What Are the Legal and Ethical Considerations in Cancer Prevention?
Facts Verified: February 2026
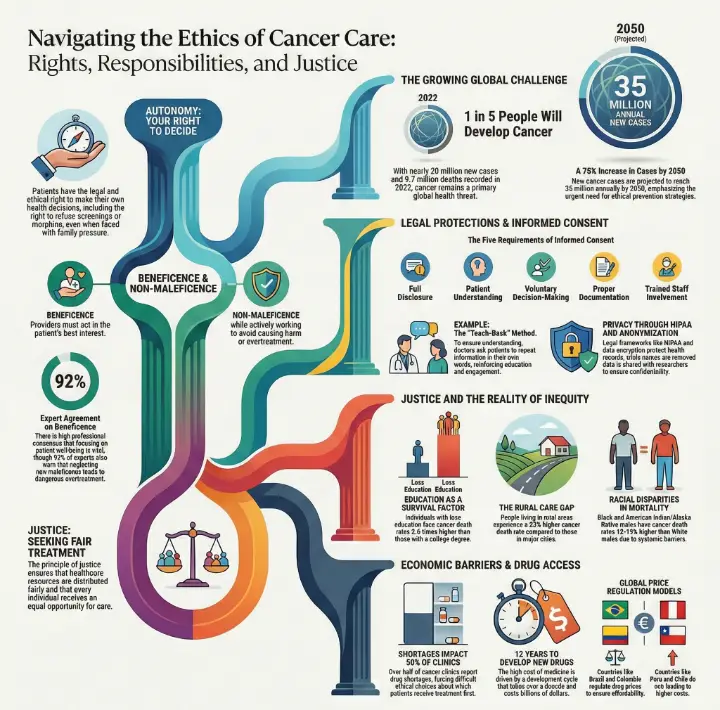
You face important choices when it comes to cancer prevention and care. Four key ethical principles guide these choices: autonomy, beneficence, non-maleficence, and justice. Autonomy means you have the right to make your own health decisions. Beneficence asks everyone to act in your best interest, while non-maleficence means avoiding harm. Justice makes sure everyone gets fair treatment.
Cancer affects many lives:
In 2022, nearly 20 million people learned they had cancer, and 9.7 million died from it.
About 1 in 5 people will develop cancer at some point.
New cases could reach 35 million by 2050, showing why prevention matters.
How It Impacts Care | Agreement Among Experts | |
|---|---|---|
Beneficence | Too much focus can cause overtreatment | 92% |
Non-maleficence | Not enough focus can cause overtreatment | 92% |
Justice | Ignoring it can cause undertreatment | 85% |
Informed consent, privacy, and fairness help protect your rights and keep care safe. These ideas form the base of Legal and Ethical Considerations in Cancer Prevention.
Key Takeaways
Understand your right to make health choices. Autonomy empowers you to decide on screenings and treatments.
Informed consent is crucial. Always seek clear information about your diagnosis and treatment options before agreeing to anything.
Healthcare providers must balance beneficence and non-maleficence. They aim to help you while avoiding harm, even when choices are tough.
Justice in healthcare means everyone deserves fair treatment. Support policies that promote equal access to cancer care for all.
Privacy laws protect your health information. Trust that your records are safe and only shared with authorized individuals.
Legal and Ethical Considerations in Cancer Prevention

Autonomy in Cancer Care
You have the right to make choices about your own health. Autonomy means you decide what happens to your body. In cancer prevention, this can include saying yes or no to screenings or treatments. Sometimes, families or doctors may want something different for you. For example, Mrs. A wanted to refuse morphine, but her family pressured her to accept it. This shows how hard it can be to respect your wishes when others have strong opinions.
Healthcare providers work to support your autonomy. They use decision aids to help you understand your options. They talk with you to make sure you know the risks and benefits. Good communication helps you feel confident in your choices. In some cultures, families may ask doctors not to tell patients about a cancer diagnosis. For example, Sara’s uncle wanted to keep her illness a secret. This can create a conflict between respecting your wishes and following family traditions.
Note: Patient-centered decision-making is key. You should always have a voice in your care, even when it feels difficult.
