Understanding Islet Cell Carcinoma in the Endocrine Pancreas
Islet cell carcinoma is a rare type of neuroendocrine tumor that develops in the islet cell carcinoma endocrine pancreas. Unlike more common pancreatic cancers, this condition arises from islet cells, which regulate hormones like insulin. Its rarity makes it challenging to diagnose, but understanding its unique nature can help you recognize potential symptoms. Early detection plays a critical role in improving outcomes. If you notice unusual signs, seeking medical advice promptly could make a significant difference in treatment success.
Key Takeaways
Islet cell carcinoma is a rare type of pancreas tumor. It affects cells that make hormones. Finding it early helps with better treatment.
Some tumors make too many hormones. This can cause low blood sugar or stomach pain. Knowing these signs can help find it sooner.
Surgery is often the best way to treat this cancer. It works well if the tumor hasn’t spread. Talk to your doctor about treatment choices.
Your genes and some health problems can raise your risk. Getting regular check-ups can help find problems early.
Eating healthy foods and exercising can lower your risk. It also helps you stay healthier overall.
The Endocrine Pancreas and Islet Cells
What is the Endocrine Pancreas?
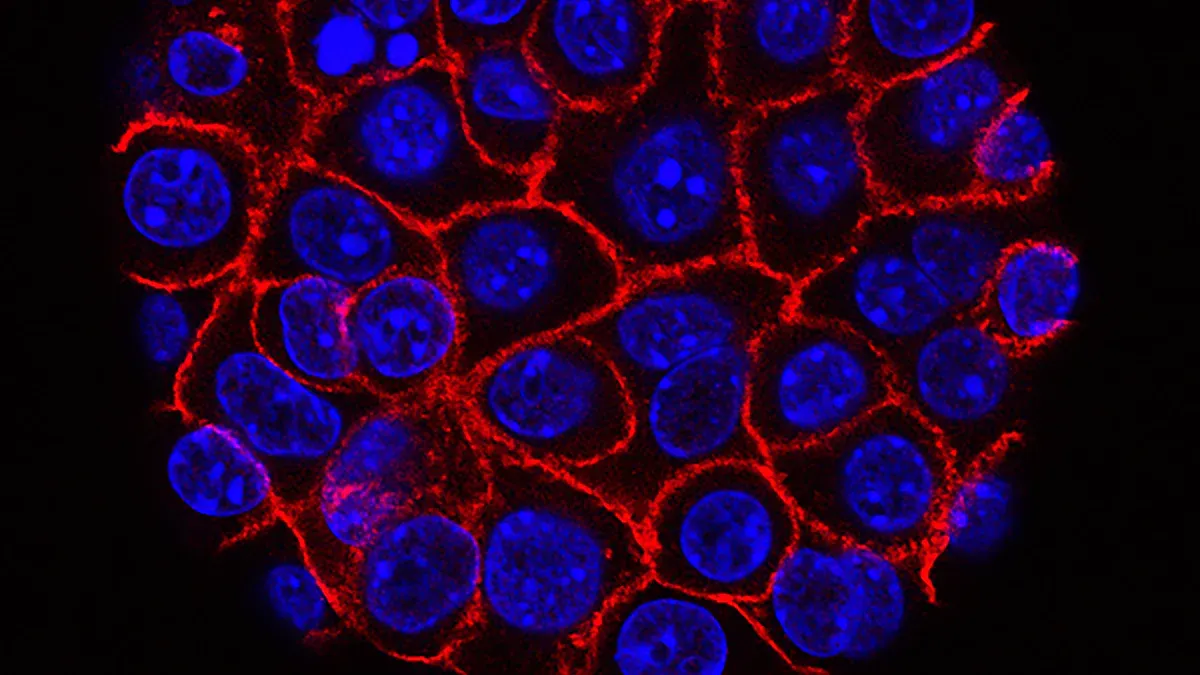
The endocrine pancreas is a vital part of your body’s digestive and hormonal systems. It consists of small clusters of cells called islets of Langerhans, which are scattered throughout the pancreas. These islets play a key role in regulating your blood sugar levels by producing essential hormones. Unlike the exocrine pancreas, which helps digest food, the endocrine pancreas focuses on maintaining your body’s internal balance.
