Why Ethical Dilemmas in Cancer Care Affect Patient Outcome

Cancer treatment often forces patients and families to face tough choices. These choices become ethical dilemmas because medical advice sometimes clashes with what patients value most. Many families feel uncertain and stressed. In a recent survey, 60.4% of caregivers said they faced at least one challenge when helping with decisions. They worried most about how treatment would affect the patient’s health and quality of life.
The rising number of cancer cases and deaths, especially in low- and middle-income countries, highlights how limited resources make these choices even harder.
Clear and steady advice from doctors matters. The chart below shows that people trust doctors the most, while changing recommendations can lower trust in other sources.
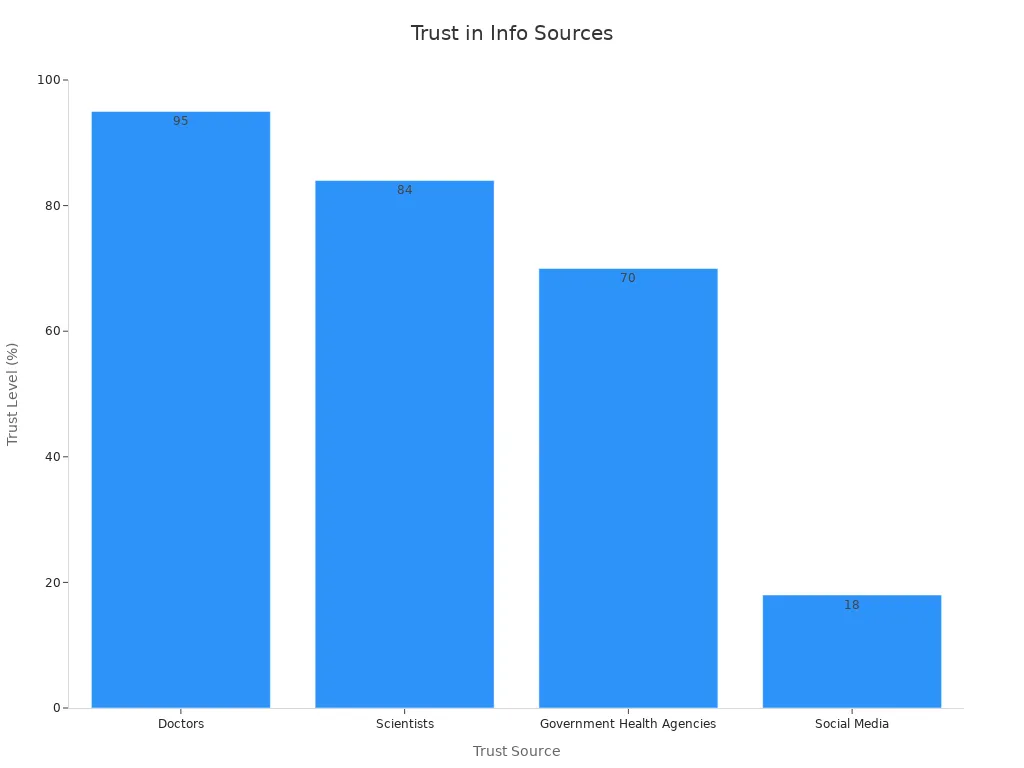
Trust Source | Trust Level (%) | Impact of Perceived Conflict on Trust |
|---|---|---|
Doctors | 95 | High trust maintained despite conflicts |
Scientists | 84 | Lower trust than doctors; affected by perceived uncertainty |
Government Health Agencies | 70 | Significantly lower trust; trust drops from 82% to 65% when recommendations perceived to change often |
Social Media | 18 | Very low trust; information validity concerns |
Understanding these challenges helps families feel more prepared. Navigating the Moral Maze: Ethical Issues in Cancer Treatment involves real-life stories that show how emotions, trust, and resources shape every decision.
Key Takeaways
Ethical dilemmas in cancer care arise when patients, families, and doctors face tough choices with no clear right answer, often due to conflicting values and limited resources.
Clear and honest communication builds trust, helps patients understand their options, and supports better decision-making throughout cancer treatment.
Patients often balance quality of life against aggressive treatments, and their preferences can change over time, highlighting the need to respect individual wishes.
Shared decision-making and early palliative care improve patient support, reduce stress, and help align treatment plans with what matters most to patients.
Addressing ethical challenges requires teamwork, open talks, and fair access to care to empower patients and families during difficult moments.
The Moral Maze in Cancer Care
Defining Ethical Dilemmas
Ethical dilemmas in cancer care happen when people face tough choices with no clear right answer. In these situations, doctors, patients, and families often struggle to decide what is best. Many people find it hard to define what makes a problem an ethical one. In a study with oncology professionals, more than half could not explain clinical ethics issues at first. However, as they talked more, they pointed to communication problems as the most common ethical challenge. Other issues included decisions at the end of life, genetic testing, resource allocation, and informed consent. For example, some patients with early-stage prostate cancer did not learn about all their treatment options. This lack of information raised concerns about patient autonomy and the right to make informed choices.
Sources of Conflict
Several factors create ethical dilemmas in cancer treatment.
