Invasive Lobular Carcinoma Incidence and Detection Trends in 2025

You may notice that more women now receive a diagnosis of invasive lobular carcinoma (ILC) than ever before. In 2025, experts expect about 33,600 new cases in the U.S. alone. ILC makes up over 10% of all breast cancers and now ranks as the seventh-most common cancer in women. You should know that ILC grows in a linear or scattered pattern, which makes it harder for doctors to find early. White women have the highest rates, but Asian American and Pacific Islander women show the fastest rise in cases. These trends make it urgent for you and your healthcare team to seek better ways to detect and treat ILC.
Key Takeaways
Invasive lobular carcinoma (ILC) cases are rising, with an expected 33,600 new diagnoses in the U.S. in 2025. Awareness of this trend is crucial for early detection and treatment.
ILC often grows in a unique pattern that makes it harder to detect early. Regular screenings and discussions with your doctor about risk factors are essential for those at higher risk.
Most ILC tumors respond well to hormone therapy, especially aromatase inhibitors. Discuss treatment options with your doctor to find the best approach for your situation.
Research on ILC is limited, leading to gaps in treatment guidelines. Participating in clinical trials can help advance knowledge and improve outcomes for future patients.
ILC Incidence Trends
2025 Case Numbers
You see more people diagnosed with invasive lobular carcinoma (ILC) every year. In 2025, doctors expect about 33,600 new cases in the United States. This number shows a steady increase compared to previous years. ILC now makes up between 10% and 15% of all breast cancer cases. Most patients with ILC are women over the age of 70. You notice that people living in cities or areas with low poverty have higher rates of ILC. If you look at the numbers, you find that ILC affects a wide range of women, but some groups show faster growth than others.
Demographic Patterns
You may wonder which groups have the highest risk for invasive lobular carcinoma (ILC). The highest rates appear in non-Hispanic White women. You also see significant increases among non-Hispanic Black women and Hispanic women. The fastest rise in cases happens in Hispanic women, especially in recent years. People older than 70 and those living in metropolitan areas face the greatest risk. If you look at the data from a large study of over 200,000 patients, you find these racial and ethnic breakdowns:
84% White
7.8% Black
4.4% Hispanic
0.7% East Asian
2.2% other groups
You should know that patients with low socioeconomic status have a 24% higher risk of death within five years compared to those with higher status. This fact shows that where you live and your income can affect your health outcomes with ILC.
Tip: If you belong to a group with rising rates, talk to your doctor about screening and risk factors.
Comparison to Other Subtypes
You may ask how invasive lobular carcinoma (ILC) compares to other breast cancer types. The most common type is invasive ductal carcinoma (IDC). You can see the difference in the table below:
Cancer Type | Incidence Rate (%) |
|---|---|
Invasive Lobular Carcinoma (ILC) | |
Invasive Ductal Carcinoma (IDC) | 85-90 |
IDC makes up most breast cancer cases, but ILC is rising faster in many groups. You need to know that ILC has unique features and challenges, so doctors must pay special attention to these trends.
ILC in Cancer Statistics
Cancer Ranking
You may wonder where invasive lobular carcinoma (ILC) stands among other cancers. ILC now ranks as the seventh-most common cancer in women in the United States. You see this type of breast cancer making up more than 10% of all breast cancer cases. Most people with ILC are women over 70 years old. You notice that ILC is rising faster than many other cancer types. This trend means you need to pay attention to changes in cancer statistics. Doctors and researchers use these rankings to decide which cancers need more study and better treatments.
Note: Cancer rankings help guide funding and research priorities. When a cancer moves up in rank, it often gets more attention from scientists and health organizations.
Research Representation
You may think that all breast cancers get equal attention in research. In reality, invasive lobular carcinoma (ILC) does not appear as often in major cancer registries and research databases. Many databases, like those at the Breast Center at Baylor College of Medicine, do not break down ILC into smaller subtypes. If you have mixed ILC and invasive ductal carcinoma (IDC), you may not get counted in these studies. This lack of detail makes it harder for doctors to learn about ILC and improve care.
You also see fewer patients with metastatic ILC joining clinical trials. This matters because people in trials often live longer and get access to new treatments. If you have metastatic ILC, you may miss out on these benefits. Here are some facts about ILC in research:
Many cancer databases do not separate ILC into detailed subtypes.
Patients with both ILC and IDC often get excluded from studies.
People with metastatic ILC join clinical trials less often than those with other breast cancer types.
You need to know that better research representation can lead to improved treatments and survival rates for everyone with ILC.
