Are All Cancers Linked to Genetic Mutations

Not all cancers stem from genetic mutations, but many are influenced by them. You might wonder if cancer is always genetic? The answer lies in understanding the difference between inherited and acquired mutations. Only 10-20% of cancers result from inherited mutations, while the majority, about 80-90%, are sporadic. These sporadic cancers often arise from environmental exposures or lifestyle factors. By exploring these distinctions, you can better grasp how genetic alterations contribute to cancer without assuming all cases are hereditary.
Key Takeaways
Only 10-20% of cancers come from inherited gene changes. Most cancers happen because of changes caused by lifestyle or environment.
These changes can be from smoking, sunlight, or random cell mistakes. They can make the chance of cancer much higher.
Choosing healthy habits, like working out and eating well, can lower cancer risk. Small steps can make a big difference.
Genetic tests can show if you have cancer risks from family. Talk to a genetic counselor to see if testing is good for you, especially if cancer runs in your family.
Knowing both genetic and lifestyle causes helps you understand cancer better. This knowledge helps you make smart health choices.
Cancer Is Always Genetic?
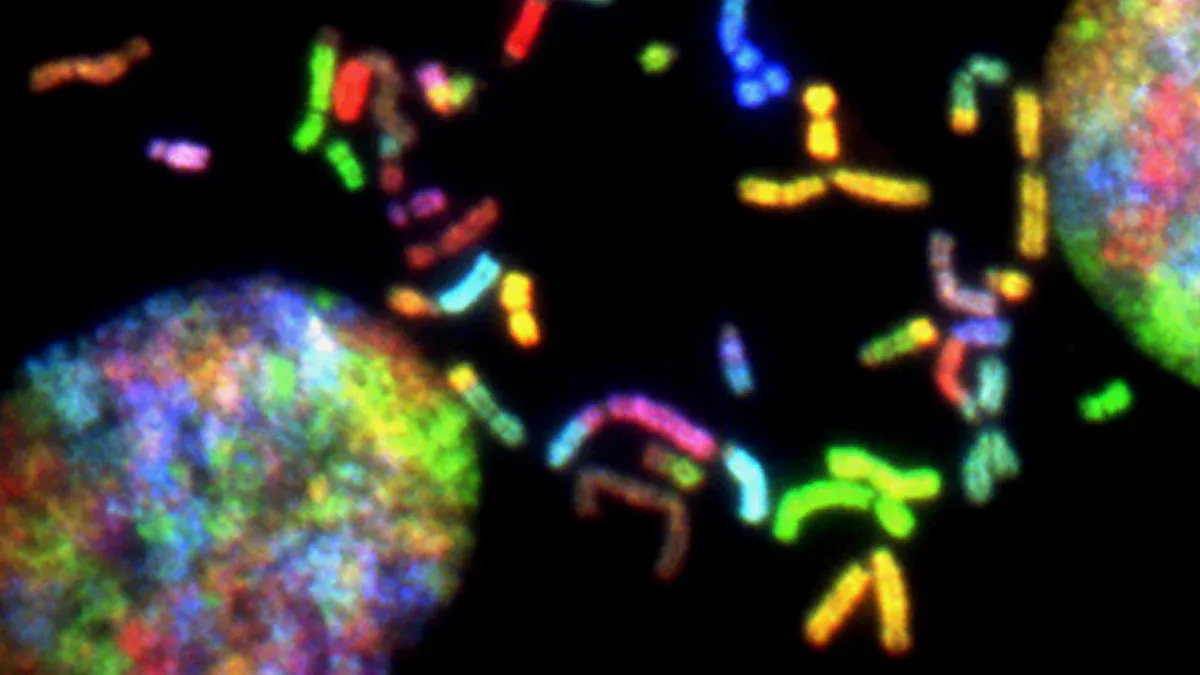
The Role of Genetic Alterations
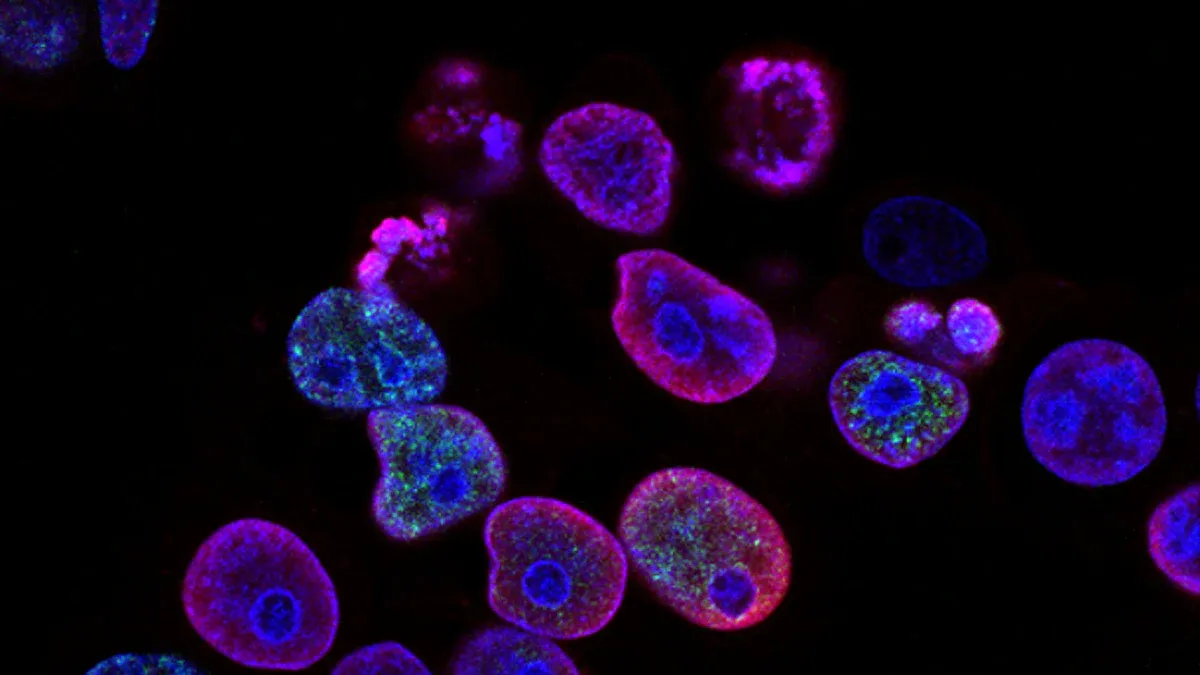
You might wonder if cancer is always genetic. While all cancers involve genetic changes, these alterations occur in different ways. Some arise from inherited mutations, while others result from environmental exposures or random errors during cell division. Research shows that up to 66% of cancers stem from random gene changes, while environmental factors contribute about 23%. For certain cancers, like lung and skin cancers, environmental factors play a larger role, accounting for more than 60% of cases. This highlights the complex interplay between genetic and non-genetic factors in cancer development.
