Understanding Malignant Peripheral Nerve Sheath Tumors
A malignant peripheral nerve sheath tumor is a rare and aggressive cancer that forms in the protective lining of your nerves. This type of tumor accounts for 5–10% of soft tissue sarcomas, which are themselves uncommon. Early detection plays a critical role in improving outcomes, as these tumors grow quickly and can spread to other parts of your body. You may face a higher risk if you have neurofibromatosis type 1 (NF1), a genetic condition linked to these tumors. Understanding this connection can help you stay vigilant and seek timely medical advice.
Key Takeaways
Malignant peripheral nerve sheath tumors (MPNST) are fast-growing cancers. They form in the covering of nerves. Finding them early helps improve treatment success.
People with neurofibromatosis type 1 (NF1) have a higher chance of getting MPNST. Regular check-ups can help find these tumors early.
Signs of MPNST include pain, swelling, and numbness near the tumor. If you have these symptoms, see a doctor quickly.
Surgery is the main way to treat MPNST. Doctors try to remove the whole tumor. This helps people live longer and lowers the chance of it coming back.
New treatments like targeted therapies and immunotherapy look hopeful for MPNST. Joining clinical trials may give access to these new treatments.
What Are Malignant Peripheral Nerve Sheath Tumors?
Definition and Overview
A malignant peripheral nerve sheath tumor is a type of soft tissue sarcoma that forms in the protective covering of your nerves. These tumors often appear as a growing mass in the soft tissues of your body. They may cause pain, swelling, or other neurological symptoms. In some cases, you might notice numbness or tingling near the affected area. These tumors can develop in any part of the body but are most commonly found in the arms, legs, or trunk.
Doctors often identify these tumors through imaging tests like MRI or PET/CT scans. On these scans, malignant peripheral nerve sheath tumors typically show irregular shapes, invasive edges, and higher metabolic activity compared to benign tumors. These characteristics help distinguish them from other nerve-related growths.
How MPNST Develops
Malignant peripheral nerve sheath tumors usually arise from pre-existing benign nerve tumors, such as plexiform neurofibromas. This transformation is more common in individuals with genetic conditions like neurofibromatosis type 1 (NF1). If you have NF1, you may already have multiple benign tumors, which increases your risk of developing MPNST.
These tumors grow when genetic mutations cause nerve cells to divide uncontrollably. Over time, the tumor invades nearby tissues, leading to symptoms like pain or loss of function. In some cases, the tumor may spread to other parts of your body, such as the lungs, through a process called metastasis.
Why MPNST Is Considered Aggressive
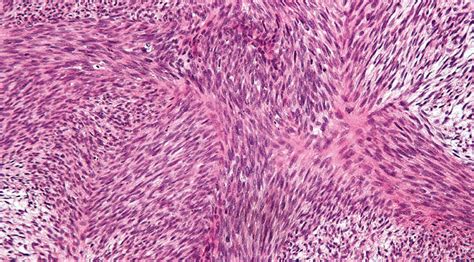
Malignant peripheral nerve sheath tumors are aggressive because they grow quickly and invade surrounding tissues. They often have irregular, locally invasive margins, making complete surgical removal challenging. These tumors also show high cellular activity, with features like spindle-shaped cells and increased mitotic figures, which indicate rapid division.
You might experience worsening symptoms as the tumor grows, such as persistent pain or difficulty moving the affected area. If left untreated, the tumor can spread to distant organs, significantly reducing survival rates. Early detection and treatment are crucial to managing this aggressive cancer effectively.
Symptoms of Malignant Peripheral Nerve Sheath Tumors
Common Symptoms
Pain or tenderness near the tumor site
You might notice pain or tenderness in the area where the tumor is growing. This discomfort often starts as mild but can worsen over time. The pain may feel sharp or dull, depending on the tumor's location and size.
Swelling or a noticeable lump
A malignant peripheral nerve sheath tumor often causes swelling or a lump that you can feel under your skin. This lump may grow quickly, making it more noticeable. If the tumor is near a joint, the swelling might limit your movement.
Numbness or weakness in the affected area
As the tumor presses on nearby nerves, you could experience numbness or weakness. This might make it harder to perform everyday tasks, especially if the tumor is in your arm or leg.
Advanced Symptoms
Difficulty moving the affected limb
When the tumor grows larger, it can interfere with your ability to move the affected limb. This happens because the tumor compresses nerves or muscles, reducing their function.
Persistent or worsening pain
Pain that doesn’t go away or gets worse over time is a common sign of advanced MPNST. This pain might spread to other areas, depending on the tumor's location.
Systemic symptoms like fatigue or weight loss
In advanced stages, you might feel unusually tired or notice unexplained weight loss. These symptoms occur as your body struggles to cope with the tumor's effects.
Other advanced signs include:
A rapidly growing mass in soft tissue
New neurological symptoms like tingling or burning sensations
Enlargement of a pre-existing neurofibroma, which could signal malignant transformation
Changes in Nerve Function
Tingling or numbness
You might feel tingling or "pins and needles" in the area near the tumor. This sensation occurs when the tumor irritates or compresses nearby nerves.