Conflicting values: Patients and doctors may have different ideas about what is important. Patients want to make their own choices, but doctors feel responsible for giving the best care. Sometimes, patients choose treatments that doctors do not recommend. This clash between patient autonomy and medical advice leads to tough decisions.
Uncertainty: Cancer care often involves unknowns. Staff shortages, rising cancer cases, and heavy workloads make it hard for teams to agree on the best path.
Communication breakdowns: Problems can arise when doctors and patients do not share information clearly. Logistical challenges, such as busy team meetings, can make it harder to talk openly.
Economic pressures: Money matters in cancer care. Some patients cannot afford certain treatments. Doctors also face hard choices about expensive drugs that insurance does not cover. These financial issues can lead to unequal access and stress for everyone involved.
Real-life stories will show how these conflicts affect patients, families, and care teams. Each case highlights the complex choices people must make during cancer treatment.
Navigating the Moral Maze: Ethical Issues in Cancer Treatment
Autonomy vs. Medical Advice
One of the most common ethical dilemmas in cancer care centers on the balance between patient autonomy and medical advice. Patients want to make their own choices about treatment. Doctors want to recommend what they believe is best. Sometimes, these views do not match. For example, a patient with breast cancer may want to avoid chemotherapy because of side effects, while the doctor believes it offers the best chance for survival. This conflict can happen at any stage, from diagnosis to treatment planning.
Studies show that patients and doctors often have different preferences. The table below highlights research comparing these preferences in cancer care:
Study (First Author, Year) | Country | Cancer Type | Preference Elicitation Technique | Sample Size (Physicians / Patients) | Mode of Administration |
|---|---|---|---|---|---|
Amin, S. (2022) | US | Breast Cancer | Discrete Choice Experiment (DCE) | 117 / 169 | Online |
Fernández, O. (2022) | Spain | Renal Cell Carcinoma | DCE | 67 / 105 | Online / Paper |
Stellato, D. (2021) | Canada | Breast Cancer | DCE | 21 / 62 | Online |
Post, C. C. B. (2021) | Netherlands | Endometrial Cancer | Threshold Technique (TTM) | 63 / 171 | Online / Paper |
Le, H. (2021) | US | Lymphocytic Leukemia | DCE | 151 / 220 | Online |
Beusterien, K. (2021) | US | Breast Cancer | DCE | 200 / 300 | Online |
Maculaitis, M. C. (2021) | US | Breast Cancer | DCE & Best-Worst Scaling (BWS) | 209 / 304 | Online |
Hauber, B. (2020) | US | Non-Small Cell Lung Cancer (NSCLC) | DCE | 102 / 200 | Online |
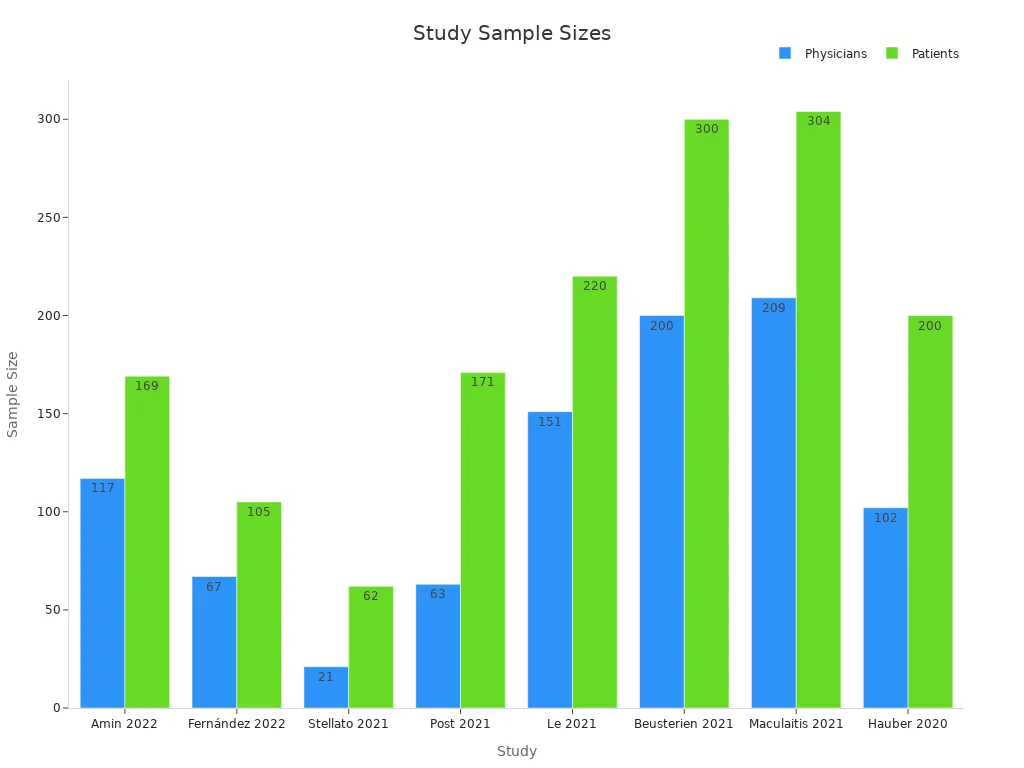
Researchers like Montgomery and Fahey, Muhlbacher and Juhnke, and Harrison have all found that doctors and patients may not always agree on what matters most in treatment. Navigating the Moral Maze: Ethical Issues in Cancer Treatment means finding ways to respect both medical expertise and patient wishes.
