Hemangioblastoma Explained and Its Key Traits

Hemangioblastoma is a rare, non-cancerous tumor that develops in your central nervous system. It often forms in areas rich in blood vessels, such as the brain, spinal cord, or retina. These tumors account for about 2% of intracranial neoplasms and up to 10% of primary spinal cord tumors. Despite being benign, they can press on nearby structures, leading to neurological symptoms. You might experience headaches, muscle weakness, or coordination problems. Early diagnosis and treatment are crucial to prevent complications and improve your quality of life.
Key Takeaways
Hemangioblastomas are rare, non-cancerous growths in the brain or spine. They can cause headaches and trouble with movement.
Finding them early is very important. If you have bad headaches or blurry vision, see a doctor quickly.
Surgery is the best way to treat hemangioblastomas. It helps reduce symptoms and makes life better.
Your genes can raise the chance of getting hemangioblastomas. Von Hippel-Lindau syndrome is one example. Genetic tests can check your risk.
Regular doctor visits are needed to watch for symptoms or new growths.
What Is a Hemangioblastoma?
Definition and Characteristics
A hemangioblastoma is a benign vascular tumor that develops in your central nervous system (CNS). These tumors are classified as CNS WHO grade 1, meaning they are non-cancerous and slow-growing. They often arise in the cerebellum, brainstem, or spinal cord. Hemangioblastomas are highly vascular, meaning they contain many blood vessels. This feature makes them distinct from other CNS tumors. You may encounter these tumors either sporadically or as part of von Hippel-Lindau (VHL) disease, a genetic condition that increases the risk of multiple tumors. About 20-30% of hemangioblastomas are linked to VHL disease. Their slow growth can still cause significant symptoms due to their location and size.
Common Locations in the Body
Hemangioblastomas most commonly occur in specific parts of your CNS. The cerebellum, which controls balance and coordination, is the most frequent site, accounting for 45-50% of cases. The spinal cord follows closely, with 40-45% of cases. Less commonly, these tumors appear in the brainstem (5-10%) or the retina. The table below summarizes these locations:
Location | Description |
|---|---|
Cerebellum | Typically located in the posterior parts |
Spinal Cord | Commonly found in the spinal cord |
Brainstem | Occurrences noted in the brainstem |
Retina | Rare occurrences in the retina |
These locations explain why hemangioblastomas often cause symptoms like headaches, muscle weakness, or vision problems.
Prevalence and Rarity
Hemangioblastomas are rare compared to other CNS tumors. They account for about 1-2.5% of all intracranial neoplasms and 2-10% of primary spinal cord tumors. In the posterior cranial fossa, they represent 8-12% of neoplasms. Despite their rarity, early diagnosis is essential to manage symptoms and prevent complications. If you experience symptoms, consulting a healthcare provider can help identify the condition early.
Causes and Risk Factors of Hemangioblastomas
Genetic Causes and von Hippel-Lindau Syndrome
Genetics play a significant role in the development of hemangioblastomas. Mutations in the VHL gene, which acts as a tumor suppressor, are a primary cause. These mutations can include missense changes, truncations, or deletions. Truncating mutations often lead to more severe outcomes. If you have von Hippel-Lindau (VHL) syndrome, your risk of developing hemangioblastomas increases significantly. Studies show that 60–80% of individuals with VHL syndrome develop central nervous system (CNS) hemangioblastomas. This strong link highlights the importance of genetic testing if you have a family history of VHL syndrome.
Sporadic Cases and Other Risk Factors
Not all hemangioblastomas are linked to inherited conditions. Sporadic cases, which occur without a family history, often result from spontaneous mutations in the VHL gene. These mutations disrupt normal cellular growth, leading to tumor formation. While VHL syndrome remains the most significant risk factor, sporadic cases show that anyone can develop this condition. Understanding these genetic changes can help you recognize the importance of early detection and medical evaluation.
Who Is Most at Risk?