Beneficence and Non-Maleficence
Doctors and nurses want to help you. Beneficence means they act in your best interest. Non-maleficence means they avoid causing harm. These two ideas guide every step in cancer prevention and treatment. Sometimes, these principles can conflict. For example, you might choose to skip a recommended therapy for early-stage breast cancer. Your doctor may worry this choice could harm you, but you have the right to decide.
Here is how these principles affect your care:
Evidence Description | Impact on Patient Outcomes |
|---|---|
Quality measures help doctors use best practices. | You get care that maximizes benefits and reduces harm. |
Doctors ask about your pain to improve your quality of life. | Your comfort and well-being are a priority. |
Pain management prevents suffering during treatment. | You tolerate treatment better and feel less pain. |
Doctors avoid harm to build trust. | You feel safe and supported in your care. |
Doctors sometimes face tough choices. They must balance your wishes with what they believe is best for your health. During the COVID-19 pandemic, doctors had to decide who would get treatment first when resources were limited. They tried to protect vulnerable patients, but some treatments were delayed. This shows how hard it can be to apply beneficence and non-maleficence in real life.
Many patients delay or avoid treatment because of cost.
Only 31% of doctors screen for financial distress.
Doctors struggle to balance the best care with what you can afford.
Justice and Equity
Justice means everyone gets fair treatment. Equity means removing barriers so all people have the same chance for good health. In cancer prevention, not everyone has equal access to care. Some groups face higher risks and worse outcomes. For example:
Black and American Indian/Alaska Native males have cancer death rates 13-14% higher than White males.
People with less education have cancer death rates 2.6 times higher than those with a college degree.
People in rural areas have a 23% higher cancer death rate than those in big cities.
Social factors like income, education, and where you live affect your cancer risk. If you have low income or no health insurance, you may not get screened or treated early. Environmental problems, like poor air or water, can also raise your risk.
"The American Society of Clinical Oncology calls for policy changes to remove barriers to cancer care. They support expanding Medicaid and new payment models to help at-risk groups."
"The AACR says we need many solutions to end racism and other barriers in cancer prevention and care."
"ACS CAN wants all Americans to have access to quality cancer care, no matter their background."
Doctors and health leaders must think about justice when making decisions. Sometimes, they must choose between funding cancer prevention or other health needs, like infant care. This can be a hard choice, but fairness should always guide the decision.
You may face challenges if you belong to a group that has less access to care. Healthcare systems must work to remove these barriers. Legal and Ethical Considerations in Cancer Prevention help make sure everyone gets a fair chance to stay healthy.
Informed Consent and Confidentiality
Informed Consent Basics
You deserve to know what will happen during cancer prevention and care. Informed consent means you get clear information before you agree to any test or treatment. Doctors must explain your diagnosis, the recommended procedure, and any risks or benefits. You also learn about other options and what could happen if you choose not to get treatment. This process helps you make the best choice for your health.
Requirement | Description |
|---|---|
Disclosure of Information | You receive enough details about your diagnosis and choices. |
Understanding | You understand the risks and benefits. |
Voluntariness | You decide freely, without pressure. |
Documentation | Your consent is recorded, often with a signed form. |
Staff Roles | Only trained staff can ask for your consent. |
Ethical guidelines remind doctors that you may feel scared or confused. They must use simple words and check that you understand. For example, many doctors use the Teach-Back method.
The Teach-Back method is an effective strategy for confirming patient understanding of health information. It reinforces education by ensuring that patients can articulate what they have learned, thus enhancing their engagement in cancer care.
If a doctor skips these steps, you may not know all your choices. This can lead to legal problems, such as lawsuits or even criminal charges, if you suffer harm because you did not get the right information.
Protecting Privacy
Your health information is private. Laws like HIPAA protect your records and limit who can see them. Hospitals use strong security controls and data encryption to keep your information safe. They remove your name and other details before sharing data with researchers. Only approved people can access your records.
Privacy Measure | Description |
|---|---|
Federal Privacy Rules | Laws protect your personal information. |
Security Controls | Experts monitor systems to prevent leaks. |
Data Anonymization | Your identity is hidden in shared data. |
Access Limitation | Only trusted staff and researchers see your data. |
Certificates of Confidentiality | Extra legal protection for sensitive information. |
You can trust that Legal and Ethical Considerations in Cancer Prevention include strong rules to keep your information safe. These steps help you feel secure when you take part in cancer prevention programs.
