What Is Mediastinal Large B-Cell Lymphoma
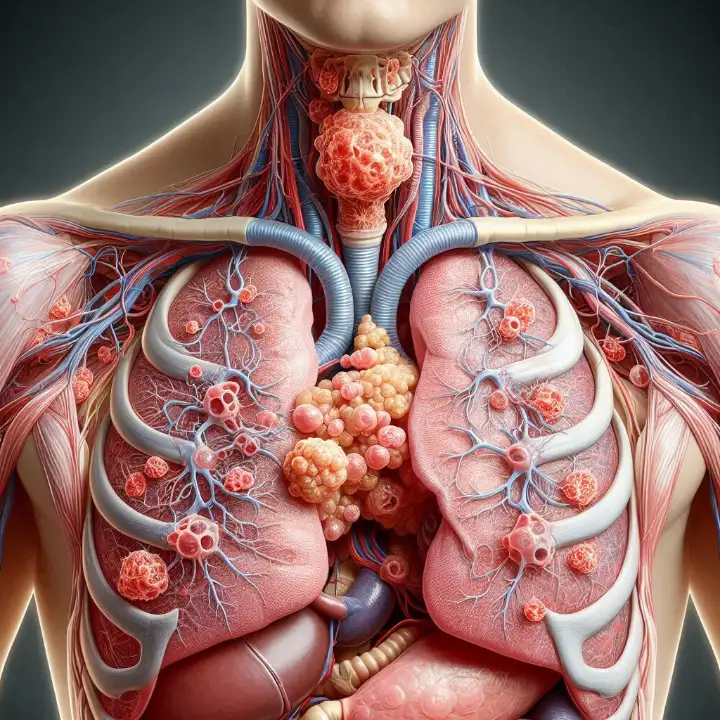
Mediastinal large B cell lymphoma is a rare and aggressive form of non-Hodgkin lymphoma that develops in the mediastinum, the area between your lungs, often originating near the thymus gland. This specific type of lymphoma accounts for only 2% to 4% of all non-Hodgkin lymphomas. It primarily affects young adults, with a median age of 35 years, and occurs more frequently in women than in men. The rapid growth associated with mediastinal large B cell lymphoma can lead to symptoms such as chest pain, shortness of breath, or swelling in the upper body, which are caused by pressure on nearby structures.
Key Takeaways
Mediastinal large B-cell lymphoma is a rare cancer. It mostly affects young adults, especially women, and starts near the thymus gland.
Symptoms include chest pain, trouble breathing, and swelling in the upper body. Finding it early helps improve treatment success.
Doctors use medical history, CT or PET scans, and biopsies to diagnose it.
Treatment often includes chemotherapy like R-CHOP and sometimes radiation. New treatments like CAR T-cell therapy are also being tested.
After treatment, regular check-ups are important to watch for the cancer coming back and to stay healthy long-term.
