Understanding Intravascular Large B-Cell Lymphoma and Its Key Features
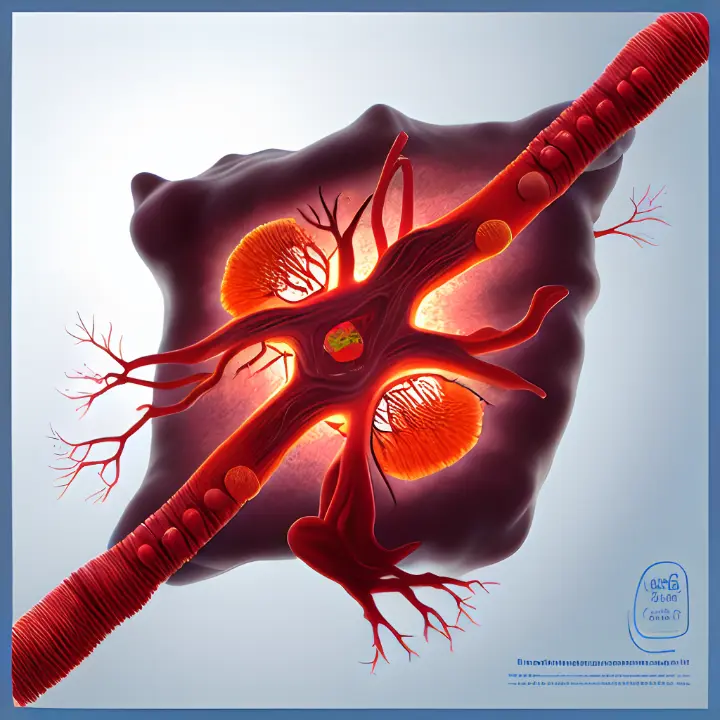
Intravascular large B-cell lymphoma is a rare and aggressive form of B-cell non-Hodgkin lymphoma. Its global incidence rate is less than 1 person per million, making it an uncommon condition. What sets this lymphoma apart is the unusual growth of tumor cells inside small and medium-sized blood vessels. Unlike other lymphomas, it does not typically involve lymph nodes or peripheral blood.
Symptoms often appear vague and depend on the affected organs. These may include fever, skin lesions, or neurological issues. Early diagnosis is crucial because of its rapid progression and nonspecific signs. Recognizing these unique features can help you understand the urgency of seeking medical attention.
Key Takeaways
Intravascular large B-cell lymphoma (IVLBCL) is a rare cancer. It mainly affects small blood vessels and causes unusual symptoms like nerve problems and skin changes.
Spotting unclear symptoms like fever, skin spots, or nerve issues is key. Early diagnosis can make treatment work much better.
Doctors use biopsies, especially random skin biopsies, to find IVLBCL. Scans and lab tests also help confirm the disease.
Chemotherapy, mainly the R-CHOP plan, is the main treatment. New targeted treatments may help people live longer.
Knowing the symptoms and seeing a doctor quickly can help. Early detection makes managing IVLBCL easier and more effective.
Clinical Features of Intravascular Large B-Cell Lymphoma

Neurological Symptoms
Neurological symptoms are among the most common and severe features of intravascular large B-cell lymphoma. You may experience sensory or motor deficits, such as weakness or numbness in specific areas. Other symptoms include paresthesias, hemiparesis, or even seizures. Some individuals report transient visual loss, vertigo, or difficulty speaking, such as aphasia or dysarthria. In advanced cases, you might notice altered consciousness or myoclonus. These symptoms often result from vascular occlusion or multiple infarct sites in the brain.
The progression of neurological symptoms can be rapid and aggressive. Without early diagnosis, these issues may worsen, leading to a poor prognosis. Diagnosing neurological involvement in IVLBCL can be challenging due to its nonspecific nature. However, recognizing these signs early can significantly improve outcomes.
Skin Manifestations
Skin changes are another hallmark of intravascular large B-cell lymphoma. You might notice firm nodules, plaques, or masses under the skin. These can appear as painful, red, or blue discolorations. In some cases, the skin may develop ulcerated nodules, palpable purpura, or small red spots. These lesions often feel indurated or thickened, resembling an "orange peel" texture.
Interestingly, a specific form of IVLBCL, known as the "cutaneous variant," involves skin lesions without systemic symptoms. This variant has a better prognosis, with a three-year survival rate of 56%. However, if the disease spreads beyond the skin, survival rates drop significantly. Paying attention to unusual skin changes can help in early detection.
Systemic Symptoms
Systemic symptoms of intravascular large B-cell lymphoma often overlap with other conditions, making diagnosis difficult. You may experience fever, fatigue, or unexplained weight loss. Other common signs include anemia, malaise, and gastrointestinal or urinary symptoms. Some individuals report pain due to abdominal or cutaneous involvement.
The nonspecific nature of these symptoms can complicate diagnosis. For example, fever and neurological signs may mimic infections or autoimmune diseases. Recognizing the combination of systemic, neurological, and skin symptoms is crucial for identifying IVLBCL early.