Invasive Lobular Carcinoma (ILC) Features
Growth Patterns
You may notice that invasive lobular carcinoma (ILC) looks different from other breast cancers. ILC cells often grow in a single-file line or spread out in loose groups. This pattern makes it harder for doctors to spot the tumor early. You see that ILC can resist therapy and may lead to a poorer outlook for advanced disease. If you compare ILC to ductal carcinoma, you find that knowing the difference helps doctors choose better treatments. Some types of ILC, like pleomorphic lobular carcinoma (PLC), have larger and more irregular nuclei. PLC also shows higher grades and lower estrogen receptor levels than classic ILC. You may see higher Ki-67 levels in PLC, which means the cancer cells grow faster.
ILC grows in single-file or scattered patterns.
Tumors often resist therapy and show poorer outcomes in advanced cases.
PLC has larger nuclei and grows faster than classic ILC.
Tip: Ask your doctor about the growth pattern of your tumor. This can help guide your treatment plan.
Hormone Receptors
You may hear your doctor talk about hormone receptors when discussing ILC. Most cases of ILC have high levels of estrogen receptor (ER) positivity. Nearly 90% of ILC tumors show strong ER or progesterone receptor (PR) positivity. You rarely see ILC with low ER levels. This means hormone therapy often works well for many people with ILC. If your tumor has high hormone receptor levels, you may respond better to certain treatments.
Most ILC cases have ≥90% ER positivity.
ER-low status is very rare in ILC.
Hormone receptor positivity helps guide therapy choices.
Note: Knowing your hormone receptor status can help you and your doctor decide on the best treatment.
Metastasis
You may wonder where ILC spreads in the body. ILC often travels to places that other breast cancers do not. You see that ILC can move to the stomach, intestines, and other organs. The table below shows common sites for ILC and invasive ductal carcinoma (IDC):
Metastatic Site | ILC (Common) | IDC (Less Common) |
|---|---|---|
Gastrointestinal tract | ✔️ | |
Genitourinary tract | ✔️ | |
Retroperitoneum | ✔️ | |
Peritoneum | ✔️ | |
Pleura | Possible | |
Leptomeninges | Rare | |
Orbital canal | Rare |
You may notice that ILC grows slowly and often comes back many years after treatment. The single-file growth makes diagnosis harder and allows the cancer to reach unusual places.
Alert: If you have ILC, ask your doctor about the risk of late recurrence and unusual metastatic sites.
ILC Detection Challenges

Early Detection
You may find that early detection of invasive lobular carcinoma (ILC) is much harder than with other breast cancers. The unique way ILC grows makes it difficult for doctors to spot on regular exams or imaging. ILC cells often spread in single lines or loose groups, so the tumor does not form a clear lump. This means you might not feel a lump during a self-exam, and your doctor may not see obvious changes on a mammogram.
Doctors face several main challenges when trying to detect ILC early. The table below shows some of these problems and what they mean for you:
Challenge | Description |
|---|---|
Histopathological diagnosis | Doctors need clear and uniform ways to diagnose ILC under the microscope. |
Limitations of standard imaging tools | Mammograms and ultrasounds often miss ILC or show unclear results. |
Response assessment criteria | Current rules for measuring cancer response do not always work well for ILC, especially if it spreads. |
Liquid biopsies for disease progression | More research is needed to use blood tests to track ILC over time. |
You should know that ILC often gets diagnosed at a later stage than invasive ductal carcinoma (IDC). This happens because imaging tools do not always catch ILC early. Here are some facts:
ILC makes up 10–15% of all breast cancers.
Doctors often find ILC at a higher stage because it hides better on scans.
ILC cases have increased over time, especially in women after menopause.
IDC rates have stayed about the same.
Tip: If you have dense breast tissue or a family history of breast cancer, ask your doctor about extra screening options.
Imaging Issues
You may wonder why imaging tests sometimes miss ILC. The problem comes from both the way ILC grows and the limits of current technology. Mammograms, the most common breast cancer screening tool, do not always show ILC clearly. This is especially true if you have dense breast tissue. In these cases, the sensitivity drops, and doctors may not see the cancer at all.