Characteristics of Mediastinal Large B-Cell Lymphoma
Origin and Development
Location in the Mediastinum and Thymus
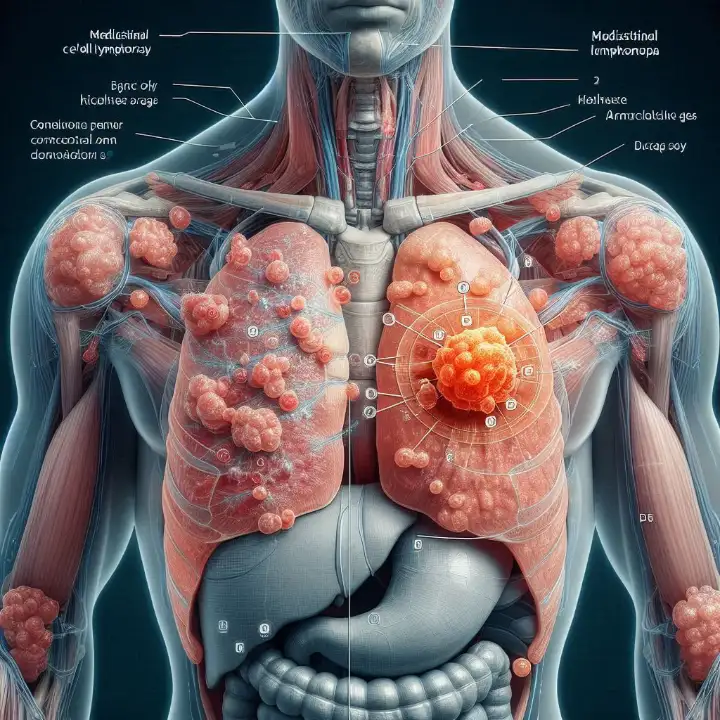
Mediastinal large B cell lymphoma originates in the mediastinum, the central area of your chest between the lungs. This region houses vital structures, including the thymus gland, where this lymphoma often begins. The tumor typically forms as a bulky mass, which can grow rapidly and compress nearby organs. Nearly all cases of this lymphoma present with a mediastinal mass, making it a hallmark feature of the disease.
Histological Features and Growth Pattern
The histological characteristics of mediastinal large B cell lymphoma distinguish it from other lymphomas. These features include fibrosis, cytomorphology, and immunophenotype. Below is a table summarizing these key features:
Feature | Description |
|---|---|
Fibrosis | Variable fibrosis, including extensive coarse and fine compartmentalizing fibrosis. |
Cytomorphology | Neoplastic cells show a range of sizes and shapes, including centroblast-like and immunoblast-like cells. |
Immunophenotype | Tumors resembling cHL show strong CD20, strong PAX-5, weak/absent CD30, and absent CD15. |
PMBL Morphology | Frequently positive for CD30 and CD15 but negative for CD20 and CD79a. |
Cell Size | Medium to large-sized cells with occasional multilobated nuclei and abundant clear cytoplasm. |
Sclerosis | Varies from delicate compartmentalizing sclerosis to broad septa of dense collagen. |
Necrosis | Focal necrosis may be present. |
Mitotic Rate | Generally high mitotic rate observed. |
The growth pattern of this lymphoma is aggressive. The tumor often exceeds 10 cm in size and can extend into nearby areas, such as the supraclavicular lymph nodes. This rapid growth can cause symptoms like chest pain, shortness of breath, and swelling. Early detection is crucial, as most patients present with stage I or II disease, which is more manageable.
Affected Population
Predominance in Young Adults and Women
Mediastinal large B cell lymphoma primarily affects young adults, with most cases occurring between the ages of 20 and 40. Women are more frequently diagnosed with this condition than men. While the exact reasons for this gender difference remain unclear, genetic factors may play a role.
Prevalence and Rarity
This lymphoma is rare, accounting for only 2-4% of all non-Hodgkin lymphomas. Despite its rarity, it is essential to recognize its unique characteristics for timely diagnosis and treatment.
Signs and Symptoms
Common Symptoms
Chest Pain and Pressure
Chest pain is one of the most common symptoms of mediastinal large B cell lymphoma. The tumor's growth in the mediastinum can press against nearby structures, causing discomfort or a feeling of tightness in your chest. This pain may worsen as the tumor enlarges, making early detection crucial.
Shortness of Breath and Difficulty Swallowing
You may experience shortness of breath if the tumor compresses your lungs or airways. This symptom often worsens as the disease progresses. Difficulty swallowing can also occur when the tumor presses against your esophagus, making it harder to eat or drink comfortably.
Swelling in the Face, Neck, or Upper Body
Swelling in the face, neck, or upper body often results from the tumor obstructing blood flow in the superior vena cava, a major vein in your chest. This condition, known as superior vena cava syndrome, can cause visible puffiness and discomfort.
Additional Symptoms
Persistent Cough or Hoarseness
A persistent, non-productive cough is another common symptom. It occurs in 40-60% of patients due to the tumor pressing on your airways. Hoarseness may also develop if the tumor affects your vocal cords or nearby nerves.
