Honeybee Venom Targets Breast and Ovarian Cancer

Honeybee venom and its key compound, melittin, show promise for treating aggressive breast and ovarian cancers. Many women face high risks from these cancers, especially in countries with limited healthcare. Breast cancer accounts for nearly a quarter of all female cancer cases worldwide, with younger women facing greater danger from aggressive types. Ovarian cancer also brings serious challenges, as shown in the table below:
Metric | Description | Range/Values |
|---|---|---|
Ovarian cancer incidence rate (per 100,000 women) | Country-specific rates | |
Ovarian cancer mortality rate (per 100,000 women) | Country-specific mortality rates | 1.9 (Malawi) to 12.8 (UK) |
Ovarian cancer survival rates (% of incident cases) | 1-year: 47.0% (Malawi) to 88.7% (Malaysia); 3-year: 38.5% (Malawi) to 76.4% (Malaysia); 5-year: 29.4% (Nigeria) to 46.5% (Australia) |
Recent honeybee venom cancer research brings hope for better treatments, but scientists still need to study safety and effectiveness. They continue to explore new options for patients who need help the most.
Key Takeaways
Melittin, a key protein in honeybee venom, shows strong ability to kill aggressive breast and ovarian cancer cells in lab studies.
Scientists use special delivery methods like nanoparticles to target cancer cells and reduce harm to healthy tissues.
Combining melittin with chemotherapy can make treatments more effective and may lower side effects for patients.
Current research is mostly in labs and animals; clinical trials are needed to confirm safety and benefits for people.
Researchers work to overcome challenges like side effects and drug resistance to develop safer, personalized cancer therapies.
New Treatment Needs

Current Limitations
Doctors face many challenges when treating aggressive breast and ovarian cancers. Standard therapies often do not work well for every patient. Many women develop resistance to hormone therapies like aromatase inhibitors and tamoxifen. This resistance means the drugs stop working over time. Ovarian cancer can be even harder to treat because some subtypes do not respond to hormone therapy at all.
Other treatments, such as surgery and chemotherapy, also have limits. Surgery may not remove all cancer cells, especially when the disease has spread. Chemotherapy can shrink tumors, but many cancers become resistant or come back after treatment. Some targeted therapies only help patients with certain genetic markers, so not everyone can benefit. Immunotherapy offers hope, but it is still under study and not yet a standard option.
Many patients need new therapies that work better and cause fewer side effects. Researchers continue to search for solutions that can help more people live longer and healthier lives.
Key limitations of current therapies include:
Ovarian cancer subtypes often do not respond to hormone therapy.
Surgery and chemotherapy may not cure late-stage disease.
Tumors often become resistant to chemotherapy.
Targeted therapies require specific biomarkers.
Immunotherapy is not yet widely available.
New approaches remain in clinical trials.
Aggressive Cancer Types
Some cancer types grow and spread very quickly. These aggressive cancers often lead to poor outcomes. High-grade serous ovarian tumors are the most aggressive form of ovarian cancer. Many women with these tumors survive less than five years after diagnosis. Other ovarian cancer subtypes also show different levels of aggressiveness, which doctors measure by how long patients survive after diagnosis.
Cancer Type | Subtype / Classification | Definition of Aggressiveness | Survival Rate / Outcome |
|---|---|---|---|
Ovarian Cancer | High-grade serous tumors | Most aggressive; worse outcomes | |
Ovarian Cancer | Highly aggressive tumors | Death within 1 year after diagnosis | Poor prognosis |