Let’s look at how different imaging tools work for ILC:
Imaging Modality | Effectiveness in Detecting ILC | Limitations |
|---|---|---|
Mammography | Moderate (85% overall, 68% in dense breasts) | Misses many cases in dense tissue; high false negatives; does not show calcifications well. |
Ultrasound | Variable | Depends on the skill of the person doing the test; not great for finding many tumors at once. |
Breast MRI | High | Costs more; can show false alarms; may lead to extra treatments you do not need. |
Digital Breast Tomosynthesis (DBT) | High | Expensive; needs special machines; gives more radiation. |
Contrast-Enhanced Mammography (CEM) | High | Works almost as well as MRI in some studies; faster to read; still not as sensitive as MRI. |
Breast-Specific Gamma Imaging (BSGI) | High (93% sensitivity) | Not as good for finding cancer in the armpit or chest wall; best used as an extra test. |
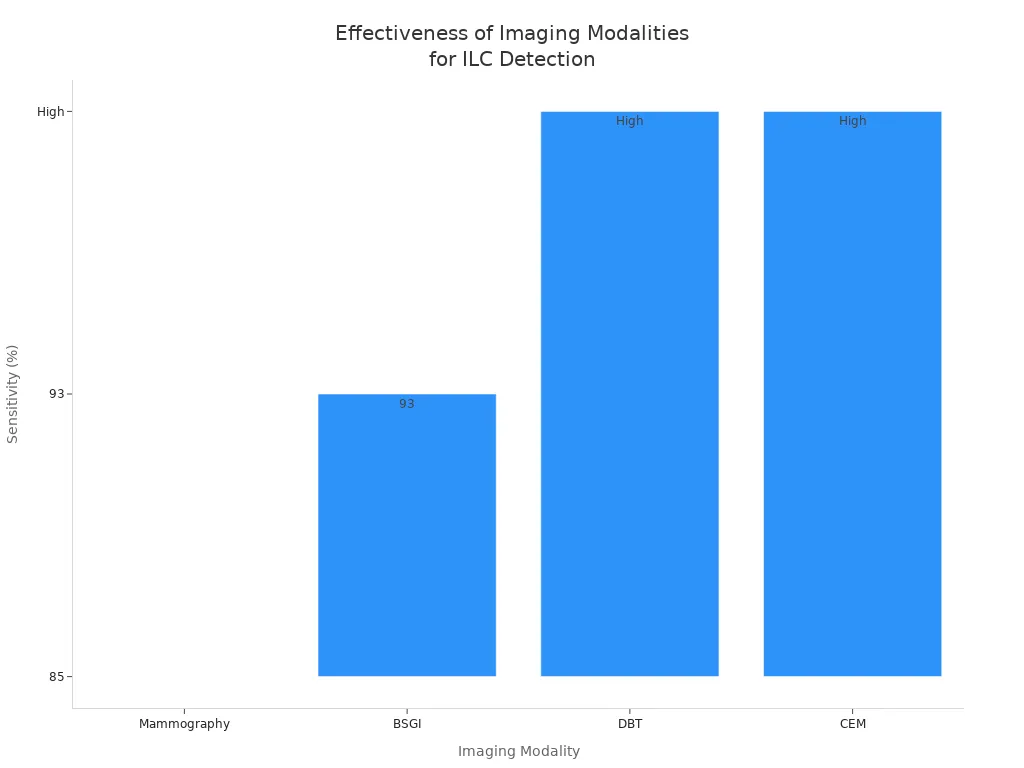
You see that MRI, DBT, and BSGI offer higher sensitivity for ILC than standard mammograms. However, these tests cost more and are not always available everywhere. Sometimes, these advanced scans show spots that are not cancer, which can lead to more biopsies or even unnecessary surgery.
Imaging problems can also affect your treatment plan. If doctors underestimate the size of your tumor, you may need another surgery to remove leftover cancer. If they overestimate, you might have a bigger surgery than you need. One study found that MRI missed the true size of the tumor in over half of ILC cases. This led to more positive margins and repeat surgeries.
Underestimating tumor size can leave cancer behind.
Overestimating can cause unnecessary removal of healthy tissue.
Note: Always ask your care team about the best imaging options for your situation. Newer tools may help find ILC earlier and guide better treatment.
ILC Treatment and Survival
Therapy Response
You may notice that invasive lobular carcinoma (ILC) responds differently to treatment than other breast cancer types. Chemotherapy often works less well for ILC, especially before surgery. You may see doctors use hormone therapy more often for ILC. Aromatase inhibitors usually help more than tamoxifen, based on recent studies. The table below shows how ILC compares to other breast cancers in therapy response:
Therapy Type | ILC Response | Other Breast Cancers (NST) Response |
|---|---|---|
Chemotherapy | Lower benefit | Higher benefit |
Aromatase Inhibitors | Higher benefit | Standard benefit |
Tamoxifen | Lower benefit than aromatase inhibitors | Standard benefit |
Tip: Ask your doctor if aromatase inhibitors are right for you. These medicines may improve your outcome if you have ILC.
Survival Rates
You may wonder about your chances of survival with ILC. Most women with ILC live many years after diagnosis. The five-year survival rate is about 89%. The ten-year survival rate is about 74%. If your cancer is found early, your chances are even better. Here are some key points:
About 94% of women with ILC are alive and cancer-free five years after diagnosis (stages I to III).
About 86% are alive and cancer-free ten years after diagnosis.
Your outcome depends on the stage and grade of your cancer.
Note: Every person is different. Your doctor can help you understand your own risks and outlook.