Loss of sensation in the affected area
In some cases, you could lose feeling entirely in the area around the tumor. This happens when the tumor damages the nerves responsible for sensation.
Causes and Risk Factors
Genetic Factors
The role of neurofibromatosis type 1 (NF1)
If you have neurofibromatosis type 1 (NF1), your risk of developing a malignant peripheral nerve sheath tumor increases significantly. NF1 occurs due to mutations in the NF1 tumor suppressor gene, which disrupts the function of neurofibromin, a protein that helps regulate cell growth. This disruption activates the RAS/RAF/MEK/ERK pathway, leading to uncontrolled cell proliferation. About 10% of individuals with NF1 develop MPNSTs, often near pre-existing neurofibromas. Staying aware of this connection can help you monitor for early signs of malignant transformation.
Other genetic mutations linked to MPNST
Several other genetic mutations contribute to the development of MPNSTs. These include:
Bi-allelic NF1 inactivation or mutation, which is essential for MPNST formation.
CDKN2A loss, commonly found in atypical neurofibromas and low-grade MPNSTs.
EGFR, SUZ12, and TP53 mutations, which are present in MPNSTs but not in benign plexiform neurofibromas.
These mutations highlight the complex genetic landscape of MPNSTs and underscore the importance of genetic testing in understanding your risk.
Environmental and Lifestyle Factors
Prior radiation therapy as a risk factor
Radiation therapy, especially when administered during childhood or for previous cancers, increases your risk of developing MPNSTs. Radiation can damage DNA in nerve cells, leading to mutations that may trigger tumor growth. If you have undergone radiation treatment, regular follow-ups with your healthcare provider can help detect any abnormalities early.
Other potential contributors, such as exposure to carcinogens
Exposure to certain environmental carcinogens, such as industrial chemicals or pollutants, may also play a role in MPNST development. Although these factors are less well-defined, reducing your exposure to harmful substances can lower your overall cancer risk. Maintaining a healthy lifestyle and avoiding known carcinogens can support your long-term health.
How MPNST Affects Children
Rarity of MPNST in Children
Malignant peripheral nerve sheath tumors (MPNST) are extremely rare in children. These tumors account for only a small percentage of pediatric cancers. Their rarity makes them harder to recognize, often leading to delayed diagnosis. This delay can complicate treatment and reduce the chances of successful outcomes. If your child has neurofibromatosis type 1 (NF1), the risk of developing MPNST increases, making regular monitoring essential.
Unique Challenges in Pediatric Cases
Diagnosis and Early Detection
Diagnosing MPNST in children presents unique challenges. The symptoms often mimic those of other conditions, making early detection difficult. You may notice swelling, pain, or weakness in your child, but these signs can overlap with other benign conditions. Doctors rely on advanced diagnostic tools to identify MPNST accurately.
Description | |
|---|---|
Imaging Studies | MRI and PET/CT scans detect abnormalities in nerves, showing tumor size and location. |
Biopsy | Tissue samples confirm cancer presence, revealing specific cell features of MPNST. |
Genetic Testing | Identifies mutations in NF1 patients, highlighting increased cancer risk. |
Early detection improves treatment options. If your child has NF1, regular imaging and genetic testing can help catch changes before they progress.
Treatment Considerations for Growing Bodies
Treating MPNST in children requires a specialized approach. Pediatric cases often involve larger tumors, especially in NF1 patients, which makes surgical removal more challenging. A multidisciplinary team of surgeons, oncologists, and pediatric specialists works together to create a treatment plan.
Challenges in treatment include:
Differentiating MPNST from other tumors.
Managing the aggressive nature of the tumor.
Balancing treatment with the needs of a growing body.
Targeted therapies show promise but remain complex due to the tumor's behavior. Your child's care team will consider these factors to minimize long-term effects on growth and development.
Prognosis and Support for Families
Emotional and Psychological Support
A diagnosis of MPNST can be overwhelming for your family. You may feel anxious about your child’s future or uncertain about treatment options. Emotional support plays a critical role during this time. Counseling services and support groups can help you and your child cope with the challenges ahead.
Resources for Families Navigating Treatment
Navigating treatment requires access to reliable resources. Many organizations provide guidance, including financial assistance and educational materials. You can connect with groups like the Children’s Tumor Foundation or local cancer support networks. These resources offer valuable tools to help you manage your child’s care and find hope during difficult times.
Treatment Options for Malignant Peripheral Nerve Sheath Tumors

Surgical Treatment
Importance of complete tumor removal
Surgery is the primary treatment for a malignant peripheral nerve sheath tumor. Complete tumor removal, known as R0 resection, involves excising the tumor with clear margins of at least 2 cm. This approach significantly improves survival rates by reducing the risk of recurrence. Wide resection is especially important for high-grade tumors, as these are more likely to spread. Tumors located in the extremities, such as the arms or legs, often allow for better surgical outcomes compared to those in complex areas like the brachial plexus.