Ovarian Cancer | Very aggressive tumors | Death within 1 to <3 years | Intermediate prognosis |
Ovarian Cancer | Moderately aggressive tumors | Death within 3 to <5 years | Better prognosis than highly aggressive |
Ovarian Cancer | Less aggressive tumors | Survival beyond 5 years | Best prognosis |
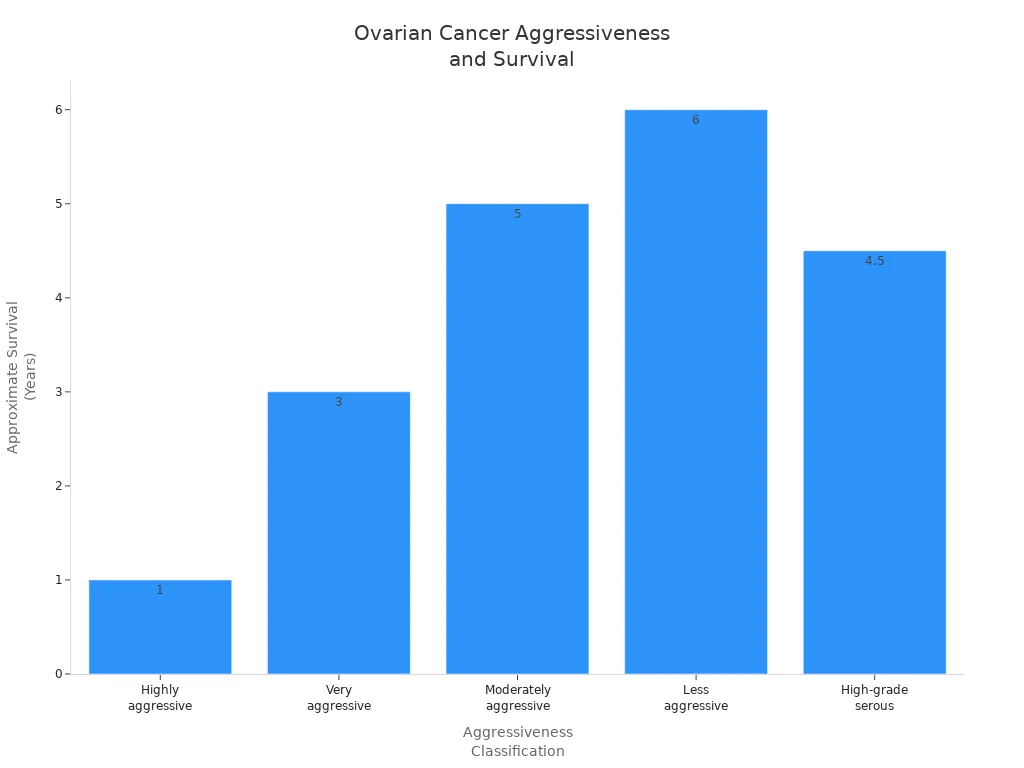
Doctors also know that factors like high body mass index and smoking increase the risk of highly aggressive ovarian cancer. Family history can play a role, too. Some women with a family history of ovarian cancer may respond better to treatment because of certain gene mutations. Researchers continue to study these patterns to find better ways to treat and prevent aggressive cancers.
Melittin Explained
What Is Melittin
Melittin is the main ingredient in honeybee venom. It makes up about half of the venom’s dry weight. This small protein has 26 amino acids and weighs around 2,846 Daltons. Melittin starts as a longer, inactive protein called prepromelittin. The body cuts it down to its active form before it can work.
The structure of melittin is special. The first 20 amino acids are hydrophobic, which means they do not mix with water. The last 6 amino acids are hydrophilic, so they do mix with water. This mix gives melittin both water-loving and water-hating parts, making it amphipathic. When melittin is in water, it looks like a loose coil. When it touches cell membranes, it changes shape and forms an alpha-helix. This shape helps it slip into cell membranes.
Melittin stands out from other honeybee venom peptides. It has a strong positive charge, which helps it stick to cell surfaces. Its unique structure lets it break through cell membranes and cause cell damage. Other peptides in bee venom may have different shapes or targets, but melittin is the most powerful at breaking cells open.
Melittin’s special structure and strong effects make it a focus for cancer research.
How It Targets Cancer
Melittin can attack cancer cells in several ways. Scientists have found that it can target tumors while sparing healthy cells. Here are some ways melittin works:
Melittin can be linked to molecules that find cancer cell markers, such as special receptors on the cell surface. This helps melittin stick to and kill only cancer cells.
Researchers use gene therapy to make melittin inside tumor cells. They use tumor-specific promoters, like the survivin promoter, so only cancer cells make melittin.
Scientists design melittin analogues that keep the cancer-killing power but lower the risk to healthy cells.
Nanoparticles can carry melittin and release it only in tumors. Tumors have leaky blood vessels, so these particles build up there more than in healthy tissue.
Shielding methods, like attaching melittin to polymers, keep it inactive until it reaches the tumor.
Melittin can also boost the immune system in the tumor area, helping immune cells attack cancer.
Some melittin-based treatments target immune cells that help tumors grow, removing them without harming other cells.
These strategies help melittin fight cancer more safely and effectively.
Preclinical Evidence
Lab Results
Scientists have tested melittin and honeybee venom in many laboratory models. These studies show that melittin can kill cancer cells quickly and keep them from growing back. Researchers often use special carriers, like nanoparticles or niosomes, to deliver melittin directly to tumors. This method helps protect healthy cells and lowers side effects.
Melittin causes cancer cells to die by changing important signals inside the cell. It activates death receptors and blocks pathways that help cancer cells survive. Melittin also changes the balance of proteins that control cell death and growth. These actions lead to rapid cell death within hours and lasting effects that can continue for days.
