Why Wearable Devices Matter for Early Cancer Diagnosis

Wearable devices matter for early cancer diagnosis because they can spot small changes in the body before symptoms show. Researchers at MIT created a wearable ultrasound scanner that helps find breast cancer early. Early detection means almost every patient survives, while late detection drops survival to about 25%. New digital sensors and AI help doctors track and treat cancer more quickly. The Impact of Wearable Devices on Early Cancer Diagnosis shows that these tools save lives by giving patients a better chance for recovery.
Key Takeaways
Wearable devices track small body changes that help detect cancer early, improving chances of survival.
Different wearables collect data like activity, heart rate, and biochemical markers to spot cancer signs before symptoms appear.
Continuous monitoring and AI analysis allow doctors to catch problems sooner and personalize cancer care.
Challenges include device accuracy, privacy concerns, and making wearables affordable and easy to use for everyone.
Building trust, protecting data, and ensuring fair access are essential to help more people benefit from wearable cancer detection.
How Wearables Detect Cancer

Types of Devices
Wearable devices come in many forms. Each type has unique features that help with cancer detection and care. The table below shows some common types and their uses:
Type of Wearable Device | Unique Features | Application in Cancer Detection and Care |
|---|---|---|
Consumer-grade activity monitors | Measure physical activity, sleep, and vital signs with high temporal granularity | Used to monitor patient performance status, fatigue, and indirect effects of cancer therapy |
Implantables | Provide continuous biochemical analyte monitoring in blood plasma or interstitial fluid | Offer real-time biochemical data potentially useful for early detection and monitoring of cancer-related physiological changes |
Microneedle patches | Minimally invasive, continuous sampling of biochemical analytes in interstitial fluid | Enable real-time monitoring of systemic biochemistry, contributing to digital phenotyping and personalized oncology |
Consumer devices like Fitbit and Apple Watch track health metrics such as activity and heart rate. These devices give doctors and patients a steady stream of information, not just snapshots during clinic visits. Some research labs have developed wearable ultrasound scanners, like the continuous Ultrasound Breast Monitor (cUSBr). This device uses special sensors to find small changes in breast tissue. Other wearables use flexible antennas or microwave imaging to spot differences between healthy and cancerous tissues. Non-invasive sensors can also check sweat, saliva, or breath for cancer-related molecules.
Data Collected
Wearable devices collect many types of data that can help with early cancer detection. Some of the most common data include:
Heart rate and heart rate variability
Gait and walking patterns
Sleep quality and duration
Skin temperature
Body composition and weight changes
Biochemical markers in sweat, saliva, or tears, like proteins and hormones
Most current wearables focus on tracking physical activity and vital signs. Newer devices can check for molecular markers in body fluids. These markers may show up before a person feels sick. For example, sweat sensors can find proteins or chemicals linked to cancer. This technology is still growing, but it could soon help doctors spot cancer even earlier.
Early Warning Signs
Wearable devices can pick up early warning signs of cancer before a person notices symptoms. They do this by watching for small changes in the body. Some examples include:
Hoarseness or voice changes, which can point to head, neck, or lung cancers
Less physical activity, which may mean fatigue from cancer
Skin or eye color changes, which can show anemia or jaundice
New or changing skin spots, which may be signs of skin cancer
Higher body temperature, which can happen with some cancers
Unexplained weight loss, which can be a warning sign
Anemia, found through signals in the blood
Wearable devices can alert users and doctors to these changes. For example, a smart bra with microwave sensors can find small lumps in breast tissue. Some devices use artificial intelligence to spot patterns in the data. These patterns may show up months before a person feels sick. Early alerts give people a chance to see a doctor sooner and start treatment earlier.
Continuous monitoring helps catch these changes quickly. Doctors and patients can act before the cancer grows or spreads. This makes wearable devices a powerful tool for early cancer detection.
The Impact of Wearable Devices on Early Cancer Diagnosis

Real-World Evidence
The Impact of Wearable Devices on Early Cancer Diagnosis can be seen in many real-life situations. Doctors and researchers have used wearable devices to track patient health and spot cancer sooner. For example, some hospitals use smartwatches to monitor heart rate, sleep, and activity in cancer patients. These devices help doctors notice changes that might signal a problem before symptoms appear.
Studies show that lower step counts on wearables often match up with pain, depression, or lower physical health in cancer patients. When doctors see these changes, they can act quickly to help the patient. Wearable sensors also track sleep patterns and movement. This information helps doctors find patients who might not respond well to treatment. By catching these signs early, doctors can adjust care plans and improve outcomes.