Advanced Disease Prognosis
If you have advanced ILC, several factors can affect your prognosis. The stage of your cancer, your age, and how your tumor responds to treatment all play a role. The table below lists some important factors:
Factor | Influence on Prognosis |
|---|---|
Black race | Worse outcomes |
Advanced stage | Worse outcomes |
Treatment response | Better survival |
Older age | Lower response rates |
Tumor aggressiveness | Early recurrence |
Higher TNM stage | |
Chemotherapy/radiation received | Better overall survival |
You should talk with your care team about these factors. They can help you make the best choices for your treatment and follow-up care.
Research and Future Directions
Data Limitations
You may notice that research on invasive lobular carcinoma (ILC) faces several data challenges. Many studies focus more on other breast cancer types, so you see fewer guidelines made just for ILC. Pathologists sometimes disagree on how to diagnose ILC, especially if they do not use special tests like E-cadherin analysis. Large genetic studies often do not include enough ILC cases, which makes it hard to learn about this cancer’s unique features. The table below shows some common data limitations:
Evidence Description | Limitation Type |
|---|---|
ILC is understudied relative to other breast cancers, with no specific treatment guidelines. | Research Underrepresentation |
ILCs are inadequately represented in large genomic data sets, and models are insufficient. | Data Representation Issues |
Lack of standard definitions for ILC diagnosis highlighted by pathologists. | Diagnostic Challenges |
Moderate inter-observer agreement among pathologists when diagnosing ILC without E-cadherin analysis. | Pathological Diagnosis Challenges |
Note: Better data and clear definitions can help doctors and researchers make progress in ILC care.
Research Needs
You see many gaps in current research. Scientists need to learn more about the genetic makeup of ILC. They also want to understand why some tumors resist drugs. You may benefit from new treatment plans made just for ILC. Researchers call for large clinical trials to test which treatments work best and to find new therapies. Here are some important research needs:
Learn more about the genes involved in ILC.
Study how and why ILC resists certain drugs.
Run big clinical trials to test new medicines and strategies.
Tip: If you join a clinical trial, you help doctors find better ways to treat ILC.
Improving Outcomes
You can help improve outcomes by staying informed and asking about new research. Doctors and scientists want to design treatments that match ILC’s special challenges. They push for clinical trials focused only on ILC. Ongoing research and funding are key to finding better options for you. Experts also stress the need to understand how ILC differs from other breast cancers. They hope new studies will lead to better survival and quality of life. Some future directions include:
Develop treatment plans made just for ILC.
Support clinical trials that focus on ILC patients.
Fund research that explores how ILC and other breast cancers differ.
Find new ways to treat ILC when chemotherapy does not work well.
Alert: You can talk to your care team about joining research studies or clinical trials. Your participation may help others in the future.
You see that invasive lobular carcinoma (ILC) cases continue to rise, often linked to hormone therapy. The table below shows the main findings:
Key Finding | Description |
|---|---|
More women receive an ILC diagnosis each year, especially after menopause. | |
Detection Challenges | ILC’s growth pattern makes it hard to find early, leading to late diagnoses. |
You need to know that ILC differs from other breast cancers in how it grows and responds to treatment. Doctors and researchers must recognize these differences to improve care. You can help by eating more fruits, vegetables, and whole grains, and by starting screening early if you are at high risk. Clinicians should use advanced imaging and work with expert pathologists. Researchers and advocates can build registries, support clinical trials, and raise awareness through events like Global Lobular Breast Cancer Awareness Day. Together, you can help close research gaps and improve outcomes for women with ILC.
FAQ
What makes ILC different from other breast cancers?
You see ILC grow in single-file lines. This pattern makes it harder to find on scans. ILC often spreads to unusual places in your body. Most ILC tumors respond well to hormone therapy.
Note: ILC rarely forms a lump you can feel.
How can you improve early detection of ILC?
You can ask your doctor about advanced imaging, like MRI or 3D mammograms. These tools help find ILC earlier. If you have dense breasts or a family history, you may need extra screening.
Ask for MRI if mammograms miss changes.
Share your risk factors with your doctor.
What symptoms should you watch for with ILC?
You may not feel a lump. Watch for subtle changes:
Symptom | Description |
|---|---|
Breast thickening | Area feels firmer or fuller |
Skin changes | Dimpling or puckering |
Nipple changes | Inversion or discharge |
Alert: Report any new breast changes to your doctor.
Does ILC have a good survival rate?
You have a high chance of living many years after diagnosis. Most women with early ILC survive at least five years. Your outcome improves with early detection and the right treatment.
Tip: Regular checkups and following your treatment plan help improve your outlook.
See Also
Understanding Invasive Lobular Carcinoma And Its Key Symptoms
Exploring Invasive Ductal Carcinoma And Its Common Symptoms
Defining Ductal Carcinoma In Situ And Its Notable Symptoms
Insights Into Invasive Cribriform Carcinoma Of The Breast
A Comprehensive Guide To Large-Cell Lung Carcinoma Classification