Genetic alterations can accumulate over time due to aging, exposure to mutagenic chemicals, or ultraviolet light. These changes can transform normal cells into cancerous ones. Scientists refer to tissues with accumulated alterations as "cancerization fields," which carry a higher risk of developing cancer. For example, studies have found that epigenetic changes, such as DNA methylation, can have a 2.3-fold greater impact on cancer risk than genetic mutations in some tissues. This demonstrates that while genetic alterations are crucial, they are not the sole drivers of cancer.
Distinguishing Hereditary and Non-Hereditary Cancers
Not all cancers are hereditary. In fact, only 10-20% of cancers result from inherited mutations passed down through families. These hereditary cancers often appear at an earlier age because individuals inherit a mutation that predisposes them to cancer. For example, mutations in genes like BRCA1 and BRCA2 increase the risk of breast and ovarian cancers.
In contrast, most cancers are non-hereditary, or sporadic. These arise from mutations that occur only in the tumor itself and are not passed down to offspring. Acquired mutations, which account for the majority of cancer cases, often result from environmental exposures or random errors during cell division. For instance, lung cancer frequently develops due to smoking, while skin cancer often results from prolonged UV exposure. Understanding these distinctions helps you see why cancer is not always genetic in origin.
Types of Genetic Mutations in Cancer
Inherited Mutations
Inherited mutations are genetic changes passed from parents to their children. These mutations exist in every cell of your body from birth and increase your risk of developing cancer. For example, inheriting a mutation in the BRCA1 or BRCA2 genes significantly raises the likelihood of breast and ovarian cancers. According to the National Cancer Institute, about 10% of all cancers result from inherited mutations. This means that while cancer is always genetic in nature, only a small percentage stems from mutations you inherit.
