Understanding Large-cell Lung Carcinoma and Its Classification
Large-cell lung carcinoma is a rare subtype of non-small cell lung cancer (NSCLC). It features large, undifferentiated cells that make it challenging to identify under a microscope. This cancer grows faster and spreads earlier than many other NSCLC subtypes, making it more aggressive. Historically, it accounted for about 10% of lung cancer cases. However, recent data shows it now represents only 2.3% of all lung carcinomas. Understanding this rare condition helps you recognize its significance in lung cancer classification and its impact on patient outcomes.
Key Takeaways
Large-cell lung carcinoma is a rare and fast-growing lung cancer. It makes up only 2.3% of all lung cancer cases. Finding it early helps improve chances of recovery.
Smoking is the main cause of large-cell lung carcinoma. Staying away from cigarettes and harmful chemicals can lower your risk a lot.
Doctors use imaging, biopsies, and special tests to diagnose this cancer. These tests help confirm the cancer type and plan treatment.
Treatments depend on the cancer stage and type. Options include surgery, chemotherapy, and special targeted medicines. Custom treatment plans work best.
Learn about new research and treatments. Regular check-ups and early care can greatly improve survival chances.
Overview of Large-cell Lung Carcinoma
Characteristics
Large-cell lung carcinoma stands out due to its unique cellular structure and behavior. You can identify it as an undifferentiated non-small cell carcinoma that lacks the distinct features of small cell carcinoma. These tumors are often large, exceeding 5 cm in size, and bulky, typically located in the peripheral regions of the lung. Microscopically, the cells appear large with round to irregular nuclei and prominent nucleoli. They tend to grow in aggregates or sheets, often accompanied by areas of necrosis. This type of cancer grows rapidly and spreads early through lymphatic and blood vessels, making it highly aggressive.
Prevalence and Risk Factors
Although large-cell lung carcinoma accounts for about 9% of all lung cancers, its prevalence varies across regions and populations. For example, in 2020, South-Eastern Asia reported the highest incidence rates among males and females, with age-standardized rates (ASR) of 11.0 and 3.4 per 100,000 person-years, respectively. By 2022, North Africa and Northern Europe showed the highest ASRs for males and females at 4.33 and 2.87 per 100,000 people.
Several factors increase your risk of developing this cancer. Smoking remains the leading cause. Living with someone who smokes also raises your risk. Exposure to harmful substances like radon, asbestos, and chromium, as well as air pollution, can further contribute to its development.
Comparison with Other Lung Cancers
Large-cell lung carcinoma differs significantly from other types of lung cancer, such as adenocarcinoma or squamous cell carcinoma. Unlike these cancers, large-cell carcinoma lacks the specific morphological traits that define adenocarcinoma or squamous cell carcinoma. Its diagnosis often requires a resected specimen, as smaller biopsy samples may not provide enough information. Immunohistochemical testing can sometimes reveal similarities to poorly differentiated adenocarcinomas or squamous cell carcinomas, but large-cell carcinoma remains distinct due to its undifferentiated nature and aggressive behavior.
Classification of Large-cell Lung Carcinoma
WHO Classification
The World Health Organization (WHO) classifies large-cell lung carcinoma as a poorly differentiated subtype of non-small cell lung cancer (NSCLC). This classification excludes cancers with specific features of adenocarcinoma, squamous cell carcinoma, or small cell carcinoma. You can only confirm this diagnosis through resection specimens, as smaller biopsy samples may not provide enough detail.
The WHO also identifies several subtypes of large-cell lung carcinoma based on histological characteristics. These include large cell neuroendocrine carcinoma, basaloid carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma, and large cell carcinoma with rhabdoid phenotype. Each subtype has unique features that help pathologists differentiate them during diagnosis.
Subtypes
Large-cell lung carcinoma consists of multiple subtypes, each with distinct traits. The table below highlights these subtypes and their descriptions:
Subtype | Description |
|---|---|
Large Cell Neuroendocrine Carcinoma | A subtype with neuroendocrine features, often aggressive in nature. |
Basaloid Carcinoma | Resembles cutaneous basal cell carcinoma, typically found in proximal bronchi. |
Lymphoepithelioma-like Carcinoma | Contains large tumor cells with lymphocytic infiltration, similar to nasopharyngeal variant. |
Clear Cell Carcinoma | Characterized by clear or foamy cytoplasm, often containing glycogen. |
Large Cell Carcinoma with Rhabdoid Phenotype | Rare variant with rhabdoid appearance and eosinophilic globules in the cytoplasm. |
Understanding these subtypes helps you recognize the diversity within large-cell lung carcinoma and its varying clinical behaviors.
Molecular Features
Molecular studies have revealed several key features of large-cell lung carcinoma. One significant finding is the presence of the LKB1 mutation, which may play a role in the cancer's development. Other common genetic mutations include TP53, FAM135B, FAT3, and RB1. For example, TP53 mutations occur in 57% of cases, while FAM135B mutations appear in 35%. These mutations often correlate with tobacco exposure, as shown by the high frequency of C > A mutations in affected individuals.