Functions of Islet Cells
Islet cells in the endocrine pancreas perform critical functions to keep your body healthy. They produce hormones like insulin and glucagon, which control your blood sugar levels. Insulin, made by beta cells, lowers blood sugar by helping your cells absorb glucose and store it as glycogen in the liver. On the other hand, glucagon, produced by alpha cells, raises blood sugar when it drops too low. This balance ensures your body has enough energy to function properly. Without these hormones, your body would struggle to regulate blood sugar, leading to serious health issues.
Differences Between Islet Cells and Exocrine Pancreatic Cells
Islet cells differ significantly from exocrine pancreatic cells in both structure and function.
Islet cells belong to the endocrine pancreas and are grouped into islets of Langerhans, while exocrine cells form acini, which secrete digestive enzymes.
Islet cells are highly vascularized, receiving much more blood supply than exocrine cells.
Each islet contains different cell types, such as alpha and beta cells, that produce hormones like insulin and glucagon. In contrast, exocrine cells focus on producing enzymes to break down food in your digestive system.
These differences highlight the unique role of islet cells in managing your body’s hormonal balance, which is crucial when understanding conditions like islet cell carcinoma endocrine pancreas.
Understanding Islet Cell Carcinoma
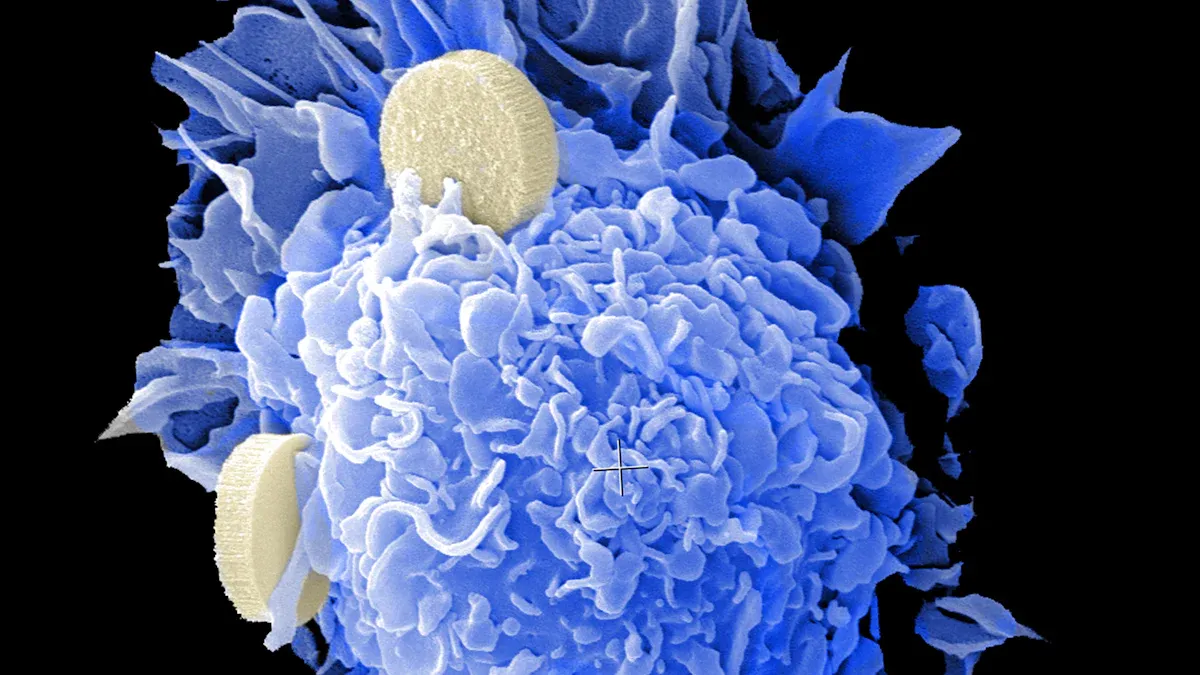
Classification as a Neuroendocrine Tumor
Islet cell carcinoma belongs to a group of tumors called pancreatic neuroendocrine tumors (NETs). These tumors originate specifically in the islet cells of the pancreas, which produce hormones like insulin and glucagon. This unique origin classifies them as neuroendocrine tumors. Unlike other pancreatic cancers, these tumors arise from the endocrine pancreas rather than the exocrine pancreas. You may also hear them referred to as islet cell tumors or islet cell carcinoma.
Types of Islet Cell Tumors
Islet cell tumors are categorized into two main types based on their ability to produce hormones.
Functional Tumors (e.g., insulinomas, gastrinomas)
Functional tumors produce excessive hormones, leading to noticeable symptoms. For example:
Insulinomas: These tumors produce too much insulin, causing low blood sugar, dizziness, and confusion.