Wearable devices also help with real-time biomarker detection. For example, some patches can measure C-reactive protein in sweat. High levels of this protein may mean inflammation or cancer growth. Doctors use this data to check how well treatments work and to spot problems early. Tumor monitoring with wearable strain sensors gives doctors a way to watch tumor growth or shrinkage without extra scans.
Real-world use of wearables gives patients and doctors a new way to fight cancer. Early alerts and continuous data help save lives by making sure problems get noticed right away.
Technology Integration
The Impact of Wearable Devices on Early Cancer Diagnosis grows even stronger when technology like artificial intelligence (AI) and digital health systems join the process. AI-based wearable biosensors use machine learning to find cancer markers in body fluids, such as urine or sweat. Some devices use random forest and neural network models to detect prostate cancer with over 99% accuracy. These smart sensors can also find volatile organic compounds in breath, which helps spot lung and stomach cancers early.
AI models improve how well sensors pick up cancer signals, making them more sensitive and selective.
Deep learning tools, like convolutional and recurrent neural networks, help predict diseases quickly. For example, some wearables can detect illness within 24 hours.
AI helps wearable devices track signals like pulse and heart rate. This makes the data more accurate and useful for doctors.
Wearable strain sensors with nanoparticles can watch tumors grow or shrink. This helps doctors plan treatments better.
Wearable devices collect many types of data, such as heart rate, temperature, movement, and chemical markers. AI looks at this data to find patterns and predict what might happen next. For example, AI can tell if a patient might not handle chemotherapy well or if they are at risk for frailty. Doctors use this information to make better treatment plans.
Data from wearables can go straight into electronic health records. This lets doctors and AI systems work together to give each patient the best care.
AI also helps patients stick to their treatment plans by tracking medicine use and diet through wearables.
Real-time monitoring means doctors can catch problems early and act fast.
The Impact of Wearable Devices on Early Cancer Diagnosis depends on how well these tools work with AI and digital health systems. When all these parts work together, patients get more personalized care, and doctors make better decisions. Continuous monitoring and smart analysis give everyone a better chance to catch cancer early and treat it more effectively.
Benefits
Continuous Monitoring
Wearable devices give people the power to track their health every day. These tools collect data all the time, not just during doctor visits. Many cancer survivors use wrist-worn devices like fitness trackers and smartwatches. Fitbit is one of the most common brands. Doctors can see daily step counts and other health signs. In lung cancer, lower step counts can show a worse outlook. Continuous data helps spot health problems early, sometimes before a person feels sick.
Aspect | Evidence Summary |
|---|---|
Proportion of studies monitoring cancer | 7 out of 68 studies (10%) focused on cancer among existing disease monitoring studies |
Device types used | Mostly consumer-grade wrist-worn devices (fitness trackers, smartwatches), with Fitbit being the most common brand |
Documented benefits | Potential for continuous monitoring of health parameters in cancer survivors; daily step counts linked to prognosis in lung cancer; early detection of health anomalies possible due to continuous data collection |
Clinical evidence strength | Limited; few randomized controlled trials and scarce reporting on cancer-specific clinical outcomes |
Challenges noted | Inconsistent reporting, low patient compliance, lack of technical support, usability issues, privacy concerns |
Patient engagement | Critical for success; many studies lack data on device instruction, technical support, and usability feedback |
Overall conclusion | Evidence for continuous health monitoring benefits in cancer risk is emerging but remains limited and not yet robustly documented |
Continuous monitoring helps people and doctors notice small changes. Early action can make a big difference in cancer care.
Early Alerts
Wearable devices can send alerts when they find unusual patterns. These early warnings help people see a doctor before symptoms get worse. For example, a sudden drop in activity or a change in sleep can signal a problem. Doctors can use this information to check for cancer or other health issues. Early alerts give patients a better chance to start treatment sooner.
Early alerts can lead to faster diagnosis.
Doctors can adjust care plans quickly.
Patients feel more in control of their health.
Personalized Care
Wearable technology supports care that fits each person. Scientists at UVA Cancer Center use smartwatches and smartphones to track hormone levels like cortisol. High cortisol can affect tumor growth in pancreatic cancer. By combining wearable data with tumor models, doctors learn how each patient’s cancer behaves. Artificial intelligence can study this data and help doctors choose the best treatments.
Personalized care means doctors treat each patient based on their unique needs. Wearables make this possible by giving real-time data about the body and behavior.
Wearable devices help people manage their health, catch problems early, and get care that matches their needs. These benefits can lead to better outcomes and more confident patients.
Challenges
Accuracy
Wearable devices for cancer detection face several accuracy challenges. Many devices only measure one vital sign, such as temperature, which limits their ability to detect cancer early. Clinical definitions, like what counts as a fever, can vary between hospitals. This makes it hard to compare results. Devices often lack standard protocols for use in clinics. Some symptoms, like pain or tiredness, are hard to measure with sensors. Most devices do not have FDA approval, so doctors may not trust the results. Data from wearables can be hard to combine with hospital records. Patients sometimes stop using the devices, especially when they feel sick.