Challenges in surgery for MPNST
Removing the tumor entirely can be challenging due to its invasive nature. MPNSTs often grow into surrounding tissues, making it difficult to achieve clear margins. In areas with dense nerve networks, surgeons must balance tumor removal with preserving nerve function. For tumors in critical locations, achieving R0 resection may not always be possible, which can impact long-term outcomes. Despite these challenges, surgery remains a cornerstone of treatment, especially when combined with other therapies.
Radiation Therapy
When radiation is used
Radiation therapy plays a key role in managing large or high-grade MPNSTs. Doctors often recommend it for patients with positive margins after surgery or for those with unresectable tumors. It can also be used as a neoadjuvant therapy to shrink the tumor before surgery or as an adjuvant therapy to reduce the risk of local recurrence. While radiation improves local control, its effect on overall survival remains uncertain.
Potential side effects
Radiation therapy can cause side effects, including skin irritation, fatigue, and swelling in the treated area. Long-term effects may include damage to nearby healthy tissues or nerves. Your doctor will carefully plan the treatment to minimize these risks while maximizing its effectiveness.
Chemotherapy
Effectiveness of chemotherapy for MPNST
Chemotherapy is less effective for MPNST compared to other cancers. It is typically reserved for advanced cases where the tumor has spread or cannot be surgically removed. While it may not cure the disease, chemotherapy can help slow tumor growth and alleviate symptoms.
Common drugs used in treatment
Doctors often use drugs like doxorubicin and ifosfamide to treat MPNST. These medications target rapidly dividing cancer cells, but they can also affect healthy cells, leading to side effects such as nausea, fatigue, and a weakened immune system. Your healthcare team will monitor you closely to manage these effects and adjust the treatment as needed.
Emerging Treatments and Clinical Trials
Targeted therapies
Targeted therapies are showing promise for treating malignant peripheral nerve sheath tumors. These therapies focus on the molecular mechanisms driving tumor growth. One key pathway involved in these tumors is the Ras/Raf/MEK/ERK pathway. Researchers have developed inhibitors that target this pathway, and clinical trials are testing their effectiveness. Some patients have experienced complete responses to MEK inhibitors, which block signals that promote tumor growth.
These therapies are particularly important because malignant peripheral nerve sheath tumors often resist traditional chemotherapy. By addressing the specific genetic mutations and pathways involved, targeted therapies offer a more precise approach. Similar treatments have already succeeded in managing other tumors linked to neurofibromatosis type 1. This progress provides hope for improving outcomes in patients with this aggressive cancer.
Immunotherapy options
Immunotherapy is another emerging option for treating malignant peripheral nerve sheath tumors. This approach uses your immune system to fight cancer. Scientists are exploring ways to enhance your body's natural defenses against these tumors. For example, checkpoint inhibitors help your immune cells recognize and attack cancer cells more effectively.
Clinical trials are essential for advancing immunotherapy. If you are interested in participating, you can follow these steps:
Contact the research team to express your interest.
Undergo screening to confirm your eligibility for the study.
Provide your consent by signing a form that explains the study's purpose and procedures.
Participate by following the study's requirements as directed by the research team.
By joining a clinical trial, you can access cutting-edge treatments while contributing to medical research. Immunotherapy and targeted therapies represent exciting advancements in the fight against malignant peripheral nerve sheath tumors.
Understanding a malignant peripheral nerve sheath tumor can help you recognize its symptoms and risk factors early. This rare and aggressive cancer often grows quickly, making early detection critical. Many cases are only diagnosed after the tumor has metastasized, which complicates treatment. Regular monitoring, especially if you have known risk factors like neurofibromatosis type 1, allows for earlier detection and more effective treatment options. If you notice concerning symptoms, consult a healthcare professional promptly. Personalized guidance ensures you receive the best care and support throughout your journey.
FAQ
What is the difference between MPNST and benign nerve tumors?
Benign nerve tumors grow slowly and usually don’t spread. MPNST, on the other hand, grows quickly, invades nearby tissues, and can metastasize. You should consult a doctor if you notice rapid growth or worsening symptoms.
Can MPNST be prevented?
You cannot fully prevent MPNST, but regular monitoring helps. If you have neurofibromatosis type 1 (NF1), routine check-ups and imaging tests can detect changes early. Avoiding unnecessary radiation exposure may also reduce risk.
How is MPNST diagnosed?
Doctors use imaging tests like MRI or PET/CT scans to locate the tumor. A biopsy confirms the diagnosis by analyzing tissue samples. Genetic testing may also help if you have NF1 or other risk factors.
Is MPNST hereditary?
MPNST itself isn’t hereditary, but conditions like NF1, which increase your risk, are genetic. If you have a family history of NF1, genetic counseling can help you understand your risk.
What should you do if you suspect MPNST?
You should contact a healthcare provider immediately. Early detection improves treatment options. Keep track of symptoms like pain, swelling, or numbness, and share this information with your doctor.
See Also
Simplifying The Causes Of Gastrointestinal Stromal Tumors
Key Characteristics Of Glioblastoma: A Simple Overview
Craniopharyngioma: Key Features And What You Need To Know
Essential Information About Carcinoid Tumors You Should Know