Gastrinomas: These increase gastrin production, leading to stomach ulcers and abdominal pain.
Glucagonomas: These raise blood sugar levels and may cause diabetes or skin rashes.
VIPomas: These disrupt intestinal hormone production, resulting in severe diarrhea and dehydration.
Treatment for functional tumors often involves surgery to remove the tumor. In some cases, additional therapies may be necessary to manage symptoms caused by excessive hormone production.
Non-Functional Tumors
Non-functional tumors do not produce hormones, so they often remain undetected until they grow large or spread. Symptoms typically include abdominal pain, weight loss, or signs caused by the tumor pressing on nearby organs. Surgery can help alleviate symptoms, but observation may be recommended for slow-growing tumors.
Type of Tumor | Symptoms | Treatment Approach |
|---|---|---|
Functional Tumors | Symptoms arise from hormones secreted, such as low blood sugar, abdominal pain, or skin rash. | Surgery is the only curative option; palliation may be needed for metastatic cases. |
Non-Functional Tumors | Present late with symptoms due to mass effect or metastases. | Surgery may alleviate symptoms; careful observation may be the best approach for indolent tumors. |
How It Differs from Exocrine Pancreatic Cancer
Islet cell carcinoma differs significantly from exocrine pancreatic cancer in terms of symptoms and prognosis. While islet cell carcinoma endocrine pancreas often presents with hormonal imbalances or mild symptoms early on, exocrine pancreatic cancer typically shows advanced signs like jaundice, dark urine, and severe abdominal pain. The prognosis for islet cell carcinoma is generally better, especially when detected early.
Type of Cancer | Symptoms | Prognosis |
|---|---|---|
Pancreatic Neuroendocrine Cancer | Early symptoms include diarrhea, indigestion, blood sugar changes, weight loss, stomach pain, jaundice, skin rash. | |
Exocrine Pancreatic Cancer | Advanced signs include jaundice, light-colored stools, dark urine, abdominal pain, weight loss, loss of appetite. | Poorer chance of recovery |
Understanding these differences can help you recognize the unique challenges and opportunities for treatment associated with islet cell carcinoma endocrine pancreas.
Causes and Risk Factors
Genetic Predispositions
Your genetic makeup can play a significant role in the development of islet cell carcinoma. Certain inherited mutations increase your risk of developing this rare tumor. For example, mutations in genes like MEN1 (multiple endocrine neoplasia type 1) or VHL (von Hippel-Lindau syndrome) are strongly linked to islet cell tumors. If you have a family history of these conditions, you may face a higher risk. Genetic testing can help identify these mutations early, giving you a chance to monitor your health closely.
Tip: If you know of any family members with endocrine-related conditions, consider discussing genetic testing with your doctor.
Associated Syndromes (e.g., MEN1)
Some syndromes are directly associated with islet cell carcinoma. MEN1 is one of the most common syndromes linked to this condition. It causes tumors in multiple endocrine glands, including the pancreas. Other syndromes, like von Hippel-Lindau and neurofibromatosis type 1, also increase your risk. These syndromes often lead to functional tumors that produce excess hormones, causing noticeable symptoms. If you have been diagnosed with one of these syndromes, regular screenings can help detect islet cell carcinoma early.
Environmental and Lifestyle Influences
While genetic factors are significant, your environment and lifestyle also contribute to your risk. Exposure to harmful chemicals, such as those found in industrial settings, may increase your chances of developing islet cell carcinoma. Smoking and a diet high in processed foods can also negatively impact your pancreas. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can reduce your overall risk.
Note: Although lifestyle changes cannot eliminate genetic risks, they can improve your overall health and lower the likelihood of complications.
Symptoms and Signs
Symptoms of Functional Tumors
Functional tumors cause hormonal imbalances due to excessive hormone production. These imbalances lead to distinct symptoms depending on the type of tumor. The table below outlines common functional tumors and their associated symptoms:
Tumor Type | Symptoms |
|---|---|
Insulinoma | Low blood sugar, dizziness, lightheadedness, weakness, confusion, tremors, visual changes. |
Gastrinoma | Abdominal pain, diarrhea, peptic ulcer disease. |
Glucagonoma | Skin rash, diabetes, diarrhea, deep vein thrombosis. |
VIPomas | Severe diarrhea, dehydration, muscle weakness, hypokalemia, achlorhydria. |
Somatostatinoma | Weight loss, anemia, foul-smelling and oily stools, diabetes, gallbladder disease. |
If you experience any of these symptoms, especially in combination, it may indicate a functional tumor. Early diagnosis can help manage these conditions effectively.