Scientists found that targeted melittin formulations can safely reach tumors and cause strong anti-cancer effects. These results support the idea that honeybee venom cancer research could lead to new treatments.
Study Aspect | Findings |
|---|---|
Apoptosis Induction | Melittin activates death receptors, increases Bax and Caspase 3/9, decreases BCL2 expression |
Signaling Pathways | JAK2/STAT3, AKT, JNK/p38 MAPK pathways involved in cell death |
Mitochondrial Effects | Raises cytochrome C, lowers AIF, promotes mitochondrial apoptosis |
Anti-metastatic Effects | Reduces invasion by lowering MMP-9 and cyclophilin A in breast cancer cells |
Cancer Types Studied | Breast cancer (MCF-7, 4T1), hepatocellular carcinoma, chemo-resistant ovarian carcinoma cells |
Gene Expression Changes | Upregulates Bax, Caspase 3/9, Mfn1; Downregulates BCL2, Drp1, MMP2, MMP9 |
Therapeutic Development | Uses gene-encapsulated pectin and nanotechnology for better delivery |
Combination Therapy | Melittin with chemotherapy (paclitaxel) shows stronger effects |
Breast Cancer Findings
Melittin shows strong effects against breast cancer cells in lab studies. Researchers tested melittin on different breast cancer cell lines, including triple-negative breast cancer, which is hard to treat. Melittin-loaded niosomes stopped cancer cells from growing and caused them to die. These effects happened quickly and lasted for up to a week.
Melittin blocks important signals that help breast cancer cells survive. It suppresses pathways like EGFR, HER2, and PI3K/Akt/mTOR. Melittin also makes cancer cells more sensitive to chemotherapy and radiation. In mouse models, melittin reduced tumor size and stopped cancer from spreading.
Scientists improved safety by using nano-liposomes and other carriers. These new formulations lowered allergic reactions and inflammation. They also helped melittin reach tumors more easily and reduced harm to healthy tissues.
Aspect | Breast Cancer Models |
|---|---|
Efficacy | Tumor growth inhibition, apoptosis induction, suppression of EGFR/HER2/NF-κB/PI3K/Akt/mTOR pathways, radiosensitization |
Safety and Toxicity | Nano-liposomes and nanocarriers reduce toxicity and inflammation, improve targeting |
Mechanistic Insights | Blocks EGF-induced MMP-9, suppresses HER2/EGFR, disrupts HIF-1α signaling, enhances Bax/Bcl-2 ratio |
Formulation Advances | Nano-liposomes and lipid nanoparticles improve delivery and widen safe dose range |
Melittin works quickly and keeps breast cancer cells from growing back. Advanced delivery methods make treatment safer and more effective.
Ovarian Cancer Findings
Ovarian cancer studies are newer but show promising results. In lab tests, melittin stopped ovarian cancer cells from growing, moving, and invading other tissues. Melittin lowered the activity of MMP9 and blocked the JAK2-STAT3 pathway, which helps cancer cells survive and spread.
In animal studies, melittin injections shrank ovarian tumors and reduced harmful proteins in tumor tissues. Melittin caused cancer cells to die by activating death receptors and blocking survival signals. These effects suggest that melittin could help treat ovarian cancer, especially when other treatments fail.
Evidence Type | Description |
|---|---|
In vitro assays | Melittin inhibits proliferation, migration, and invasion of ovarian cancer cells |
Molecular mechanism | Downregulates MMP9, reduces JAK2/STAT3 pathway activity, stable binding to MMP9 and STAT3 |
In vivo animal model | Melittin injections suppress tumor growth and decrease harmful proteins in tumor tissues |
Ovarian cancer research is still in early stages. Scientists need more studies to understand safety and long-term effects. Early results show that melittin may work even better when combined with other parts of honeybee venom.
Melittin shows rapid and lasting effects in ovarian cancer models, but researchers need more data before moving to human trials.
Honeybee Venom Cancer Research
Whole Venom vs. Melittin
Scientists have compared the effects of whole honeybee venom and isolated melittin on cancer cells. Whole venom is a complex mixture. It contains melittin, other peptides like apamin and adolapin, and enzymes such as phospholipase A2. Isolated melittin is a single peptide that makes up about half of the venom’s dry weight. Both forms show strong effects against tumor cells, but they work in different ways.