Fatigue, Fever, and Weight Loss
Fatigue is one of the most reported symptoms, affecting 50-70% of patients. It can feel overwhelming and may not improve with rest. Fever and night sweats, seen in 30-50% and 20-30% of cases respectively, often result from your immune system's response to the cancer. Unexplained weight loss, occurring in 30-40% of patients, can signal an aggressive disease.
Note: The table below summarizes the prevalence of these symptoms:
Symptom | Prevalence (%) | Description |
|---|---|---|
Fever | 30-50 | Caused by your immune system's response to cancer cells. |
Night Sweats | 20-30 | Excessive sweating during sleep due to cytokine release. |
Unexplained Weight Loss | 30-40 | Significant weight loss, often indicating aggressive disease. |
Cough | 40-60 | Non-productive cough caused by the tumor pressing on airways. |
Chest Pain | 30-50 | Pain due to tumor pressure on surrounding structures. |
Shortness of Breath | 40-60 | Difficulty breathing caused by compression of lungs or airways. |
Fatigue | 50-70 | Overwhelming tiredness that does not improve with rest. |
Lymphadenopathy | 30-50 | Swollen lymph nodes due to lymphoma progression. |
These symptoms often worsen as the disease advances. For example:
Fever and night sweats become more frequent.
Weight loss becomes more significant.
Cough and shortness of breath intensify as the tumor grows.
Recognizing these signs early can help you seek timely medical attention and improve outcomes.
Diagnosis of Mediastinal Large B-Cell Lymphoma
Initial Assessment
Medical History and Physical Examination
Diagnosing mediastinal large B cell lymphoma begins with a thorough medical history and physical examination. Your doctor will ask about symptoms like chest pain, shortness of breath, or swelling in the upper body. They may also inquire about unexplained weight loss, fatigue, or fever. During the physical exam, they will check for swollen lymph nodes or signs of superior vena cava syndrome, which can cause puffiness in the face and neck.
To support the initial assessment, doctors often order laboratory tests, including:
Complete blood cell count (CBC) to evaluate overall health.
Liver function tests to check for organ involvement.
Serum markers like LDH and beta-2 microglobulin, which can indicate disease activity.
Diagnostic Tools
Imaging Tests (e.g., CT Scans, PET Scans)
Imaging tests play a critical role in diagnosing mediastinal large B cell lymphoma. A CT scan can reveal a large, irregular mass in the mediastinum. This mass may compress nearby structures, causing symptoms like difficulty breathing or swallowing. PET scans are equally important. They detect metabolic activity by highlighting areas where lymphoma cells absorb glucose. These scans help determine the extent of the disease and guide treatment planning.
Tip: PET scans are often repeated after treatment to confirm its effectiveness. If the scan remains positive, further diagnostic steps may be necessary.
Biopsy and Histological Analysis
A biopsy is essential for confirming the diagnosis. Doctors may perform a mediastinoscopy or thoracoscopy to collect tissue samples from the mediastinal mass. Pathologists then analyze these samples under a microscope to identify the unique histological features of the lymphoma. Immunohistochemistry helps classify the tumor by detecting specific markers like CD20 and CD30.
Blood Tests and Immunohistochemistry
Blood tests provide additional insights into your condition. They help assess organ function and detect markers associated with lymphoma. Immunohistochemistry, a specialized test, identifies proteins on the surface of lymphoma cells. This step is crucial for distinguishing mediastinal large B cell lymphoma from other similar conditions, such as Hodgkin lymphoma.
Treatment Options for Mediastinal Large B-Cell Lymphoma
Standard Therapies
R-CHOP Chemotherapy Regimen
Chemotherapy is the cornerstone of treatment for mediastinal large B cell lymphoma. The R-CHOP regimen combines rituximab with four chemotherapy drugs: cyclophosphamide, doxorubicin, vincristine, and prednisone. You typically receive this treatment in 4 to 6 cycles, depending on your condition. In some cases, doctors may recommend radiation therapy after chemotherapy to target any remaining cancer cells.
