Mammary Secretory Carcinoma Explained: Key Traits and Behavior
Mammary secretory carcinoma is a rare and distinct type of breast cancer. It accounts for less than 0.15% of all breast cancer cases but represents 80% of childhood breast cancers. This condition features unique histological traits, such as tumor nests surrounded by stroma and eosinophilic secretions. Its genetic hallmark is the ETV6–NTRK3 gene fusion caused by a t(12;15)(p13;q25) translocation. Despite its rarity, mammary secretory carcinoma holds clinical significance due to its generally favorable prognosis. Early detection plays a crucial role in ensuring effective treatment and improved outcomes.
Key Takeaways
Mammary secretory carcinoma is a very rare breast cancer. It is less than 0.15% of cases but 80% of childhood breast cancers.
Finding it early is very important for better results. This cancer often has a good outcome if caught early.
The ETV6-NTRK3 gene fusion helps doctors identify this cancer. It makes this cancer different from other breast cancers.
Surgery is the main way to treat small tumors. New treatments are being studied for more serious cases.
Long-term care is very important to check for cancer returning. It also helps patients stay healthy and feel supported.
What Is Mammary Secretory Carcinoma?
A Rare Breast Cancer
Mammary secretory carcinoma is an uncommon type of breast cancer, accounting for less than 0.15% of all cases. Despite its rarity, it is the most prevalent form of breast cancer in children, representing 80% of childhood breast cancer diagnoses. The condition affects both males and females, though it is significantly more common in females, with a male-to-female ratio of approximately 1:6.
First described in 1966, this cancer was initially called juvenile breast carcinoma due to its frequent occurrence in young females. It typically presents as a painless, firm mass, often located in the outer upper quadrant of the breast. Histologically, it is distinguished by the presence of intracellular and extracellular secretory material, which contributes to its unique classification. These features, combined with its rarity, make mammary secretory carcinoma a distinct entity within the spectrum of breast cancers.
How It Differs from Other Breast Cancers
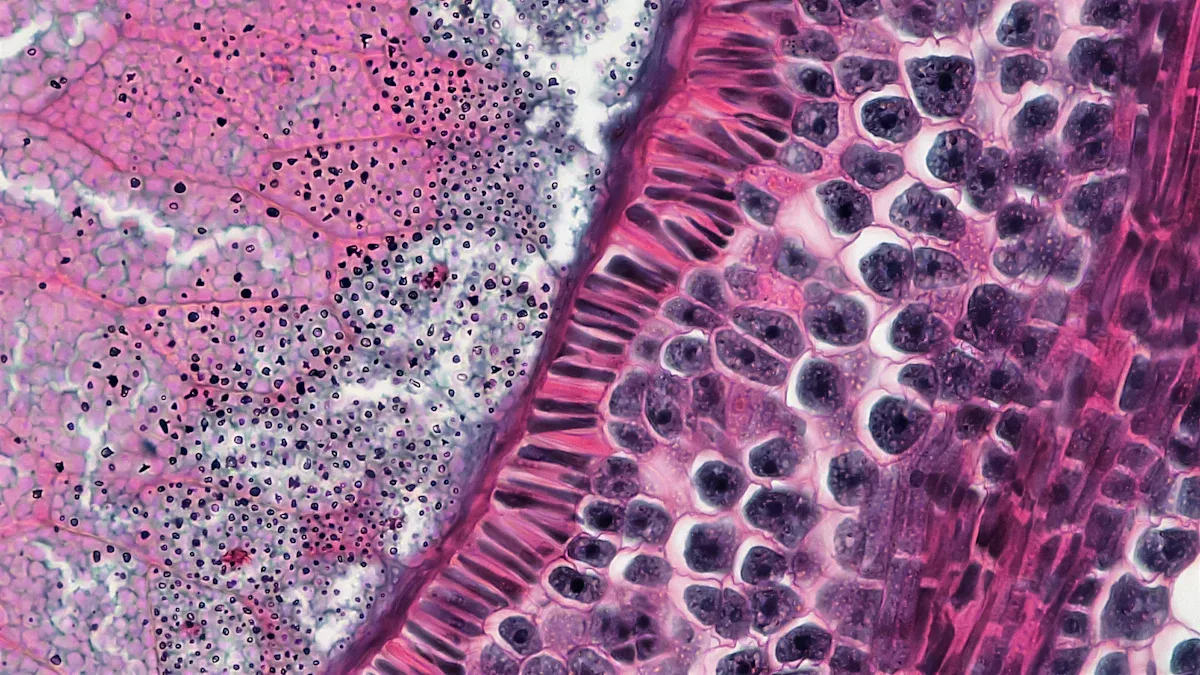
Mammary secretory carcinoma stands apart from other breast cancers in several ways. One of its defining characteristics is the presence of eosinophilic extracellular secretions, which are visible under H&E staining. This feature is not commonly observed in other types of breast cancer. Additionally, it is associated with a specific genetic alteration: the t(12;15)(p13;q25) translocation, which results in the ETV6–NTRK3 gene fusion. This genetic hallmark is a key factor in its diagnosis and sets it apart from other breast cancer subtypes.