You may be at higher risk of developing hemangioblastomas if you have VHL syndrome. This genetic condition predisposes you to multiple tumors, including those in the CNS. Sporadic cases, though less common, can affect individuals without a family history. If you experience symptoms like headaches, vision problems, or muscle weakness, seeking medical advice is crucial. Early diagnosis can improve outcomes and prevent complications.
Symptoms of Hemangioblastomas
General Symptoms
As a hemangioblastoma grows, it can press on nearby structures, leading to neurological symptoms. These symptoms often depend on the tumor's size and location. Common issues include headaches, weakness, and sensory changes. You might also experience balance problems or coordination difficulties. In some cases, the tumor can block the flow of cerebrospinal fluid, causing hydrocephalus, which leads to nausea, vomiting, and increased pressure in the brain.
Other symptoms you may notice include:
Vision problems, such as blurred vision or eye pain.
Weakness in your arms or legs.
Speech difficulties or cognitive challenges.
Dizziness, back pain, or numbness in your limbs.
Bowel or bladder dysfunction.
These symptoms can vary widely, but they often worsen as the tumor grows.
Symptoms by Tumor Location
The location of the hemangioblastoma plays a significant role in the symptoms you experience. For example:
Tumor Location | Symptoms |
|---|---|
Cerebral Hemangioblastoma | Vision problems, weakness, speech difficulties, cognitive difficulties. |
Cerebellar Hemangioblastoma | Headaches, dizziness, coordination problems, nausea and vomiting. |
Brainstem and Spinal Cord | Back pain, sensory changes, weakness or paralysis, bowel and bladder dysfunction. |
Larger tumors in the spinal cord may compress nerves, leading to numbness, clumsiness, or difficulty walking. Cerebellar tumors often affect coordination, making daily tasks challenging.
When to Seek Medical Advice
You should seek medical advice if you experience severe headaches or sudden neurological changes. Symptoms like vision loss, weakness, or difficulty walking also warrant immediate attention. If you notice signs of infection, such as fever or swelling near the affected area, consult a healthcare provider promptly. Early diagnosis can help prevent complications and improve your quality of life.
Diagnosing Hemangioblastomas
Medical History and Physical Examination
Diagnosing a hemangioblastoma begins with a thorough medical history and physical examination. Your doctor will ask detailed questions about your symptoms, such as headaches, vision problems, or neurological changes. They may also inquire about your family history, especially if there is a known occurrence of von Hippel-Lindau (VHL) syndrome or other hereditary conditions.
During the physical examination, your healthcare provider will assess your neurological function. This evaluation may include checking your reflexes, muscle strength, coordination, and sensory responses. These steps help identify any abnormalities that could point to the presence of a tumor in your central nervous system.