Immunohistochemical testing also provides valuable insights. Large-cell lung carcinoma typically shows positive staining for markers like keratin 7 and epithelial membrane antigen (EMA). However, it often tests negative for TTF-1, p63, and keratin 5/6. These molecular features distinguish it from other NSCLC subtypes and guide treatment decisions.
Diagnostic Criteria for Large-cell Lung Carcinoma
Clinical and Radiologic Features
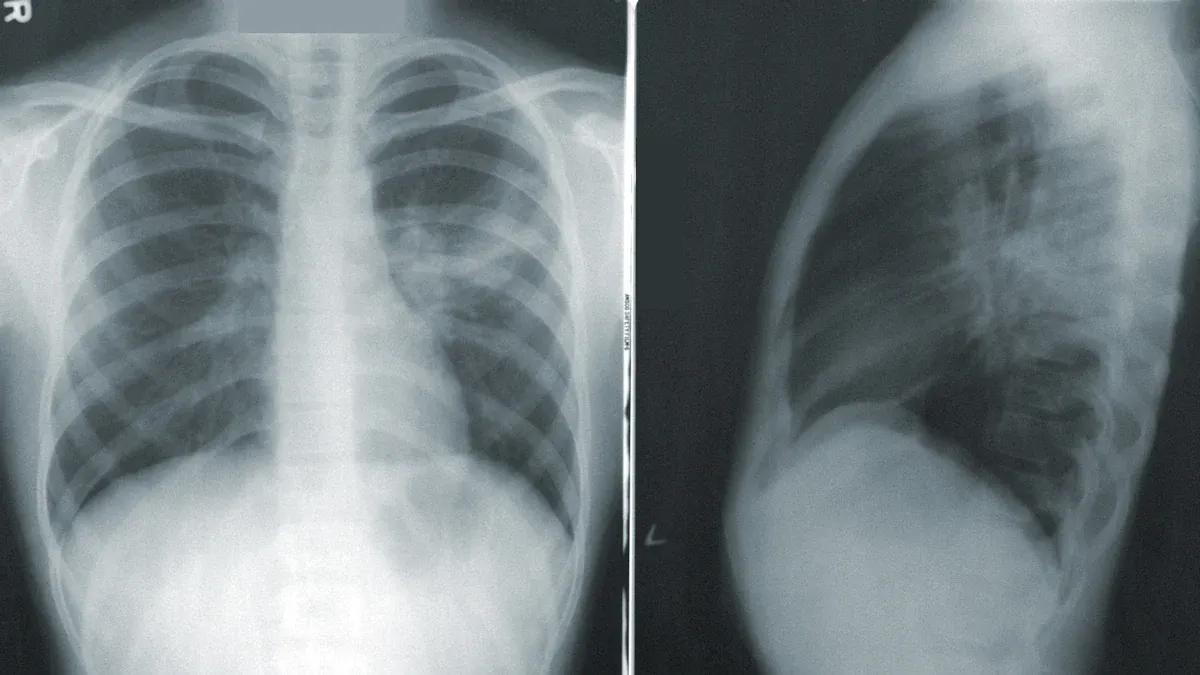
When diagnosing large-cell lung carcinoma, you may notice symptoms similar to other non-small cell lung cancers. These include a persistent cough, chest pain, shortness of breath, and unexplained weight loss. Radiologic imaging often reveals a mass larger than 4 cm, typically located in the peripheral regions of the lung. However, the basaloid variant may appear centrally. Other findings, such as mediastinal adenopathy or pneumonia, might also be present.
Feature Type | Description |
|---|---|
Clinical Features | Similar to other non-small cell lung cancers (NSCLCs) |
Radiologic Features | Mass usually larger than 4 cm |
Most cases are peripheral lung masses | |
Basaloid variant tends to be centrally located | |
Mediastinal adenopathy and pneumonia may be present |
Despite these findings, imaging alone cannot confirm the diagnosis. Large-cell lung carcinoma often requires further testing due to its overlapping features with other NSCLC subtypes.
Histological Diagnosis
Histological analysis plays a critical role in diagnosing large-cell lung carcinoma. You will find that immunohistochemical testing is essential, especially when the tumor lacks clear differentiation. Pathologists assess specific markers to rule out other NSCLC subtypes. For example:
Positive squamous markers (p40, CK5/6) and negative adenocarcinoma markers (TTF-1, napsin A) suggest nonkeratinizing squamous cell carcinoma.
Positive adenocarcinoma markers and negative squamous markers indicate adenocarcinoma, solid subtype.
A diagnosis of large-cell carcinoma is made when both marker types are negative.
This cancer is defined as an undifferentiated NSCLC without features of adenocarcinoma or squamous cell carcinoma. However, you should note that a definitive diagnosis requires a thoroughly sampled resected tumor. Small biopsy specimens or cytology samples often lack the necessary detail, leading to potential misclassification.
