decisions together.
Some tools are made for doctors, while others are for patients. This changes how the information looks and how complex it is.
Including more patient details, like other health problems or race, can make these tools even better.
The best tools help patients understand their options and feel more involved in their care.
Big data and decision support tools now guide cancer treatment. They help doctors give the right care to the right patient at the right time. This leads to better outcomes and more satisfied patients.
Real-World Impact
Early Detection Successes
Big data tools help doctors find cancer earlier than ever before. AI models can scan thousands of images and spot tiny changes that signal cancer. Hospitals use these systems to review mammograms, lung scans, and skin photos. Doctors now find more early-stage cancers, which gives patients more treatment options.
Doctors detect more cases of ductal carcinoma in situ (DCIS) during breast cancer screening. This leads to a shift toward finding cancer at an earlier stage.
AI systems help spot small melanomas on the skin that doctors might miss.
Hospitals use big data to track which patients need more tests or follow-up visits.
Early detection often leads to higher survival numbers. However, experts warn that these numbers can sometimes be misleading. Finding cancer earlier does not always mean people live longer. Sometimes, early detection finds cancers that would never cause harm. This can lead to extra treatments and worry for patients.
Doctors and researchers now look for ways to measure real success. They focus on reducing deaths from cancer and improving quality of life, not just finding more cases.
Improved Outcomes
Big data also helps improve how doctors treat cancer. Hospitals use large databases to compare treatments and see which ones work best. Doctors use this information to choose the right therapy for each patient.
Benefit | Example |
|---|---|
Better treatment match | Doctors use genetic data to pick drugs that target a patient’s tumor. |
Fewer side effects | AI tools help avoid treatments that may not work or cause harm. |
Faster recovery | Hospitals track patient progress and adjust care plans quickly. |
Doctors now see more patients living longer with cancer. However, experts say that measuring true improvement is complex. Survival rates can look better when doctors find cancer earlier, but this does not always mean people live longer. The best measure of success is when fewer people die from cancer and patients feel better during and after treatment.
Big data gives doctors new ways to track progress and focus on what matters most—helping patients live longer, healthier lives.
Challenges and Future Directions
Data Quality and Privacy
Big data in cancer research brings many challenges. Data quality stands out as a major concern. Researchers often collect huge amounts of information, but not all of it is accurate or complete. Clinical data can be messy because doctors use free text instead of structured forms. This makes it hard to combine and analyze information from different hospitals. CancerLinQ and the Veterans Health Administration (VHA) show real-world examples of these problems. CancerLinQ works to clean and organize both structured and unstructured data. The team uses a common data model and follows HIPAA rules to protect patient privacy. The VHA faces tough choices about sharing data while keeping veterans’ information safe. They use special processes to remove personal details and standardize data formats.
Privacy remains a top concern. Even after removing names, there is still a risk that someone could identify a patient. The United States does not have one clear law for data privacy. Hospitals must follow rules like HIPAA and GDPR, which can change over time. No technology can guarantee total privacy. Teams use a mix of access controls, anonymization, and encryption to keep data safe.