The table below highlights the main differences:
Aspect | Whole Honeybee Venom (BV) | Isolated Melittin (MEL) |
|---|---|---|
Composition | Complex mix: melittin, peptides, enzymes, other compounds | Single peptide, main source of cytotoxicity |
Cytotoxicity | Strong effects on tumor cells, boosted by synergy between melittin and PLA2 | Strong cytotoxicity via membrane disruption and apoptosis |
Mechanism of Action | Synergy between melittin and PLA2, immune stimulation, other therapeutic effects | Disrupts membranes, induces apoptosis, inhibits cell growth |
Effects on Normal Cells | Less toxic to normal cells than to tumor cells | Less toxic to normal cells than to tumor cells |
Additional Effects | Immune stimulation and possible other benefits | Mainly targets tumor cell membranes and pathways |
Biochemical Interactions | Melittin and PLA2 work together, affecting cell membranes and proteins | Melittin forms aggregates, changes membrane potential, interacts with enzymes |
Researchers have found that the complexity of whole venom may offer extra benefits. The different components can work together, making the venom more effective against cancer cells.
Synergy and Safety
Honeybee venom cancer research has shown that venom and melittin can work with standard cancer drugs. Studies report that melittin boosts the effects of chemotherapy drugs like 5-fluorouracil and doxorubicin. Some experiments also show synergy with drugs used for other conditions, such as fluoxetine and sertraline. These combinations can kill cancer cells more effectively, especially at lower doses. This may help reduce side effects for patients.
However, not all combinations work well. Some mixtures, like doxorubicin with venom, may not always help and could even reduce effectiveness. Scientists stress the need for more studies to understand which combinations are safe and useful.
Safety remains a key concern. While honeybee venom and melittin target cancer cells, researchers must test for possible harm to healthy cells. Most studies so far have taken place in labs or with animals. More research and clinical trials are needed to make sure these treatments are safe for people.
The number of studies on honeybee venom cancer research has grown quickly in the last decade. Scientists continue to explore how the venom’s complex mix of compounds can help fight cancer and improve patient care.
Delivery and Safety
Targeted Formulations
Researchers have developed several advanced delivery systems to help melittin reach cancer cells while protecting healthy tissues. These systems use nanotechnology to carry melittin directly to tumors. This approach increases the treatment’s effectiveness and lowers the risk of side effects.
Description | Example/Mechanism | |
|---|---|---|
Liposomes and Lipid-Coated Nanoparticles | Tiny carriers that combine the benefits of liposomes and nanoparticles. They hold melittin, stay stable in the body, and can circulate longer. | Nanoparticles with a melittin core and special coatings, such as PEG and RGD, help target tumor cells and trigger cell death. |
Stimulus-Responsive Carriers | Nanocarriers that release melittin only when they sense certain triggers in the tumor, like acidity or light. | pH-responsive nanoparticles release melittin in acidic tumors; some systems use light to change shape and deliver the drug. |
Modified Melittin and Conjugates | Scientists change melittin’s structure to make it safer and more stable. | Melittin analogs with small changes reduce harm to red blood cells and improve cancer targeting. |
Co-Delivery Nanoparticles | Nanoparticles that carry melittin with other helpful molecules. | Melittin wrapped with FEGCG forms fluoro-nanoparticles, which lower side effects and boost cancer-fighting power. |
These targeted systems help melittin find and attack cancer cells more precisely. They also allow for controlled release, so the drug works best where it is needed most.
Reducing Toxicity
Melittin can cause side effects, especially haemolysis, which means it breaks down red blood cells. This problem can lead to serious health risks, such as kidney failure or shock. Researchers have found ways to make melittin safer for patients.
Using α-crystallin, a protein from the human eye lens, can block melittin from harming red blood cells.
Removing allergenic parts and histamine from bee venom creates a safer product. Sweet bee venom, which contains melittin, has helped patients with nerve pain from chemotherapy without causing allergic reactions.
Giving melittin in low doses under the skin or into the skin reduces the risk of haemolysis while keeping its cancer-fighting effects.
Nanotechnology, gene therapy, and immunoconjugates help deliver melittin more precisely and lower the chance of harming healthy cells.
Combining bee venom treatments with other drugs, like morphine, can improve pain relief and may allow for lower, safer doses.
Most side effects in studies involve haemolysis, but allergic reactions are rare with pure melittin. New delivery methods and careful dosing continue to make melittin-based therapies safer for future cancer treatments.
Combination Therapies
With Chemotherapy
Doctors often use combination therapies to treat aggressive cancers. Melittin, the main compound in honeybee venom, works well with standard chemotherapy drugs. Scientists have found that melittin can make cancer cells more sensitive to drugs like docetaxel and paclitaxel. This means that lower doses of chemotherapy may still kill cancer cells, which can help reduce side effects for patients.