Molecular Testing
Molecular testing has become a cornerstone in diagnosing large-cell lung carcinoma. This testing identifies genetic mutations, such as TP53 or LKB1, which are common in poorly differentiated NSCLCs. By analyzing the tumor's molecular profile, you can confirm the diagnosis and guide treatment planning. For instance, molecular profiling helps detect mutations like EGFR or ALK, which may qualify patients for targeted therapies. These therapies often outperform traditional chemotherapy, offering better outcomes and fewer side effects.
Molecular testing not only aids in diagnosis but also personalizes treatment. This approach ensures that therapies align with the tumor's unique genetic characteristics, improving the effectiveness of care.
Prognosis and Treatment of Large-cell Lung Carcinoma
Prognosis by Subtype
The prognosis for large-cell lung carcinoma varies depending on its subtype. Some subtypes are more aggressive, leading to worse outcomes. The table below highlights the prognosis for different subtypes:
Subtype | Prognosis |
|---|---|
Classic large cell carcinoma | Relatively poor prognosis |
Large cell neuroendocrine carcinoma | Poorer prognosis than classic |
Giant cell carcinoma | Worse outcomes than classic |
Rhabdoid phenotype | Associated with aggressive behavior |
Basaloid variant | Worse prognosis than classic |
Large-cell lung carcinoma generally has a poorer prognosis compared to other non-small cell lung cancers. Its aggressive nature and tendency to metastasize early significantly impact survival rates. For example, the 5-year relative survival rate for localized cases is 63.1%, but this drops to 6.9% for distant-stage diagnoses.
Treatment Options
Treatment for large-cell lung carcinoma depends on the stage and subtype. Common options include:
Treatment Option | Description |
|---|---|
Surgery | Removes all or part of the tumor, often used for early-stage cases. |
Chemotherapy | Uses drugs to kill cancer cells throughout the body. |
Targeted therapy | Focuses on specific genetic mutations in cancer cells. |
Radiation therapy | Uses high-energy rays to destroy cancer cells. |
Immunotherapy | Boosts your immune system to fight cancer. |
Additional options | Includes laser therapy, cryosurgery, and electrocautery for specific cases. |
Targeted therapies and immunotherapies have shown promise in improving outcomes. For example, biomarker testing can identify genetic mutations like RET, allowing for personalized treatments such as selpercatinib.
Advances in Research
Recent research has led to significant advancements in treating large-cell lung carcinoma. Some promising developments include:
A 2023 clinical trial showed that selpercatinib improved progression-free survival in patients with RET mutations.
Immunotherapies like atezolizumab and pembrolizumab have been approved as adjuvant treatments after surgery for early-stage cases.
Nivolumab combined with chemotherapy before surgery has demonstrated longer survival compared to chemotherapy alone.
The FDA approved pembrolizumab with chemotherapy before surgery, followed by pembrolizumab post-surgery, leading to better outcomes.
These advancements highlight the importance of genetic testing and personalized treatment approaches in improving survival rates.
Large-cell lung carcinoma represents a poorly differentiated form of non-small cell lung cancer. It lacks the defining features of adenocarcinoma, squamous cell carcinoma, or small-cell carcinoma, making it a heterogeneous entity. Advances in immunohistochemistry and molecular profiling have refined its classification, aiding in more personalized care. Early diagnosis plays a vital role in improving outcomes, as survival rates drop significantly with advanced stages. For instance, patients diagnosed at stage IA have a 5-year survival rate exceeding 90%, compared to less than 10% for stage IV. Staying informed about new treatments and seeking timely medical advice can make a significant difference in managing this aggressive cancer.
FAQ
What makes large-cell lung carcinoma different from other lung cancers?
Large-cell lung carcinoma stands out due to its undifferentiated cells and aggressive behavior. Unlike adenocarcinoma or squamous cell carcinoma, it lacks specific features. Its rapid growth and early spread make it more challenging to treat.
Can large-cell lung carcinoma be prevented?
You can reduce your risk by avoiding smoking and secondhand smoke. Limiting exposure to harmful substances like radon or asbestos also helps. Regular health check-ups and a healthy lifestyle further lower your chances.
How is large-cell lung carcinoma diagnosed?
Doctors use imaging tests, biopsies, and molecular testing to diagnose this cancer. Imaging reveals the tumor's size and location. Biopsies confirm its undifferentiated nature, while molecular testing identifies genetic mutations for targeted treatment.
Is large-cell lung carcinoma treatable?
Yes, treatment options include surgery, chemotherapy, radiation, and immunotherapy. Early-stage cases respond better to surgery. Advanced stages often require a combination of therapies, including targeted treatments based on genetic testing.
What should you do if you suspect symptoms?
If you notice persistent cough, chest pain, or unexplained weight loss, consult a doctor immediately. Early diagnosis improves outcomes. Don't ignore symptoms, even if they seem minor.
Tip: Keep track of any unusual symptoms and share them with your healthcare provider for timely evaluation.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Key Molecular Characteristics of Lung Giant Cell Carcinoma
Understanding Anaplastic Large Cell Lymphoma Treatment Options
A Comprehensive Guide to Diffuse Large B-Cell Lymphoma
Essential Information on Basaloid Squamous Cell Lung Carcinoma