Variability in Presentation
The presentation of intravascular large B-cell lymphoma varies widely, making it a challenging condition to diagnose. You may notice that symptoms differ based on geographic location and the specific organs affected. For example:
In Western countries, neurological and skin symptoms are more common.
In Asian countries, patients often present with hemophagocytic syndrome, a severe immune response that can cause fever, anemia, and organ dysfunction.
This variability stems from the disease's impact on small blood vessels, which can lead to organ dysfunction. Symptoms like fever, cutaneous lesions, and neurological signs often dominate. However, other signs such as hepatosplenomegaly (enlarged liver and spleen) or gastrointestinal issues may also appear.
The nonspecific nature of these symptoms complicates the diagnostic process. You might experience fever, fatigue, or weight loss, which could mimic other conditions. In fact, studies show that 91% of patients are diagnosed at advanced stages (stage III or IV). Common symptoms include:
Fever (45%)
Skin symptoms (39%)
Neurological issues (34%)
Pain from abdominal or skin involvement (21%)
Fatigue (16%)
Weight loss without fever (11%)
Less common signs include gastrointestinal or urinary symptoms, cardiac dysfunction, and dyspnea. These diverse presentations highlight the importance of recognizing patterns. For instance, a combination of fever, neurological symptoms, and skin changes should raise suspicion for this condition.
The variability in presentation underscores the need for early and accurate diagnosis. You can improve outcomes by seeking medical attention promptly if you notice unusual or persistent symptoms. Understanding these patterns can help you and your healthcare provider identify intravascular large B-cell lymphoma earlier, potentially leading to better treatment results.
Diagnosis of Intravascular Large B-Cell Lymphoma
Biopsy Techniques
Biopsy remains the cornerstone for diagnosing intravascular large B-cell lymphoma. Among the available methods, random skin biopsy (RSB) stands out as a low-risk and effective diagnostic tool. It offers a sensitivity of 78% and a specificity of approximately 99%. This technique involves sampling skin tissue, often from areas without visible lesions, to detect lymphoma cells within blood vessels.
Biopsy Technique | Sensitivity | Specificity |
|---|---|---|
Random Skin Biopsy (RSB) | 78% | ~99% |
Incisional Biopsy | N/A | N/A |
Incisional biopsy is another option, particularly when it includes subcutaneous fat. However, false negatives can occur. To improve accuracy, you should inform the pathologist to look for subtle lymphocyte aggregates. Multiple biopsies from suspicious sites are often recommended to enhance diagnostic precision.
Imaging Studies
Imaging studies play a supportive role in diagnosing intravascular large B-cell lymphoma. Magnetic resonance imaging (MRI) can reveal contrast-enhanced lesions, which may resemble other conditions like toxoplasmosis. Additionally, 18F-FDG PET/CT is highly valuable for both initial diagnosis and monitoring treatment response. This imaging modality helps identify areas of abnormal metabolic activity, which are often indicative of lymphoma.
MRI: Useful for detecting contrast-enhanced lesions.
18F-FDG PET/CT: Effective for diagnosis and tracking treatment progress.
Despite their utility, imaging studies alone often fail to confirm the diagnosis due to the absence of solid tumors. For this reason, combining imaging with biopsy techniques is crucial for accurate detection.
Laboratory Tests
Laboratory tests provide additional insights into the nature of the disease. Genetic testing can identify specific genetic characteristics of lymphoma cells, aiding in diagnosis. Immunophenotyping is another essential test. It determines the expression of markers like CD79a, CD19, and CD20 on malignant lymphocytes, confirming the presence of intravascular large B-cell lymphoma.
Test Type | Description |
|---|---|
Genetic testing | Identifies specific genetic characteristics of lymphoma cells. |
Immunophenotyping | Determines the immunophenotypic expression of malignant lymphocytes, including markers like CD79a, CD19, and CD20. |
These tests, combined with biopsy and imaging, form a comprehensive approach to diagnosing this rare and aggressive lymphoma. Early and accurate diagnosis can significantly improve treatment outcomes.
Treatment Options for Intravascular Large B-Cell Lymphoma
Chemotherapy
Chemotherapy forms the backbone of treatment for intravascular large B-cell lymphoma. Combination regimens like CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and CHOP-like therapies have shown promising results. Anthracycline-based treatments, in particular, improve remission rates and survival outcomes. Adding rituximab, a monoclonal antibody, to these regimens further enhances their effectiveness.
The R-CHOP regimen, which combines rituximab with CHOP, is the most widely used chemoimmunotherapy for this condition. Studies reveal that R-CHOP achieves a 2-year overall survival rate of 66% and a 3-year overall survival rate of 81%. These statistics highlight the importance of early and aggressive chemotherapy in managing this aggressive lymphoma.
💡 Tip: If you or a loved one is undergoing chemotherapy, staying informed about potential side effects and discussing them with your healthcare provider can help manage the treatment process effectively.
Targeted Therapies
Targeted therapies offer a more precise approach to treating intravascular large B-cell lymphoma. The MATRIX regimen, which combines chemotherapy with targeted therapy, has shown significant promise. Patients treated with this regimen achieved a complete remission rate of 49% at a median follow-up of 30 months. This is a notable improvement compared to methotrexate-cytarabine alone (23%) or methotrexate-cytarabine plus rituximab (30%).