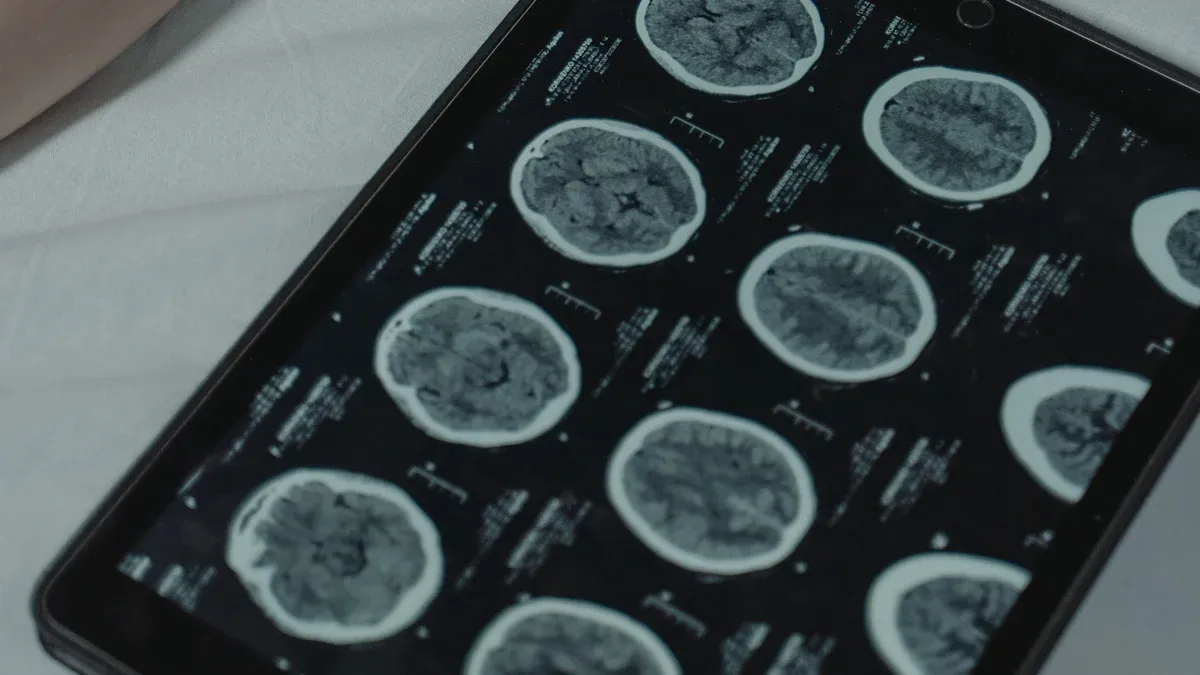
Imaging Techniques (MRI, CT Scans)
Imaging plays a critical role in confirming the diagnosis of a hemangioblastoma. Magnetic Resonance Imaging (MRI) is the preferred method due to its ability to produce detailed images of soft tissues. It can clearly show a well-defined, enhancing mass that distinguishes the tumor from surrounding tissue. Computed Tomography (CT) scans, while less detailed than MRI, are useful when MRI is not an option. CT scans can reveal the hypodensity of the tumor's cystic parts and show uniform enhancement with contrast.
Imaging Technique | Description |
|---|---|
Magnetic Resonance Imaging | Best for diagnosing hemangioblastomas; shows enhancing mass clearly delineated from surrounding tissue. |
Computed Tomography | Useful when MRI is contraindicated; can reveal hypodensity and uniform enhancement of tumors. |
Angiography | Evaluates tumor blood supply; useful for surgical planning. |
These imaging techniques not only confirm the presence of a tumor but also provide valuable information for treatment planning.
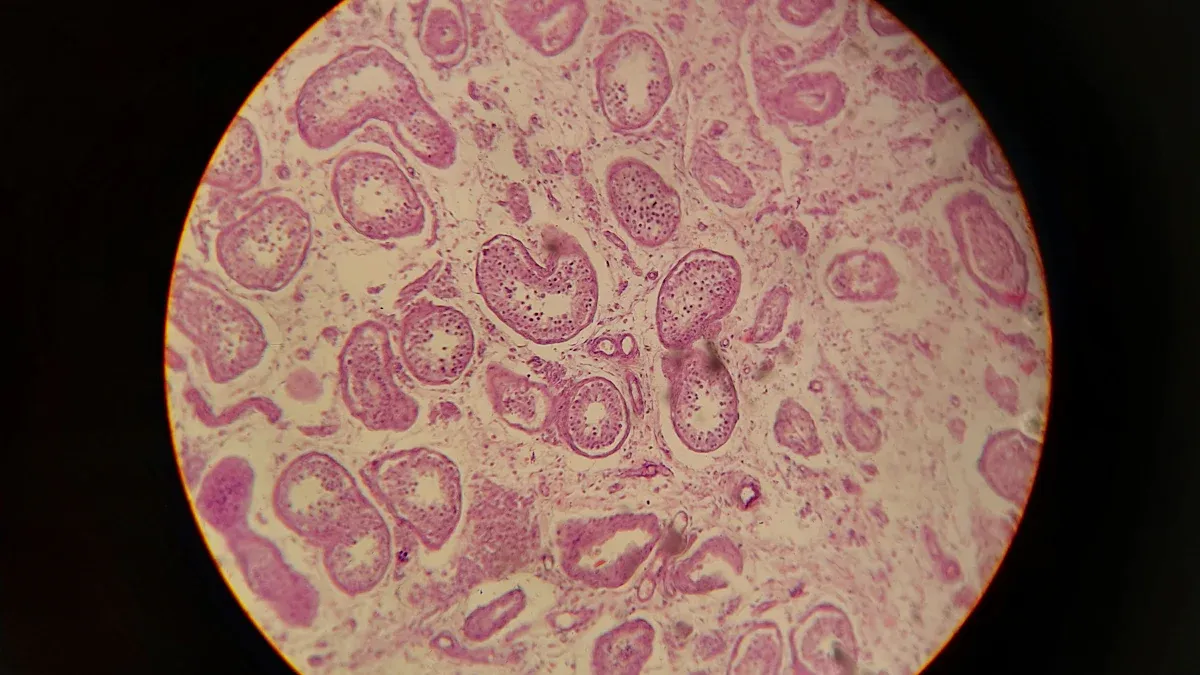
Biopsy and Laboratory Analysis
In some cases, a biopsy may be performed to confirm the diagnosis of a hemangioblastoma. This involves taking a small sample of the tumor tissue for microscopic examination. However, biopsies are not routinely used for diagnosing this condition. They are typically reserved for situations where imaging results are inconclusive or when a precise diagnosis is needed to guide treatment decisions.
By examining the tumor tissue, pathologists can identify the unique characteristics of a hemangioblastoma, ensuring that the diagnosis is accurate and that the treatment plan is appropriate for your condition.
Treatment Options for Hemangioblastomas
Surgical Removal