When you inherit a mutation, your cells start with one genetic alteration. This makes it easier for additional mutations to accumulate over time, leading to cancer. Cancers caused by inherited mutations often develop earlier in life compared to those caused by acquired mutations. For instance, individuals with Li-Fraumeni syndrome, linked to TP53 mutations, face a higher risk of developing multiple cancer types at a young age. Understanding inherited mutations helps you recognize the importance of family history in assessing cancer risk.
Acquired Mutations
Acquired mutations, also known as somatic mutations, occur during your lifetime and are not passed to your children. These mutations arise from environmental exposures, such as smoking or ultraviolet radiation, or random errors during cell division. Unlike inherited mutations, acquired mutations only affect specific cells and are not present in every cell of your body.
Studies show that TP53, the most commonly mutated gene, appears in 35% of cancer cases. Other frequently mutated genes include PIK3CA, KRAS, and BRAF. These mutations often correlate with tumor progression and poor clinical outcomes. For example, TP53 mutations are associated with advanced tumor stages and reduced survival rates. Acquired mutations play a significant role in cancer development, emphasizing the impact of lifestyle and environmental factors on your health.
Environmental and Lifestyle Factors in Cancer
Carcinogens and Their Impact
Carcinogens are substances that can cause cancer by damaging your DNA or interfering with cellular processes. These harmful agents exist in various forms, including chemicals, radiation, and even certain viruses. For example, tobacco smoke contains over 70 known carcinogens, making smoking one of the leading causes of lung cancer. Similarly, prolonged exposure to ultraviolet (UV) rays from the sun increases your risk of skin cancer.
You encounter carcinogens in everyday life, but their impact depends on the level and duration of exposure. For instance, asbestos, a material once widely used in construction, can lead to mesothelioma when inhaled over time. Industrial chemicals like benzene, found in some solvents, also pose significant risks. Even processed meats, classified as Group 1 carcinogens by the World Health Organization, have been linked to colorectal cancer.
Tip: Reducing your exposure to carcinogens can lower your cancer risk. Simple steps like using sunscreen, avoiding tobacco, and limiting processed foods can make a big difference.
Lifestyle Choices and Cancer Risk
Your lifestyle choices play a crucial role in cancer prevention. Habits like smoking, excessive alcohol consumption, and poor diet increase your risk. For example, smoking not only causes lung cancer but also contributes to cancers of the throat, mouth, and bladder. Drinking alcohol excessively can damage your liver and lead to liver cancer.
A sedentary lifestyle also raises your risk. Physical inactivity contributes to obesity, which is linked to several cancers, including breast and colon cancer. On the other hand, regular exercise helps regulate hormones and boosts your immune system, reducing cancer risk.
Healthy eating is another key factor. Diets rich in fruits, vegetables, and whole grains provide antioxidants that protect your cells from damage. Avoiding sugary drinks and processed foods can help maintain a healthy weight, further lowering your risk.
Note: Small changes in your daily habits can have a significant impact on your long-term health. Start with manageable goals, like adding a 30-minute walk to your routine or swapping sugary snacks for fresh fruit.
Hereditary Cancers and Family Syndromes
Examples of Hereditary Cancers
Some cancers run in families due to inherited genetic mutations. These hereditary cancers often appear earlier in life and may affect multiple family members. For example, mutations in the BRCA1 and BRCA2 genes significantly increase your risk of breast and ovarian cancers. Men with these mutations also face a higher risk of prostate cancer. Another example is Lynch syndrome, caused by mutations in DNA mismatch repair genes. This syndrome raises your likelihood of developing colorectal, endometrial, and other cancers.
Retinoblastoma, a rare eye cancer in children, is another hereditary cancer. It occurs when mutations in the RB1 gene are passed down. Similarly, familial adenomatous polyposis (FAP) results from mutations in the APC gene. If you inherit this mutation, you may develop hundreds of polyps in your colon, increasing your risk of colorectal cancer. These examples highlight how specific genetic mutations can lead to hereditary cancer syndromes.
Note: If multiple relatives have the same type of cancer, especially at a young age, it may indicate a hereditary cancer syndrome. Consulting a genetic counselor can help you assess your risk.
Patterns of Inheritance
Hereditary cancers follow specific inheritance patterns. Most are passed down in an autosomal dominant manner. This means you only need one copy of the mutated gene from either parent to have an increased cancer risk. For instance, BRCA1 and BRCA2 mutations follow this pattern. If one parent carries the mutation, you have a 50% chance of inheriting it.