Another effective option is the DA-EPOCH-R regimen. This involves dose-adjusted etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, and rituximab. Unlike R-CHOP, this approach often eliminates the need for radiation therapy. Below is a comparison of these two regimens:
Treatment Regimen | Description |
|---|---|
R-CHOP | 4 to 6 cycles of CHOP plus rituximab, often followed by radiation therapy. |
DA-EPOCH-R | 6 cycles of dose-adjusted chemotherapy, typically without radiation. |
Radiation Therapy for Localized Disease
Radiation therapy is often used when the tumor is large or does not fully respond to chemotherapy. It helps destroy any remaining cancer cells in the mediastinum. Doctors usually recommend this treatment after chemotherapy to improve outcomes and reduce the risk of recurrence.
Emerging Treatments
Immunotherapy and Targeted Therapies
Immunotherapy is a promising area of research for treating mediastinal large B cell lymphoma. CAR T-cell therapy, for example, modifies your immune cells to attack cancer. This approach has shown potential in clinical trials. Targeted therapies, such as copanlisib, work by blocking enzymes essential for tumor growth. These treatments offer hope for patients with recurrent or resistant disease.
Clinical Trials and Experimental Approaches
Clinical trials are exploring innovative combinations of therapies. For instance, researchers are studying the effects of copanlisib and nivolumab. Copanlisib inhibits tumor growth, while nivolumab prevents cancer cells from multiplying. Participating in a clinical trial could give you access to cutting-edge treatments.
Managing Side Effects
Supportive Care and Symptom Management
Managing side effects is an essential part of your treatment journey. Common side effects include fatigue, nausea, and low blood cell counts. You can work with your healthcare team to address these issues. For example, they may recommend medications to control nausea or strategies to boost your energy levels.
Here are some supportive care measures to consider:
Focus on mental health: Join a support group or speak with a therapist to manage emotional challenges.
Maintain a healthy diet: Eat nutrient-rich foods to strengthen your immune system.
Engage in light exercise: Activities like walking or yoga can help reduce fatigue and improve your mood.
By taking these steps, you can improve your quality of life during treatment.
Prognosis and Coping Strategies
Prognosis and Survival Rates
Factors Influencing Outcomes
Several factors can affect your prognosis if you have mediastinal large B cell lymphoma. Age plays a significant role, with younger patients often experiencing better outcomes. The stage of the disease at diagnosis, known as Ann Arbor staging, is another critical factor. Early-stage disease (Stage I or II) typically has a more favorable prognosis. The type of chemotherapy regimen you receive also impacts survival rates. Advances in treatment have significantly improved outcomes over the years.
Prognostic Factor | Description |
|---|---|
Age | Younger patients often have better outcomes. |
Ann Arbor Staging | Early-stage disease correlates with higher survival rates. |
Chemotherapy Treatment | Effective regimens like R-CHOP improve survival. |
Years of Diagnosis | Survival rates have improved with modern therapies. |
Long-Term Survival Statistics
Survival rates for mediastinal large B cell lymphoma have improved due to advancements in treatment. The overall 5-year survival rate is approximately 70-80%. Below is a breakdown of survival statistics over different time frames:
Survival Rate | Time Frame |
|---|---|
93.99% | 1 year |
85.04% | 5 years |
81.76% | 10 years |
These numbers highlight the importance of early diagnosis and effective treatment in improving long-term outcomes.
Coping with Diagnosis and Treatment
Emotional and Psychological Support
A cancer diagnosis can feel overwhelming, but emotional support can make a significant difference. Speaking with a therapist or joining a support group can help you manage anxiety and depression. These resources provide a safe space to share your feelings and connect with others facing similar challenges. Addressing mental health is crucial, as it can directly impact your treatment outcomes.