Unlike many breast cancers, mammary secretory carcinoma often exhibits a triple-negative profile, meaning it lacks estrogen receptor (ER), progesterone receptor (PR), and HER2 expression. However, it does not share the aggressive behavior typically associated with other triple-negative breast cancers. Its mutational burden is also notably low, with few additional pathogenic mutations identified. These molecular and genetic differences highlight its distinct biological identity and influence its clinical management.
Key Characteristics of Mammary Secretory Carcinoma
Histological Features
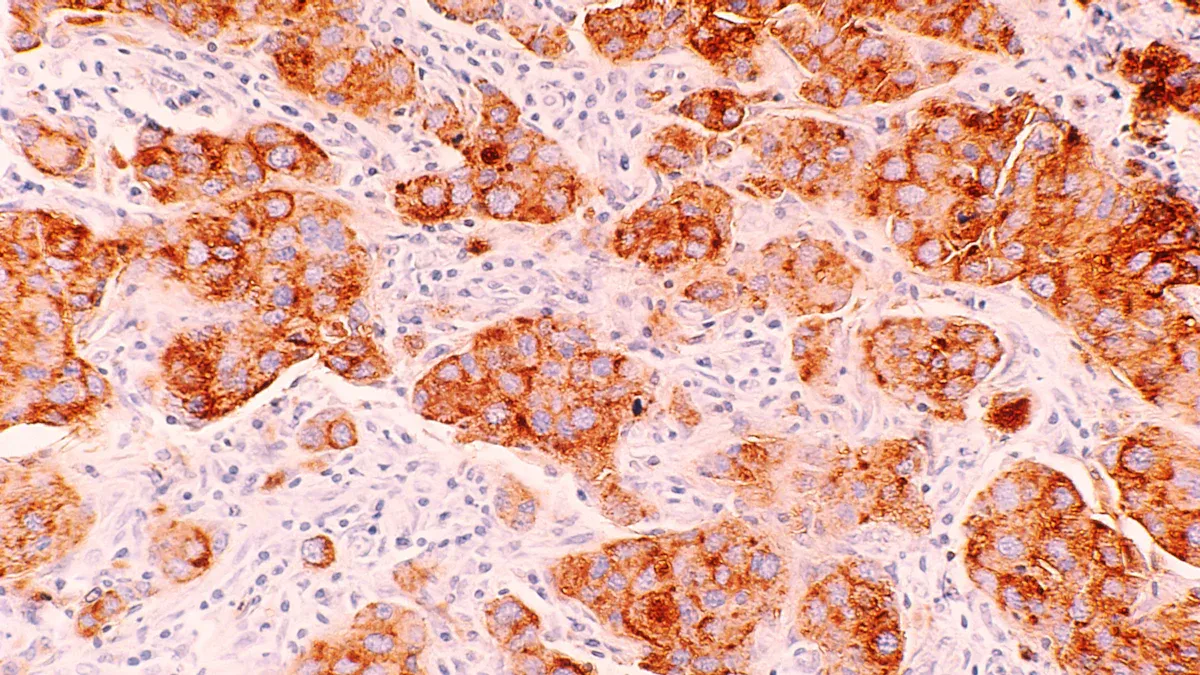
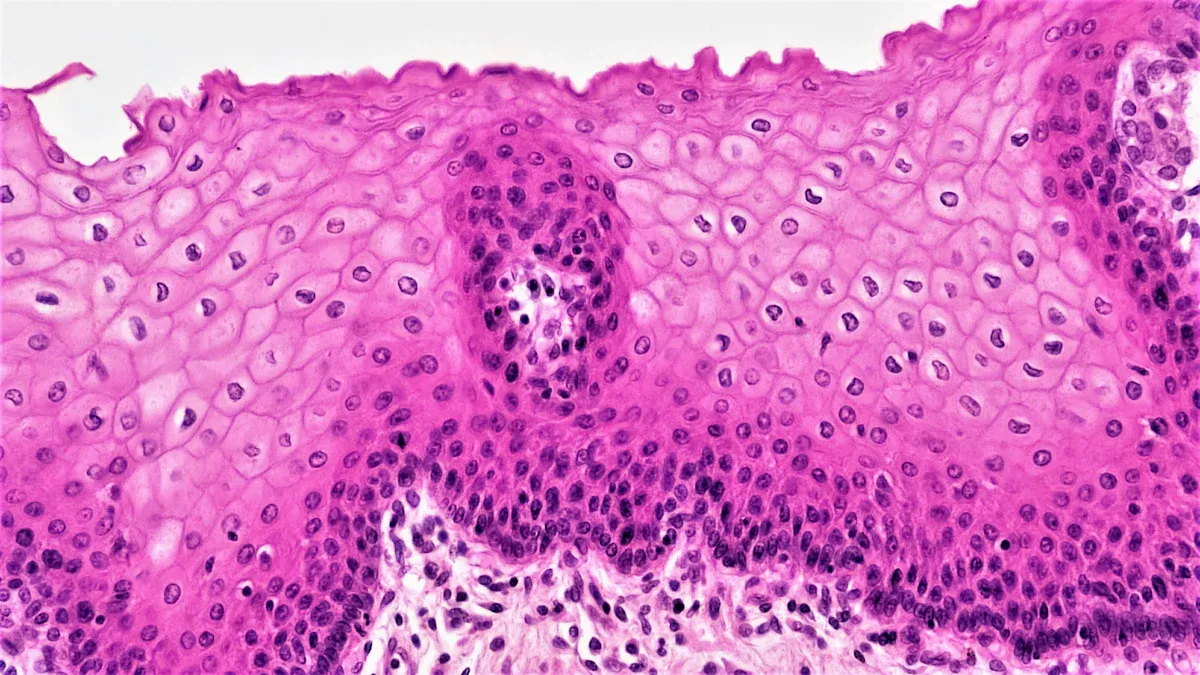
Mammary secretory carcinoma exhibits distinct histological traits that set it apart from other breast cancers. Tumors often display well-defined borders and are composed of cells arranged in nests, tubules, or microcystic patterns. These structures are surrounded by fibrous stroma, which provides a supportive framework. A hallmark feature is the presence of eosinophilic secretory material, both within the cells and in the extracellular spaces. This material stains positively with periodic acid-Schiff (PAS), aiding in its identification. The unique histological appearance of this cancer plays a crucial role in its diagnosis.
Molecular and Genetic Profile
The molecular and genetic profile of mammary secretory carcinoma is equally distinctive. The ETV6-NTRK3 gene fusion serves as a defining genetic marker. This fusion results from a t(12;15)(p13;q25) translocation and is not exclusive to breast secretory carcinomas. It also appears in similar tumors in other parts of the body, suggesting a shared genetic foundation. Additionally, tumors associated with this carcinoma express markers like MUC4 and SOX10. These markers, commonly found in salivary gland tumors, can assist in diagnosis and prompt further genetic testing. The molecular characteristics of mammary secretory carcinoma highlight its unique biological identity.
Imaging Characteristics
Imaging techniques play a vital role in identifying mammary secretory carcinoma. Magnetic resonance imaging (MRI) is particularly effective in detecting its specific features. For instance, MRI scans often reveal well-defined lesions with fibrous capsules. These lesions typically appear hypointense in most sequences but exhibit a hyperintense, heterogeneous signal in T2-weighted images. Intravenous contrast enhances the visualization, revealing papillary-like projections within the tumor. Such imaging characteristics help differentiate mammary secretory carcinoma from other breast cancers, aiding in accurate diagnosis and treatment planning.