Symptoms of Non-Functional Tumors
Non-functional tumors differ from functional ones because they do not produce hormones. As a result, they often remain undetected until they grow large or spread. Symptoms typically include abdominal pain, unexplained weight loss, or discomfort caused by the tumor pressing on nearby organs. Unlike functional tumors, non-functional tumors lack hormone-related symptoms, which can delay their diagnosis. This delay often results in detection at more advanced stages, making treatment more challenging.
When to Seek Medical Advice
You should consult a healthcare provider if you notice persistent symptoms like abdominal pain, unexplained weight loss, or signs of hormonal imbalances such as dizziness or severe diarrhea. Early detection of conditions like islet cell carcinoma endocrine pancreas can significantly improve treatment outcomes. Regular check-ups and discussing any unusual symptoms with your doctor can help identify potential issues before they progress.
Diagnosis of Islet Cell Carcinoma
Imaging Techniques
CT Scans and MRI
Imaging techniques play a crucial role in diagnosing islet cell carcinoma. CT scans and MRI are among the most effective tools for detecting these tumors. A study comparing these methods found that biphasic CT and delayed enhanced T1-weighted MRI offer high sensitivity rates. These techniques provide detailed images of the pancreas, helping doctors identify tumors early.
You may also encounter other imaging methods during diagnosis:
Endoscopic Ultrasound: A probe inserted through your digestive tract uses sound waves to create images of the pancreas.
MRI and Triphasic CT Scanning: These scans capture images during different phases of blood flow, improving diagnostic accuracy.
OctreoScan Imaging: This method uses a radioactive form of somatostatin to detect tumors based on their absorption levels.
These imaging tools allow healthcare providers to locate tumors and assess their size and spread.
Blood Tests and Hormonal Analysis
Blood and urine tests are essential for diagnosing islet cell carcinoma. These tests measure hormone levels and detect abnormalities caused by functional tumors. For example:
Test Type | Purpose |
|---|---|
Look for increased levels of hormones | |
Urine tests | Look for increased levels of substances |
If you have a functional tumor, these tests can reveal elevated levels of insulin, gastrin, or other hormones. This information helps doctors confirm the presence of a tumor and determine its type.
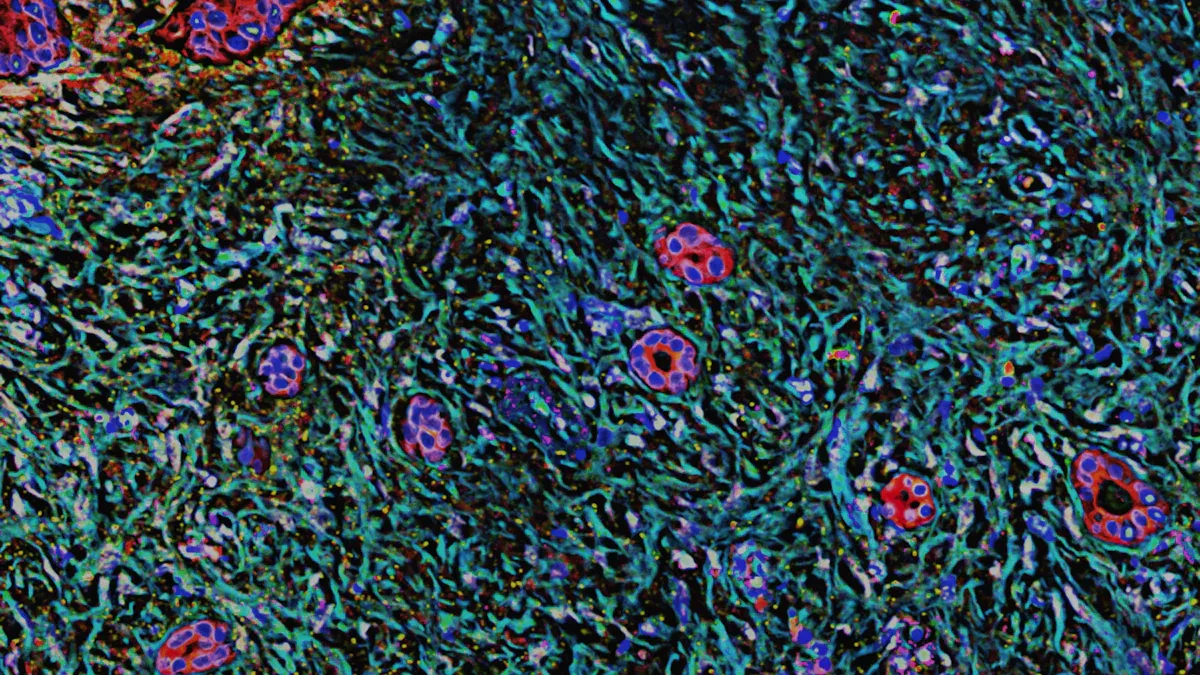
Biopsy and Histopathological Examination
A biopsy provides a definitive diagnosis of islet cell carcinoma. During this procedure, a small tissue sample is taken from the tumor and examined under a microscope. Histopathological analysis identifies the tumor type and determines whether it is cancerous. This step is critical for planning the most effective treatment.