Surgical removal is the most common and effective treatment for hemangioblastomas. Since these tumors are benign and well-defined, surgeons can often remove them completely without damaging nearby tissues. Before surgery, your doctor will use imaging techniques like MRI or CT scans to map the tumor's location and plan the procedure. During surgery, the team will carefully dissect the tumor while maintaining hemostasis, as hemangioblastomas are highly vascular. Blood products are often kept on hand to manage potential blood loss.
After surgery, you will need regular follow-up appointments to monitor for recurrence. Neurological evaluations and imaging tests, such as MRIs, help ensure the tumor has not returned. Surgical excision offers a high success rate, with most patients experiencing significant symptom relief and improved quality of life.
Radiation Therapy
Radiation therapy is not always necessary for treating hemangioblastomas. Doctors may recommend it if surgery is not an option due to the tumor's location or your overall health. It is also considered for patients with multiple tumors, especially those associated with von Hippel-Lindau (VHL) disease. For small, asymptomatic tumors, a "watch-and-wait" approach with regular imaging may be more appropriate.
While radiation therapy can effectively control tumor growth, it may cause side effects. These include fatigue, skin irritation, headaches, and, in rare cases, radiation necrosis or secondary tumors. Your healthcare provider will weigh the benefits and risks before recommending this treatment.
Monitoring and Follow-Up Care
After treatment, ongoing monitoring is essential to ensure your recovery and prevent complications. You will need regular neurological evaluations and imaging tests, such as MRI or CT scans, to check for tumor recurrence or new growths. This is especially important if you have VHL disease, as it increases the risk of developing additional tumors.
Routine follow-up appointments allow your doctor to track your progress and address any lingering symptoms. Staying consistent with these visits helps you maintain your health and catch potential issues early. With proper care, most patients achieve a favorable long-term outlook.