Biological Behavior of Mammary Secretory Carcinoma
Growth Patterns
Mammary secretory carcinoma exhibits diverse growth patterns that reflect its unique histological features. Tumor cells often form nests surrounded by dense collagen stroma, creating a honeycomb-like appearance. These nests may display microcystic, glandular, or solid structures, with some regions showing papillary or tubular arrangements. Intracellular and extracellular secretory material, a hallmark of this cancer, fills these structures. In certain cases, irregular microcysts resembling thyroid follicles or dilated cysts containing eosinophilic secretions are observed. Tumor cells typically show mild-to-moderate atypia, with pale cytoplasm and small, round nuclei. Mitotic activity remains rare, indicating a relatively slow growth rate.
Metastasis and Spread
Mammary secretory carcinoma primarily spreads to nearby lymph nodes, particularly sentinel and axillary nodes. Studies indicate that approximately 29.3% of patients experience lymph node involvement. However, distant metastases are rare. Long-term follow-up has revealed isolated cases of metastasis to the bone, liver, or other distant sites. Despite its generally indolent nature, the potential for metastasis underscores the importance of vigilant monitoring. While most patients achieve favorable outcomes, a small number have succumbed to the disease, highlighting the need for early detection and comprehensive care.
Response to Treatment
Surgery remains the cornerstone of treatment for mammary secretory carcinoma. For localized tumors, conservative surgery or simple mastectomy is often sufficient. Radical mastectomy may be necessary for cases with unfavorable prognostic features. Chemotherapy and radiotherapy have shown limited effectiveness, particularly in metastatic cases. This has led to growing interest in targeted therapies, which may offer better outcomes for patients with advanced disease. The choice of treatment depends on the tumor's characteristics and the patient's overall health, emphasizing the need for personalized care.
Diagnosis and Treatment Options
Diagnostic Techniques
Diagnosing mammary secretory carcinoma involves a combination of clinical evaluation, imaging, and pathological analysis. Physicians typically begin with a physical examination to identify any palpable masses. Imaging techniques, such as mammography and ultrasound, help determine the size, shape, and location of the tumor. Mammography often reveals a well-defined mass, while ultrasound may show a hypoechoic lesion with irregular margins.
Pathological examination confirms the diagnosis. A core needle biopsy is the preferred method for obtaining tissue samples. Histological analysis identifies the characteristic features of mammary secretory carcinoma, such as eosinophilic secretory material and well-defined tumor borders. Immunohistochemistry plays a crucial role in detecting the ETV6-NTRK3 gene fusion, a genetic hallmark of this cancer. Additional tests, including periodic acid-Schiff (PAS) staining, further aid in distinguishing this carcinoma from other breast cancers.
Treatment Approaches
Treatment for mammary secretory carcinoma depends on the tumor's characteristics and the patient's overall health. Surgery remains the primary approach for managing localized tumors. Conservative surgery, such as simple mastectomy or lumpectomy, is recommended for patients with favorable prognoses. Sentinel lymph node biopsy is often performed alongside these procedures to assess lymph node involvement. For tumors with unfavorable features, radical mastectomy may be necessary.
Other treatment options include chemotherapy and radiotherapy, though their effectiveness is limited. These therapies are typically reserved for rare cases of metastasis, where they show minimal response. Emerging studies suggest that targeted drug therapy may offer better outcomes for metastatic tumors by addressing specific genetic alterations. Long-term follow-up care is essential for monitoring recurrences. Physicians recommend follow-up for at least 20 years after diagnosis to ensure early detection of any changes.