Researchers have tested melittin with chemotherapy in lab studies. They saw that melittin stopped cancer cells from repairing themselves after chemotherapy. Cancer cells died faster and did not grow back as easily. Melittin also blocked signals that help cancer cells survive, making chemotherapy more effective.
Melittin’s ability to boost chemotherapy gives hope for patients with cancers that do not respond well to treatment. Doctors may use these combinations in the future to help more people.
Benefits of combining melittin with chemotherapy:
Increases cancer cell death
Reduces drug resistance
Lowers needed chemotherapy dose
May cause fewer side effects
Personalized Approaches
Personalized medicine means doctors choose treatments based on each patient’s cancer type and needs. Scientists now design melittin to target certain cancer cells. For example, they add an RGD motif to melittin. This helps melittin find and attack aggressive breast cancer cells, such as HER2-enriched and triple-negative types. Melittin stops these cells from growing by blocking important signals like EGFR and HER2.
Researchers also use polymeric nanoparticles to carry melittin. These tiny carriers deliver melittin right to the tumor. This approach helps protect healthy cells and makes treatment safer. Lab studies show that melittin can kill hard-to-treat cancer cells by disrupting their growth signals. Scientists can make melittin in the lab and change its formula to fit each patient’s needs.
Personalized melittin therapies could give patients better results with fewer side effects. More research will help doctors use these new treatments safely in the future.
Future Prospects
Clinical Trials Path
Researchers see great promise in honeybee venom cancer research, but most results come from lab and animal studies. Before doctors can use these treatments in people, scientists must run careful clinical trials. These trials help show if honeybee venom and melittin are safe and effective for patients with aggressive cancers.
Many natural products, like honeybee venom, have helped create new cancer drugs. Over the years, scientists have found that compounds from plants and animals can fight cancer in different ways. Melittin and phospholipase A2, found in bee venom, can stop cancer cells from growing and even cause them to die. They work by blocking important signals that cancer cells need to survive. Still, honeybee venom cancer research remains in the early stages. Most studies have not moved past the lab or animal testing phase.
Clinical trials will help answer important questions about the best dose, how to give the treatment, and which patients will benefit most. These steps are key before honeybee venom-based therapies can become approved cancer drugs.
Research Challenges
Scientists face several challenges as they try to turn honeybee venom into a real cancer treatment. One big problem is making sure the treatment does not harm healthy cells. Melittin can cause side effects like breaking down red blood cells and hurting the liver. Researchers work to solve these problems by using new delivery systems, such as nanoparticles and special carriers, to target tumors more safely.
Other challenges include:
Not enough studies in living animals to test safety and the best way to give the treatment.
Limited knowledge about how bee venom affects the immune system, especially for skin cancer.
The need to lower toxicity and avoid harming healthy tissues.
Making sure the treatment works well with other cancer drugs.
Scientists now focus on linking melittin to molecules that find cancer cells, using nanotechnology, and combining it with other treatments. These steps may help overcome drug resistance and improve results for patients. Natural products like honeybee venom continue to inspire new ideas in cancer therapy, but more research and clinical trials are needed before these treatments can help people.
Honeybee venom cancer research offers new hope for patients with aggressive cancers. Melittin shows strong effects against tumor cells in laboratory studies. Safety remains important for patients and clinicians.
Qualified professionals must monitor patients for reactions.
Standardized preparations help ensure safety.
Ongoing research and clinical trials will guide future therapies. People can stay hopeful as scientists explore new options.
FAQ
What is melittin and where does it come from?
Melittin is a small protein found in honeybee venom. Scientists study melittin because it can attack cancer cells. Bees make melittin as part of their natural defense.
Can honeybee venom cure cancer?
Honeybee venom does not cure cancer. Researchers test it in labs to see if it helps fight cancer cells. Doctors need more studies before using it as a treatment.
Is melittin safe for healthy cells?
Melittin targets cancer cells more than healthy cells. Some side effects can happen, like breaking red blood cells. Scientists use special carriers to make melittin safer.
How do doctors give melittin to patients?
Doctors do not use melittin in hospitals yet. Researchers test melittin in animals and lab models. They use nanoparticles and other carriers to deliver melittin to tumors.
#BanishCancer
See Also
Recognizing Symptoms And Treatment Options For Duodenal Cancer
An Overview Of Invasive Ductal Carcinoma And Symptoms
Different Cancer Types Commonly Associated With AIDS Diagnosis
Understanding Invasive Cribriform Breast Carcinoma Explained Clearly