Some hereditary cancers, like those linked to Lynch syndrome, also follow autosomal dominant inheritance. However, not everyone who inherits a mutation will develop cancer. This concept, called incomplete penetrance, means other factors, such as lifestyle or additional mutations, influence your risk.
Understanding these patterns helps you recognize how hereditary cancers are passed through families. If you suspect a family history of cancer, genetic testing can provide clarity and guide preventive measures.
Genetic Testing and Cancer Risk
Benefits of Genetic Testing
Genetic testing can provide valuable insights into your cancer risk. By analyzing your DNA, it identifies inherited mutations that may increase your likelihood of developing certain cancers. For example, testing for BRCA1 and BRCA2 mutations can help you understand your risk for breast and ovarian cancers. This knowledge empowers you to take proactive steps, such as increased screenings or preventive measures, to protect your health.
Testing also benefits your family. If you carry a genetic mutation, your relatives may want to get tested too. This can help them assess their own risks and make informed decisions about their health. Additionally, genetic testing can guide doctors in tailoring treatments. For instance, some therapies target specific mutations, making them more effective for certain patients.
Tip: If you have a family history of cancer, consider consulting a genetic counselor. They can help you decide if testing is right for you.
Limitations and Ethical Considerations
While genetic testing offers many benefits, it has limitations. It cannot predict with certainty whether you will develop cancer. A positive result means you have a higher risk, but other factors, like lifestyle and environment, also play a role. Remember, cancer is always genetic? Not entirely. Most cancers result from acquired mutations, not inherited ones.
Ethical concerns also arise with genetic testing. Sharing your results with insurance companies or employers could lead to discrimination. Although laws like the Genetic Information Nondiscrimination Act (GINA) exist, they may not cover all situations. Testing can also cause emotional stress. Learning about a high cancer risk might leave you feeling anxious or overwhelmed.
Note: Before undergoing genetic testing, weigh the benefits and risks carefully. A genetic counselor can help you navigate these complex decisions.
Not all cancers result from genetic mutations, but many are influenced by them. Both inherited and acquired mutations play a role, along with environmental and lifestyle factors. Understanding these elements helps you see the bigger picture of cancer development.
Inherited mutations may increase your risk, but they account for only a small percentage of cases.
Acquired mutations often arise from lifestyle choices or environmental exposures.
Tip: Genetic testing can guide you in making informed decisions, but it’s not necessary for everyone. A complete understanding of cancer requires considering both genetic and non-genetic factors.
FAQ
What is the difference between inherited and acquired mutations?
Inherited mutations are passed from your parents and exist in every cell of your body. Acquired mutations develop during your lifetime due to environmental factors or random errors in cell division. Inherited mutations increase your risk from birth, while acquired mutations occur later and affect specific cells.
Can lifestyle changes reduce cancer risk?
Yes, lifestyle changes can lower your risk. Avoid smoking, limit alcohol, eat a balanced diet, and exercise regularly. These habits reduce exposure to carcinogens and help maintain a healthy weight, which lowers the likelihood of developing certain cancers.
Tip: Start small. Replace sugary snacks with fruits or add a daily walk to your routine.
Should everyone get genetic testing for cancer?
Not everyone needs genetic testing. It’s most useful if you have a strong family history of cancer or early-onset cases in relatives. A genetic counselor can help you decide if testing is right for you based on your personal and family history.
How do environmental factors cause cancer?
Environmental factors, like UV rays or tobacco smoke, damage your DNA. This damage can lead to mutations that trigger cancer. For example, prolonged sun exposure increases skin cancer risk, while smoking is a leading cause of lung cancer.
Note: Protect yourself by using sunscreen and avoiding tobacco products.
Are all cancers hereditary?
No, most cancers are not hereditary. Only 10-20% of cancers result from inherited mutations. The majority arise from acquired mutations caused by environmental exposures, lifestyle choices, or random errors during cell division.
Reminder: Understanding your family history can still help assess your risk for hereditary cancers.
See Also
Exploring Cancer Types Associated With AIDS Infection
An In-Depth Overview of Various Cancer Categories
Identifying Signs and Origins of Head and Neck Cancer
Understanding Lung Adenocarcinoma Causes and Associated Risks