Treatment Type | Description |
|---|---|
Surgical removal | Considered the mainstay of treatment for localized MSC tumors. |
Conservative surgery | Recommended for patients with favorable prognoses, involving simple mastectomy and sentinel lymph node biopsy. |
Radical mastectomy | Used for tumors with unfavorable prognostic features. |
Chemotherapy and radiotherapy | Limited role; rare cases of metastasis show little to no response to these treatments. |
Targeted drug therapy | Emerging studies suggest this may be more effective for metastatic tumors. |
Long-term follow-up | Recommended for at least 20 years after diagnosis to monitor for recurrences. |
Prognosis and Long-Term Outlook
Survival Rates and Influencing Factors
Mammary secretory carcinoma generally has an excellent prognosis, with survival rates reflecting its indolent nature. Studies report the following survival statistics:
Overall survival (OS) rate: 76.3%
Five-year OS rate: 91.8%
Breast cancer-specific survival (BCSS) rate: 88%
Five-year BCSS rate: 97.8%
Long-term data further highlight the favorable outcomes:
Time Period | BCSS (%) | OS (%) |
|---|---|---|
5-year | 95.79 | 89.47 |
10-year | 93.16 | 81.58 |
20-year | 93.16 | 76.84 |
Several factors influence these outcomes. Early-stage diagnosis plays a pivotal role, as tumors detected early often exhibit mild clinicopathologic features. Treatment choices also impact survival. Breast-conserving surgery (BCS) combined with radiotherapy tends to yield better results compared to mastectomy. However, the role of systemic therapies, such as chemotherapy, remains unclear due to limited data. These factors underscore the importance of personalized treatment strategies tailored to each patient’s condition.
Importance of Follow-Up Care
Long-term follow-up care is essential for patients diagnosed with mammary secretory carcinoma. Although the prognosis is generally favorable, the potential for recurrence or late metastasis necessitates ongoing monitoring. Physicians recommend follow-up care for at least 20 years after diagnosis. Regular check-ups, imaging studies, and physical examinations help detect any changes early, ensuring timely intervention if needed.
Follow-up care also provides an opportunity to address the patient’s overall well-being. Emotional support, lifestyle guidance, and management of any treatment-related side effects contribute to improved quality of life. By maintaining a proactive approach, healthcare providers can help patients achieve the best possible outcomes while minimizing the risk of complications.
Mammary secretory carcinoma is a rare breast cancer with distinct traits and generally indolent behavior. Its defining features include well-circumscribed tumors with microcysts, epithelial cells arranged in papillary or tubular patterns, and unique staining characteristics. Most cases occur in the outer upper quadrant of the breast, with tumor sizes ranging from 10 to 55 mm. Early detection significantly improves outcomes, as this carcinoma typically exhibits mild dysplasia and low metastatic potential.
Patients should consult healthcare professionals for personalized care and long-term follow-up. This ensures timely intervention and supports overall well-being.
FAQ
What makes mammary secretory carcinoma unique compared to other breast cancers?
Mammary secretory carcinoma stands out due to its rarity, distinct histological features, and the ETV6-NTRK3 gene fusion. Unlike other triple-negative breast cancers, it exhibits indolent behavior and a low mutational burden, contributing to its generally favorable prognosis.
Can mammary secretory carcinoma occur in men?
Yes, mammary secretory carcinoma can occur in men, though it is significantly more common in women. The male-to-female ratio is approximately 1:6. Despite its rarity, early detection remains crucial for effective treatment in both genders.
Is mammary secretory carcinoma hereditary?
No evidence suggests that mammary secretory carcinoma is hereditary. Its defining genetic alteration, the ETV6-NTRK3 gene fusion, arises from a somatic mutation rather than an inherited one. Genetic counseling is not typically required for this condition.
How is mammary secretory carcinoma diagnosed?
Physicians diagnose mammary secretory carcinoma through clinical evaluation, imaging, and pathological analysis. Core needle biopsy confirms the diagnosis by identifying its unique histological features and detecting the ETV6-NTRK3 gene fusion through immunohistochemistry.
What is the long-term outlook for patients with mammary secretory carcinoma?
The long-term outlook is generally excellent. Most patients achieve high survival rates, especially with early detection and appropriate treatment. Regular follow-up care ensures early identification of recurrences or late metastases, supporting better outcomes.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Essential Insights About Carcinoid Tumors You Need
Key Features and Insights Into Cholangiocarcinoma Explained
Invasive Cribriform Carcinoma: Understanding Its Impact on Breasts
Invasive Ductal Carcinoma: Symptoms and Key Information You Need