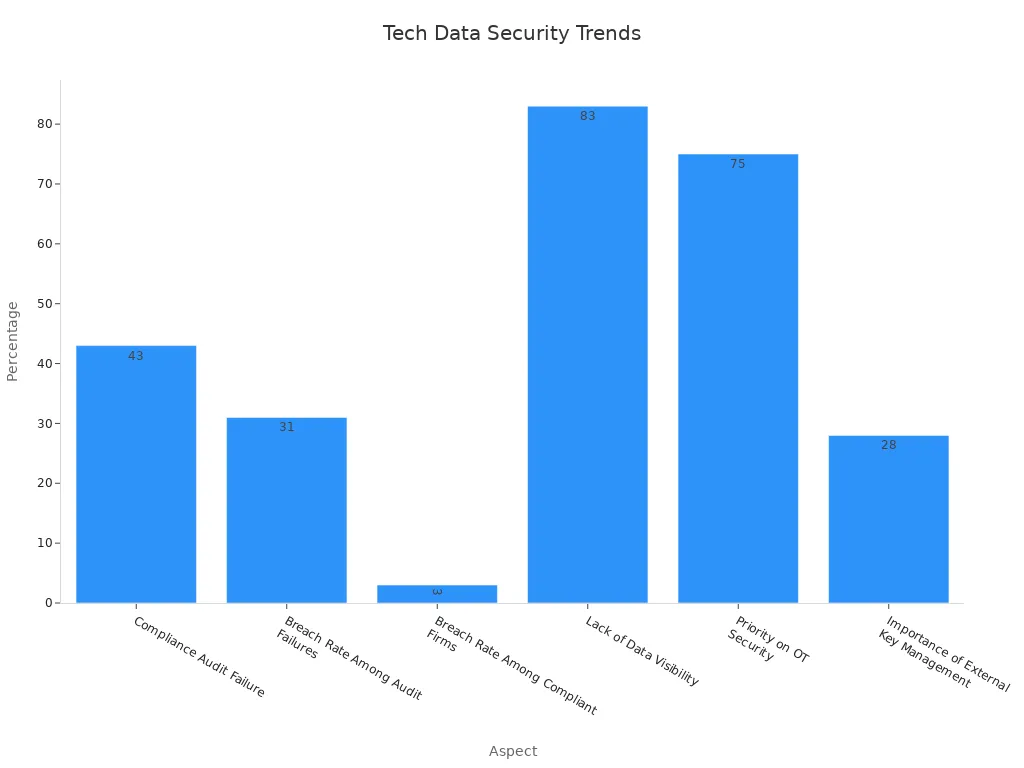
Recent advances in technology help address these risks. Many IT leaders now use AI-powered Data Security Posture Management (DSPM) tools. These tools help find and protect sensitive data, even in unstructured formats. The chart below shows how organizations focus on security and compliance:
Integration and Best Practices
Combining different types of data improves cancer research. Researchers now link radiology, pathology, genomics, and clinical records. This helps doctors predict how patients will respond to treatment. Multimodal data also helps find which patients benefit from new drugs. The GENIE BPC NSCLC project shows how standardizing clinical and genomic data supports large-scale studies. Quality checks and clear clinical notes make these datasets more reliable.
Integrated data helps predict cancer outcomes and treatment responses.
Multimodal approaches improve the accuracy of immune therapy predictions.
Projects like RUBIES combine clinical trial, imaging, and electronic health record data for better evidence.
Adding socioeconomic data helps explain differences in treatment access and results.
Flatiron Health uses integrated evidence to speed up research and improve trial design.
Researchers see that best practices in data integration lead to more reliable results. They use reproducible pipelines and strong quality controls. These steps reduce bias and make findings more useful for doctors and patients. As technology improves, integrated evidence will play a bigger role in cancer care and research.
Big data and AI have changed cancer care for everyone. Doctors, patients, and researchers now use many types of information to make better choices. The table below shows how big data helps at every step:
Application Area | Transformative Impact |
|---|---|
Cancer Genomics | Finds key mutations and supports precision medicine |
Personalized Therapies | Matches treatments to each patient’s needs |
Predictive Analytics | Helps doctors plan care and spot high-risk patients early |
Machine Learning | Improves treatment planning and decision-making |
Doctors track patient progress, reduce hospital stays, and improve quality of life. Patients get care that fits their needs. Everyone benefits from safer, faster, and more effective treatments. Staying informed and supporting data-driven care will help shape a brighter future in cancer treatment.
FAQ
What is big data in cancer research?
Big data in cancer research means using huge amounts of information from many sources. Scientists study genes, images, and patient records. They use computers to find patterns and improve cancer care.
How does AI help doctors treat cancer?
AI helps doctors by finding patterns in data that humans might miss. It suggests the best treatments for each patient. AI also helps doctors spot cancer earlier and track how well treatments work.
Is patient data safe when used for research?
Researchers use strong security tools to protect patient data. They remove names and personal details. Hospitals follow strict rules like HIPAA to keep information private.
Can big data improve cancer survival rates?
Big data helps doctors find the best treatments faster. It also helps spot cancer early. These advances can lead to better survival rates and improved quality of life for patients.
What are the main challenges with big data in cancer care?
Doctors and researchers face problems with data quality and privacy. They also need to combine different types of data. Teams work hard to solve these issues and make data more useful.
See Also
An In-Depth Overview of Various Cancer Types
Exploring Large-Cell Lung Cancer and Its Categories
Recognizing Symptoms And Treatment Options For Duodenal Cancer
Defining Anaplastic Large Cell Lymphoma And Treatment Methods