Devices often measure only one sign, like temperature.
Hospitals use different rules for symptoms.
No standard way to use devices in clinics.
Hard to measure pain and fatigue with sensors.
Few devices have FDA approval.
Data may not fit with hospital systems.
Patients may not always use the devices.
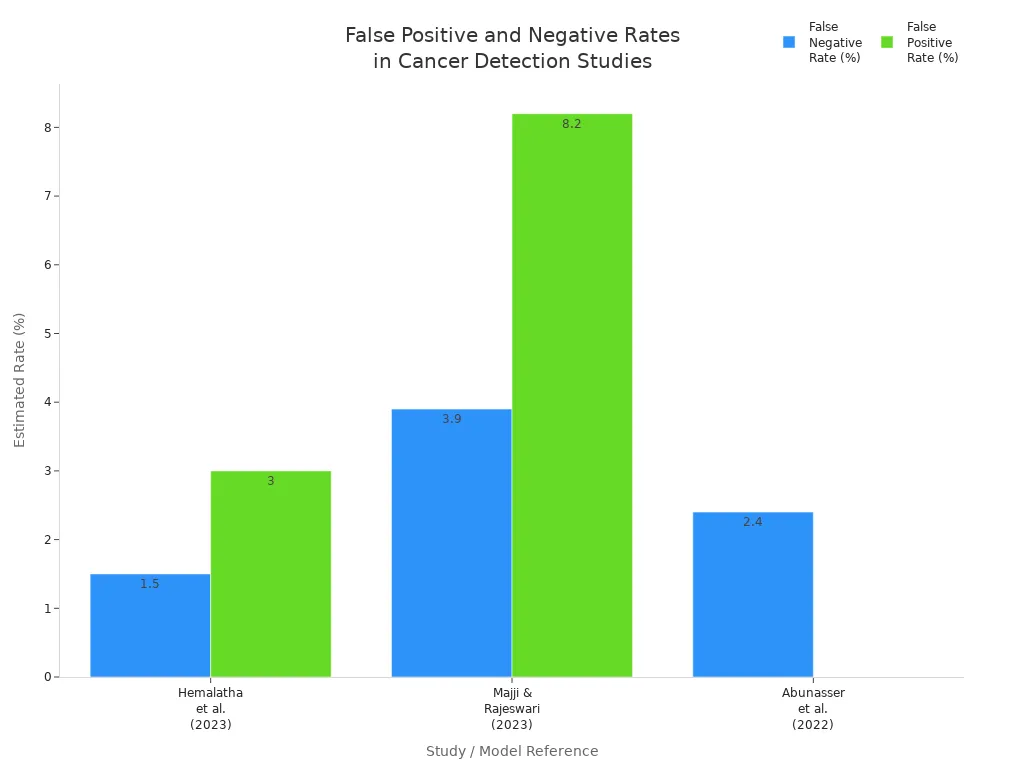
Researchers work to solve these problems. They train patients and doctors, use AI to measure symptoms, and try to make devices track more signs. Some devices now use deep learning to improve accuracy. The table below shows how well some devices perform:
Study / Model Reference | Sensitivity (Recall) | Specificity | Precision | Accuracy | Notes on False Positives/Negatives |
|---|---|---|---|---|---|
Hemalatha et al. (2023) | 97% | N/A | 98.2% | Low false negatives and false positives | |
Majji & Rajeswari (2023) | 96.10% | 91.80% | N/A | 91.56% | High true positive rate, low false negatives |
Abunasser et al. (2022) | 97.60% | N/A | 97.60% | N/A | Balanced low false negatives and positives |
Smart Bra Studies | N/A | N/A | N/A | N/A | More errors without deep learning |
Privacy
Privacy remains a major concern for people using wearable devices. Some cancer survivors feel comfortable sharing their health data to help others. Others worry about who can see or use their information. Risks include companies selling data to third parties or insurance companies. Even when data is anonymous, it can sometimes be traced back to a person. Many devices do not fall under strict health privacy laws, so there are fewer protections. Most people want to know how their data will be used and who will see it. Trust in the company or doctor collecting the data matters a lot.
People often balance the benefits of early cancer detection with the risks of sharing private health information.
Accessibility
Not everyone can use wearable devices for cancer detection. Cost is a big barrier. Many people cannot afford these devices. Some devices are hard to use or do not give feedback quickly. Wearables are mostly used in research, not in regular clinics. People with lower incomes or less experience with technology use wearables less often. Black and Hispanic groups, older adults, and those with less digital skill face more barriers. Devices may not work as well for people with darker skin tones. These gaps can lead to unfair differences in who benefits from early cancer detection.