Tip: If your doctor recommends a biopsy, it’s an important step toward understanding your condition and starting the right treatment.
Treatment Options for Islet Cell Carcinoma
Surgical Interventions
Surgery is often the first-line treatment for islet cell carcinoma. It offers the best chance for a cure, especially when the tumor is localized. Your doctor may recommend surgery based on the tumor's size, location, and whether it has spread.
Types of Surgery
Several surgical options exist for treating islet cell carcinoma. These include:
Enucleation: This procedure removes small, localized tumors while preserving most of the pancreas. It is often used for functional tumors.
Pancreaticoduodenectomy (Whipple Procedure): This complex surgery removes the head of the pancreas, part of the small intestine, and nearby tissues. It is suitable for larger tumors.
Distal Pancreatectomy: This surgery removes the tail of the pancreas and sometimes the spleen. It is often used for tumors in the pancreas's tail region.
Total Pancreatectomy: In rare cases, the entire pancreas is removed. This option is considered when multiple tumors are present or the cancer is widespread.
Your surgeon will choose the most appropriate procedure based on your condition. Surgery can significantly improve your prognosis, especially when performed early.
Chemotherapy and Targeted Therapies
Chemotherapy may be recommended if the cancer has spread or surgery is not an option. It uses drugs to kill cancer cells or slow their growth. Targeted therapies, on the other hand, focus on specific molecules involved in tumor growth. These therapies often have fewer side effects compared to traditional chemotherapy. For islet cell carcinoma endocrine pancreas, targeted drugs like everolimus and sunitinib have shown promising results. They work by blocking pathways that tumors use to grow and spread.
Hormone Therapy for Functional Tumors
Functional tumors produce excess hormones, leading to various symptoms. Hormone therapy helps control these symptoms by reducing hormone production or blocking their effects. For example, somatostatin analogs like octreotide and lanreotide can manage symptoms caused by insulinomas or gastrinomas. These medications improve your quality of life and may even slow tumor growth.
Note: Hormone therapy is not a cure but an effective way to manage symptoms while undergoing other treatments.
Palliative Care for Advanced Stages
When islet cell carcinoma reaches advanced stages, palliative care becomes an essential part of your treatment plan. This type of care focuses on improving your quality of life by managing symptoms and addressing emotional, physical, and psychological needs. It does not aim to cure the disease but helps you live more comfortably.
Key Goals of Palliative Care
Palliative care for advanced islet cell carcinoma has several important objectives:
Symptom Management: You may experience pain, fatigue, or digestive issues. Palliative care specialists use medications and therapies to reduce these symptoms.
Emotional Support: Coping with advanced cancer can feel overwhelming. Counselors and support groups can help you manage stress and anxiety.
Improved Comfort: Treatments like radiation or nerve blocks can relieve pain caused by tumors pressing on nearby organs.
Tip: Discuss your symptoms openly with your care team. They can tailor treatments to meet your specific needs.
Common Palliative Treatments
Your care team may recommend a combination of treatments to address your symptoms:
Pain Relief: Medications like opioids or nonsteroidal anti-inflammatory drugs (NSAIDs) can help control pain.
Nutritional Support: Dietitians can guide you on foods that are easier to digest and provide essential nutrients.
Psychological Care: Therapists can assist you in processing emotions and maintaining a positive outlook.
The Role of Your Care Team
Palliative care involves a team of specialists, including doctors, nurses, and social workers. They work together to ensure you receive comprehensive care. This team also supports your family, helping them understand your condition and providing guidance on how to assist you.