Accessing Support Groups and Counseling
Support groups and counseling services offer practical and emotional assistance. Many organizations provide resources tailored to patients with mediastinal large B cell lymphoma. These services can help you navigate the challenges of treatment and recovery. Consider reaching out to local or online groups for additional support.
Recurrence and Next Steps
Options for Second-Line Treatments
If your lymphoma recurs, several second-line treatments are available. These include chemotherapy regimens like ICE (ifosfamide, carboplatin, etoposide) and DHAP (dexamethasone, cisplatin, cytarabine). Targeted therapies, such as CAR T-cell therapy, have shown promise for recurrent cases. Below is a table summarizing some options:
Treatment Option | Description |
|---|---|
ICE | Combines ifosfamide, carboplatin, and etoposide. |
DHAP | Includes dexamethasone, cisplatin, and cytarabine. |
CAR T-cell | Uses modified immune cells to target cancer. |
Lenalidomide | Combined with rituximab for targeted therapy. |
Importance of Follow-Up Care
Regular follow-up care is essential after treatment. Your healthcare team will monitor your progress and check for signs of recurrence. Follow-up visits may include imaging tests and blood work to ensure the lymphoma remains in remission. Staying proactive with your care can improve your long-term outcomes and quality of life.
Mediastinal large B-cell lymphoma is a rare but aggressive cancer that requires prompt attention. You’ve learned about its symptoms, diagnostic methods, and treatment options, including chemotherapy, radiation, and emerging therapies like CAR T-cell therapy. Early diagnosis plays a vital role in improving outcomes. Acting quickly can prevent complications and increase your chances of remission and long-term survival.
Advancements in treatment have significantly improved survival rates. For example:
Radiation therapy has shown success in early-stage cases.
CAR T-cell therapy offers hope for resistant or recurrent disease.
Aspect | Details |
|---|---|
Study Focus | Long-term outcomes and optimal management of primary mediastinal large B-cell lymphoma (PMBL) |
Data Source | Swedish Lymphoma Register (SLR) covering 95% of lymphoma cases diagnosed in Sweden |
Key Findings | Emphasis on minimizing long-term toxicity while achieving cure, especially in younger patients |
Approval | Approved by the Regional Board of the Ethical Committee in Stockholm |
You are not alone in this journey. Support groups, counseling, and medical advancements provide resources to help you cope and thrive. Consulting healthcare professionals early ensures personalized care and better outcomes.
FAQ
What causes mediastinal large B-cell lymphoma?
The exact cause remains unknown. However, genetic mutations and immune system dysfunction may play a role. Researchers believe environmental factors and infections could also contribute.
How is mediastinal large B-cell lymphoma different from other lymphomas?
This lymphoma originates in the mediastinum and often affects young adults, especially women. It grows rapidly and can compress nearby organs, causing unique symptoms like chest pain and swelling in the upper body.
Can mediastinal large B-cell lymphoma be cured?
Yes, many patients achieve remission with treatments like R-CHOP chemotherapy and radiation. Early diagnosis improves the chances of a cure. Advanced therapies, such as CAR T-cell therapy, offer hope for resistant cases.
What are the side effects of treatment?
Common side effects include fatigue, nausea, and low blood counts. You may also experience hair loss or an increased risk of infections. Supportive care can help manage these effects.
Should I consider clinical trials?
Clinical trials provide access to innovative treatments, such as immunotherapy and targeted therapies. If standard treatments are ineffective, participating in a trial could offer new options. Discuss this with your doctor.
Tip: Always consult your healthcare provider to explore the best treatment options for your condition.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Exploring Diffuse Large B-Cell Lymphoma and Its Implications
A Comprehensive Guide to Intravascular Large B-Cell Lymphoma
An Overview of Anaplastic Large Cell Lymphoma Treatment Options
Decoding Large-Cell Lung Carcinoma: Types and Classifications
Insights into Large Cell Lung Carcinoma with Rhabdoid Features