Cost and affordability limit access.
User-friendliness and feedback matter for adoption.
Older adults and those with less digital skill face more challenges.
Devices may be less accurate for some skin tones.
Policymakers and health leaders need to plan ways to make wearable cancer detection fair and available to everyone.
Ethics and Equity
Data Security
Wearable devices collect sensitive health information. This data can include details about cancer risk or diagnosis. Several risks threaten the security of this information:
Hackers can access data sent over wireless or Bluetooth connections if encryption is weak.
Companies that make wearables may own the data and sometimes share or sell it, even if it is anonymized. Sometimes, people can be identified from this data.
Patients often do not know where their data is stored or who can see it. Different countries have different privacy laws, which can make protection harder.
Cybersecurity for wearables is not as strong as in banks or other industries. This makes health data a target for hackers.
Health data, if shared without consent, could lead to discrimination by employers or insurers.
Many people want control over their health data and worry about privacy. However, privacy policies are often hard to understand, and users may not realize how their data is used.
To protect data, experts recommend several best practices:
Encrypt all data, both when stored and when sent.
Use strong passwords and multi-factor authentication.
Regularly check devices and networks for suspicious activity.
Update software to fix security problems.
Follow rules set by groups like the FDA and international standards.
User Trust
Trust plays a big role in whether people use wearable devices for cancer monitoring. People want to know that their data is safe and that the device works well. Several factors shape this trust:
Factor | Description | Influence on Trust and Use |
|---|---|---|
People trust devices from companies with a good reputation. | Strongly increases trust | |
Perceived Security | Users feel safer when they know their data is protected. | Increases trust |
Perceived Privacy | If people think their data might be misused, they trust less. | Lowers trust |
Trust Propensity | Some people naturally trust technology more than others. | Shapes initial trust |
Risk-Benefit Analysis | Users weigh the benefits of early cancer detection against privacy risks. | Affects willingness to use |
Cultural Differences | Trust levels can change based on culture and background. | Changes trust and use |
Surveys show that many people, especially older adults, hesitate to share their wearable data. Clear and simple data policies help build trust and encourage more people to use these devices.
Health Equity
Not everyone has the same chance to benefit from wearable cancer detection. Barriers include cost, access to technology, and digital skills. People with lower incomes, less education, or who are older often use wearables less. Even when people own devices, many do not use them regularly.
Most wearables are bought by individuals, making them less available to disadvantaged groups.
The digital divide means some groups, such as racial and ethnic minorities, have less access to these tools.
Training and easier-to-use devices can help more people benefit.
Several programs aim to close these gaps:
Community-based screening brings devices to places like churches and community centers.
Telemedicine and virtual visits help people in rural areas see cancer specialists.
Some groups work to improve broadband access, so more people can use digital health tools.
Involving diverse patients in device design helps make wearables more useful for everyone.
Making wearable cancer detection fair means investing in access, education, and trust. When everyone can use these tools, early cancer diagnosis becomes possible for all.
Wearable devices offer hope for early cancer diagnosis by tracking health changes in real time. Studies show these tools help people stay active and may spot problems sooner, but strong proof for better survival remains limited. Experts see promise in new biosensors, AI-powered analysis, and more comfortable designs. Challenges include making devices easy to use, protecting data, and reaching everyone, no matter their background.
The future looks bright as technology advances and care becomes more personal. With continued research and fair access, wearables could help save more lives from cancer.
FAQ
What types of cancer can wearable devices help detect?
Wearable devices can help detect several types of cancer. These include breast, lung, skin, and some blood cancers. Devices look for changes in the body that may signal early cancer growth.
Are wearable devices safe to use every day?
Most wearable devices use safe materials and low-power sensors. Doctors and researchers test these devices before use. People can wear them daily without harm.
How accurate are wearable devices for early cancer detection?
Accuracy depends on the device and the type of cancer. Some devices use advanced sensors and AI to improve results. Doctors still use other tests to confirm any findings.
Who can benefit most from wearable cancer detection?
People with a family history of cancer or those at higher risk may benefit most. Wearables also help patients who want to track their health closely.
Do wearable devices replace regular cancer screenings?
Wearable devices do not replace regular screenings. Doctors use them as extra tools. People should still visit their doctor for check-ups and follow medical advice.
See Also
Recognizing Key Symptoms And Causes Of Esophageal Cancer
A Detailed Look At Symptoms And Treatments For Duodenal Cancer
Identifying The Symptoms And Causes Of Laryngeal Cancer