Note: Palliative care can begin alongside other treatments. It is not limited to end-of-life care and can benefit you at any stage of advanced cancer.
By focusing on your comfort and well-being, palliative care helps you maintain dignity and enjoy a better quality of life during challenging times.
Prognosis and Outlook
Survival Rates and Statistics
The prognosis for islet cell carcinoma depends on several factors, including the tumor type and stage at diagnosis. Studies show that patients with localized tumors have a five-year survival rate of approximately 90%. However, this rate decreases significantly when the cancer spreads to distant organs. Non-functional tumors, often diagnosed at later stages, tend to have a poorer prognosis compared to functional tumors. Early detection plays a critical role in improving survival outcomes.
Factors Affecting Prognosis
Several factors influence the prognosis of islet cell carcinoma. Understanding these can help you and your healthcare team make informed decisions about treatment.
Tumor Type and Stage
The type of cancer cell and the stage at diagnosis are crucial. Functional tumors, which produce hormones, often present symptoms earlier, leading to earlier detection. Non-functional tumors, on the other hand, may remain undetected until they grow larger or metastasize. The stage of the tumor—whether localized, regional, or metastatic—directly impacts survival rates.
Response to Treatment
Your response to treatment also affects the prognosis. Tumors that respond well to surgery, chemotherapy, or targeted therapies typically offer better outcomes. Factors like your overall health and age can influence how well you tolerate treatments.
Factor | Description |
|---|---|
Type of cancer cell | Different types of islet cell tumors may have varying prognoses. |
Tumor location | The specific location of the tumor in the pancreas can impact outcomes. |
Tumor spread | Whether the tumor has metastasized affects the prognosis significantly. |
MEN1 syndrome | Presence of this syndrome can influence prognosis and treatment. |
Patient's age and health | Older age and poor health can negatively affect recovery chances. |
Diagnosis timing | Prognosis may differ if the cancer is newly diagnosed versus recurrent. |
Importance of Early Diagnosis
Early diagnosis significantly improves the outlook for islet cell carcinoma endocrine pancreas. Detecting the tumor before it spreads allows for more effective treatment options, such as surgery. Regular check-ups and paying attention to unusual symptoms can make a difference. If you notice persistent signs like abdominal pain or hormonal imbalances, consulting a healthcare provider promptly can improve your chances of recovery.
Islet cell carcinoma is a rare but significant condition that affects the endocrine pancreas. You’ve learned about its symptoms, causes, and treatment options, including surgery, hormone therapy, and palliative care. Early detection remains crucial for improving outcomes.
Remember: If you notice unusual symptoms like abdominal pain, weight loss, or hormonal imbalances, consult a healthcare provider promptly. Early action can make a difference.
Stay informed and proactive about your health. If you have questions or concerns, don’t hesitate to seek professional advice. Your health deserves attention and care.
FAQ
What makes islet cell carcinoma different from other pancreatic cancers?
Islet cell carcinoma originates in the endocrine pancreas, affecting hormone-producing cells. Other pancreatic cancers, like exocrine pancreatic cancer, arise in the digestive enzyme-producing cells. Islet cell carcinoma often presents with hormonal symptoms, while exocrine pancreatic cancer typically shows digestive-related symptoms.
Can islet cell carcinoma be cured?
Yes, early-stage islet cell carcinoma can often be cured with surgery. Treatment success depends on factors like tumor size, type, and spread. Functional tumors detected early have better outcomes. Regular check-ups improve the chances of early detection.
Are islet cell tumors always cancerous?
No, not all islet cell tumors are cancerous. Some are benign and grow slowly without spreading. However, even benign tumors can cause symptoms due to hormone overproduction. A doctor can determine the tumor type through tests and imaging.
How can you reduce the risk of islet cell carcinoma?
You can lower your risk by maintaining a healthy lifestyle. Avoid smoking, eat a balanced diet, and exercise regularly. If you have a family history of related syndromes, consider genetic testing and regular screenings.
What should you do if you suspect islet cell carcinoma?
Consult a healthcare provider immediately if you notice symptoms like unexplained weight loss, abdominal pain, or hormonal imbalances. Early diagnosis improves treatment options and outcomes. Don’t ignore persistent or unusual symptoms.
Tip: Keep a record of your symptoms to share with your doctor for a more accurate diagnosis.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Key Features and Insights About Cholangiocarcinoma
Essential Information You Need About Carcinoid Tumors
Important Facts You Should Know About Embryonal Carcinoma