Prognosis and Potential Complications
Recovery and Long-Term Outlook
The long-term outlook for individuals with hemangioblastomas is generally positive, especially when the tumors are diagnosed and treated early. Many patients experience significant symptom relief after treatment, with some achieving complete recovery. However, outcomes can vary. Some individuals may face persistent neurological challenges, such as coordination issues or sensory deficits, depending on the tumor's location and size.
Having a strong support system plays a vital role in recovery. Access to rehabilitation services, including physical and occupational therapy, can help you adapt to life after surgery. These services focus on improving mobility, strength, and overall quality of life. Regular follow-ups with your healthcare provider ensure that any lingering symptoms are addressed promptly.
Possible Complications
Complications can arise if hemangioblastomas are left untreated or improperly managed. These issues may occur during surgery, immediately after, or in the long term.
Type of Complication | Description |
|---|---|
Intraoperative Complications | Significant bleeding due to the vascular nature of tumors; risk of neurological deficits post-surgery. |
Postoperative Complications | CSF leaks, hydrocephalus, edema, swelling, and infection risks following surgery. |
Long-term Complications | Recurrence of tumors, long-term neurological deficits, vision problems, and endocrine disturbances. |
Understanding these risks highlights the importance of proper surgical planning and post-treatment care.
Importance of Regular Monitoring
Regular monitoring is essential for managing hemangioblastomas, especially if you have von Hippel-Lindau (VHL) disease. Imaging studies, such as MRI or CT scans, help detect new growths or changes in existing tumors. Routine check-ups allow your doctor to track your condition and address any complications early.
Continuous monitoring ensures no new tumors develop or existing ones grow.
Follow-up appointments help manage symptoms and maintain your overall health.
Staying consistent with these evaluations can improve your long-term prognosis and quality of life.
Understanding hemangioblastomas is essential for managing this rare condition effectively. These benign tumors, often linked to von Hippel-Lindau syndrome, originate from blood vessels in the brain or spinal cord. Symptoms vary based on tumor size and location, ranging from headaches to severe neurological issues.
Early diagnosis plays a critical role in improving outcomes. Recognizing causes, risk factors, and symptoms allows for timely treatment, which helps preserve your quality of life. Regular monitoring and a multidisciplinary approach ensure better management of potential complications.
If you experience symptoms like persistent headaches or vision problems, consult a healthcare professional promptly. Taking action early can make a significant difference in your recovery and long-term health.
FAQ
What makes hemangioblastomas different from other brain tumors?
Hemangioblastomas are benign and slow-growing. They originate from blood vessels, unlike malignant tumors that spread aggressively. These tumors often occur in the cerebellum or spinal cord and are highly vascular, which makes them unique.
Can hemangioblastomas turn into cancer?
No, hemangioblastomas remain benign. They do not transform into cancer. However, their growth can still cause serious symptoms by pressing on nearby structures in your central nervous system.
How is von Hippel-Lindau syndrome related to hemangioblastomas?
Von Hippel-Lindau (VHL) syndrome is a genetic condition that increases your risk of developing hemangioblastomas. About 20-30% of these tumors are linked to VHL. If you have a family history of VHL, genetic testing can help assess your risk.
Are there any lifestyle changes that can help manage hemangioblastomas?
Lifestyle changes cannot prevent or cure hemangioblastomas. However, maintaining regular medical check-ups and following your doctor’s advice ensures early detection and effective management. Staying informed about your condition also helps you make better health decisions.
What should you do if you suspect you have a hemangioblastoma?
If you notice symptoms like persistent headaches, vision problems, or muscle weakness, consult a healthcare provider immediately. Early diagnosis improves treatment outcomes and helps prevent complications. Don’t ignore neurological changes, even if they seem minor.
🧠 Tip: Keep a symptom diary to share with your doctor. It helps track changes and speeds up diagnosis.
See Also
Key Features and Insights About Craniopharyngioma Explained
Essential Information You Need About Ganglioneuroma
Fibrosarcoma Overview: Important Traits and Information