Addressing Costs and Access

Drug Costs and Shortages
You may notice that cancer drugs can cost a lot, and sometimes they are hard to find. These problems affect your care and the care of many others. Prices for cancer medicines change from country to country. For example:
Colombia and Brazil control drug prices, making them more affordable.
Peru and Chile do not regulate prices, so medicines cost more.
Mexico uses a mixed system, which can make some drugs expensive.
In some countries, high prices do not match what people can afford.
Drug shortages also create big challenges. Over half of cancer clinics have reported that shortages made it hard to give the best care. Many clinics had to make tough choices, like deciding who gets treatment first. Some switched to less effective drugs or spent more money to find alternatives.
Cause | Description |
|---|---|
Manufacturing Issues | Problems in making drugs can reduce supply. |
Supply Chain Disruptions | Trouble moving drugs from factories to clinics can cause shortages. |
Regulatory Delays | Slow approval of new drugs keeps them off the market. |
Market Dynamics | Few suppliers and low prices can make shortages worse. |
Developing new cancer drugs takes about 12 years and costs billions of dollars. This makes medicines expensive. Cancer centers now use waste management and adjust doses to stretch supplies. Some experts suggest tax breaks and grants to help make more generic drugs and keep prices down.
Equity for Marginalized Groups
You deserve fair access to cancer prevention, no matter your background. Many people face barriers because of language, money, or where they live. Some groups, like non-Hispanic Blacks, have higher cancer death rates because they do not get the same care. Structural racism and low income make it harder to get screened or treated.
Barrier Type | Description |
|---|---|
Informed Consent Process | Patients with limited English may not understand their choices. |
Financial Resources | Lack of money for translated forms can stop people from joining studies. |
Health Literacy | Not knowing enough about health can keep people from making good decisions. |
Community programs that use local leaders and offer information in many languages help more people get screened. Telehealth and free services also make it easier for people in rural or low-income areas to get care. When you have health insurance, you are more likely to get screened and treated early. Recent changes in laws may make it harder for some to keep their coverage, which could delay diagnosis and treatment.
Legal and Ethical Considerations in Cancer Prevention remind us that everyone should have a fair chance to stay healthy. You can help by supporting policies that make care more equal for all.
You play an important role in cancer prevention. Four ethical principles—autonomy, beneficence, non-maleficence, and justice—guide your choices and protect your rights. Informed consent, privacy, and equity help you trust your care team and make good decisions.
Ethical cancer care focuses on helping marginalized groups and supports dignity for everyone.
Strong privacy rules and fair access to information build trust and improve outcomes.
AI in cancer care must be transparent and fair to support your autonomy and safety.
You can make better choices when you understand these principles.
FAQ
What does autonomy mean in cancer prevention?
You have the right to make choices about your health. Autonomy lets you decide if you want screenings or treatments. Doctors must respect your wishes and help you understand your options.
Why is informed consent important?
You need clear information before any test or treatment. Informed consent protects your rights. It helps you make safe choices and keeps you in control of your care.
How do privacy laws protect my health information?
Privacy laws like HIPAA keep your health records safe. Hospitals use strong security to stop leaks. Only trusted staff can see your information. You can ask who has access.
What should you do if you cannot afford cancer drugs?
You can talk to your doctor about cheaper options. Some clinics offer help with costs. Community programs and insurance may cover some medicines. Ask about financial support.
How can you get fair cancer care if you belong to a marginalized group?
You can look for clinics with language help or free screenings. Community leaders often share resources. Telehealth and insurance programs can improve access. Support groups also help you find care.
This article is for educational purposes only and is not a substitute for professional medical advice. For more details, please see our Disclaimer. To understand how we create and review our content, please see our Editorial Policy.
See Also
An In-Depth Overview of Various Cancer Types
Essential Information About Carcinoid Tumors You Need
Recognizing Symptoms and Causes Associated With Anal Cancer
Key Characteristics and Behavior of Mammary Secretory Carcinoma
Important Facts Regarding Basaloid Squamous Cell Lung Carcinoma