The MATRIX regimen also improves overall survival rates, making it a valuable option for patients who may not respond well to standard chemotherapy. These therapies target specific molecules involved in the growth and survival of lymphoma cells, offering a tailored treatment approach.
Supportive Care
Supportive care plays a crucial role in managing the symptoms and side effects of treatment. You may require medications to control nausea, pain, or infections during chemotherapy. Blood transfusions or growth factors might be necessary to address anemia or low white blood cell counts.
Psychological support is equally important. Coping with a rare and aggressive condition like intravascular large B-cell lymphoma can be emotionally challenging. Counseling or support groups can provide valuable emotional and mental health support.
🩺 Note: Regular follow-ups and open communication with your healthcare team ensure that your treatment plan remains effective and tailored to your needs.
Prognosis of Intravascular Large B-Cell Lymphoma
Survival Rates and Influencing Factors
Survival rates for intravascular large B-cell lymphoma vary significantly based on treatment and disease progression. Without treatment, the median survival is only five months. Patients receiving anthracycline-based chemotherapy, such as R-CHOP, have a mean survival of 13 months. High-dose chemotherapy combined with autologous stem cell transplantation has shown promising results. Among seven patients treated with this approach, five remained relapse-free after follow-ups ranging from 10.5 to 95.5 months.
Geographic differences also influence survival outcomes. In Japan and Europe, the two-year overall survival (OS) rate is 66%, with a three-year OS of 81%. However, in North America, the three-year OS is lower, at 42.7%. Factors such as age over 60, thrombocytopenia, and lack of anthracycline therapy negatively impact prognosis.
Factor | Influence on Prognosis |
|---|---|
Age over 60 years | Poor prognosis |
Thrombocytopenia | Poor prognosis |
Lack of anthracycline therapy | Poor prognosis |
Challenges in Prognosis
Diagnosing intravascular large B-cell lymphoma early remains a significant challenge. The disease often presents with nonspecific symptoms, making it difficult to identify before advanced stages. In many cases, a definitive diagnosis occurs postmortem. The wide range of clinical features, including neurological, skin, and systemic symptoms, complicates early detection.
Delays in diagnosis often lead to a fatal outcome. Late-stage diagnosis reduces the effectiveness of treatment and worsens survival rates. Early recognition of symptoms and prompt medical evaluation are critical for improving outcomes.
Advances in Research and Early Detection
Recent advancements in research have improved early detection methods. The classification of intravascular large B-cell lymphoma into three types—classical, cutaneous, and hemophagocytic syndrome-associated—has enhanced diagnostic accuracy. Improved imaging techniques, such as post-contrast 3D black blood Cube MRI, now reveal lesions more effectively than conventional methods. These advancements help detect the disease earlier, especially in the cutaneous variant, which has a better prognosis.
Ongoing research continues to refine diagnostic tools and treatment strategies. Early detection remains the key to improving survival rates and quality of life for patients.
Intravascular large B-cell lymphoma (IVLBCL) is a rare but aggressive disease that demands early diagnosis and immediate treatment. You must stay vigilant about its nonspecific symptoms, such as neurological issues, skin changes, or unexplained fever. Raising awareness among patients and healthcare providers can lead to faster recognition and better outcomes.
🧬 Hope for the Future: Advancements in research and treatment, including targeted therapies and improved diagnostic tools, offer new possibilities. These developments bring hope for better survival rates and quality of life for those affected by this challenging condition.
FAQ
What makes intravascular large B-cell lymphoma different from other lymphomas?
IVLBCL grows inside small blood vessels instead of lymph nodes. This unique feature causes symptoms based on the affected organs, such as neurological issues or skin changes. Early detection is crucial due to its aggressive nature.
Can IVLBCL be cured?
Treatment can lead to remission, especially with early diagnosis. Chemotherapy, like the R-CHOP regimen, and targeted therapies improve survival rates. However, outcomes depend on factors like age, stage at diagnosis, and treatment response.
💡 Tip: Regular follow-ups and adherence to treatment plans improve your chances of better outcomes.
How is IVLBCL diagnosed if symptoms are nonspecific?
Doctors use a combination of random skin biopsies, imaging studies like PET/CT scans, and laboratory tests. These methods help confirm the presence of lymphoma cells in blood vessels, even when symptoms are vague.
Who is most at risk for developing IVLBCL?
This condition primarily affects adults over 60. Risk factors include age, geographic location, and possibly genetic predispositions. It is rare, so awareness of symptoms is vital for early detection.
What should you do if you suspect IVLBCL?
Seek medical attention immediately if you notice unexplained neurological issues, skin changes, or persistent fever. Early evaluation by a specialist can lead to faster diagnosis and treatment.
🩺 Note: Always share detailed symptom information with your doctor to aid in accurate diagnosis.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
A Comprehensive Guide To Diffuse Large B-Cell Lymphoma
Simplifying The Basics Of B-Cell Prolymphocytic Leukemia
Anaplastic Large Cell Lymphoma: Definition And Treatment Options