Quality of Life vs. Aggressive Treatment
Another challenge in Navigating the Moral Maze: Ethical Issues in Cancer Treatment is deciding between quality of life and aggressive treatment. Some patients want to live as long as possible, even if treatments cause pain or side effects. Others prefer to focus on comfort and daily activities, even if it means a shorter life.
The table below shows how patients with different cancers make these choices:
Study (Author, Year) | Country | Cancer Type & Stage | Sample Size | Patient Preferences on QoL vs LoL | Key Findings |
|---|---|---|---|---|---|
Jenkins (2013) | UK | Advanced ovarian cancer (Stages 1-4) | 225 | 33% prioritized QoL, 9% prioritized LoL, 57% valued both | Highlights diverse patient priorities balancing QoL and survival |
Collins (2013) | USA | Advanced cancer with complications (bowel obstruction, etc.) | 98 | 47% chose palliative intervention for symptom control/QoL, 20 patients for survival | Physician recommendation strongly influenced decisions |
DiBonaventura (2014) | USA | Metastatic breast cancer | 181 | Treatment effectiveness (survival) was most important | Patients weigh side effects against survival benefits |
Gerber (2012) | USA | Lung cancer | 13 | Patients expressed trade-offs between maintaining life activities and QoL | Maintenance chemotherapy decisions involve QoL considerations |
Brom (2014) | Netherlands | Glioblastoma, metastatic colorectal cancer | 28 | Some patients would stop treatment if QoL was affected; others unwilling to accept QoL over LoL | Reveals patient ambivalence in treatment decisions |
Berry (2015) | USA | Bladder cancer (Stages 0a-4) | 60 | 38% prioritized survival, balancing toxicities and LoL | Survival remains a key factor in treatment decisions |
A recent study found that many patients with advanced cancer value improvements in quality of life, such as pain control and the ability to do daily tasks, more than living longer. These preferences can change over time and depend on factors like age, income, and cancer stage. Navigating the Moral Maze: Ethical Issues in Cancer Treatment often means weighing the benefits of aggressive therapy against the risks to comfort and well-being.
Clinical trials also show that when patients of different races receive equal access to aggressive treatments, survival rates become similar. For example:
Black and White patients with advanced colorectal cancer had equal outcomes when given the same treatments.
Nurse navigator programs help minority patients complete therapy and join clinical trials, improving survival rates.
The Oncotype DX test helps guide chemotherapy decisions, but some groups still refuse treatment more often, showing ongoing disparities.
A 2022 review of cancer trials found that only 24% of new treatments improved both survival and quality of life. Many trials reported unchanged quality of life even when survival improved, showing the need to consider both factors in Navigating the Moral Maze: Ethical Issues in Cancer Treatment.
End-of-Life Choices
End-of-life decisions are among the most difficult parts of Navigating the Moral Maze: Ethical Issues in Cancer Treatment. Patients and families must choose between continuing treatment or focusing on comfort care. These choices are emotional and complex. Many patients struggle to understand what different options mean for their future.
A national survey found that 68% of patients received end-of-life care that matched their wishes. When doctors talked with patients about end-of-life care, the chance of getting care that fit their preferences more than doubled. Awareness of having a terminal illness also made it more likely that care matched patient wishes.
Aspect of Decision-Making | Numerical Evidence | Interpretation |
|---|---|---|
Patients receiving EOL care consistent with preferences | 68% | Majority receive care aligned with baseline preferences |
Increased likelihood of receiving care consistent with preferences if EOL discussion occurred | OR 2.26; P < .0001 | Physician-patient communication improves preference-concordant care |
Increased likelihood if patient aware of terminal illness | OR 3.94; P = .0005 | Awareness strongly influences care consistency |
Women with advanced breast cancer undergoing second-line chemo citing hope as reason | 43% vs. 19% (second-line vs. first-line); P = .006 | Treatment rationale varies by treatment line and hope factor |
Patient involvement in decisions to limit treatment | 50% | Patients involved only half the time in limiting treatment decisions |
Agreement between patient and oncologist preferences for comfort care | 91.4% vs. 46.7% (comfort vs. life-prolongation); P = .001 | Higher concordance when comfort care preferred |
Discordance between patient and oncologist prognostic estimates | 68% (161/236 dyads); 95% CI 62%-75% | Most patients more optimistic than oncologists |
Discordant patients unaware of discrepancy | 89% (144/161) | Lack of awareness of prognostic discordance |
Influence of awareness of cancer progression on patient decisions | 75% | Awareness is a major factor in decision-making |
Influence of knowledge that phase I drug kills cancer cells on enrollment decision | 63% | Treatment decisions influenced by perceived drug efficacy |
Despite the benefits of these talks, end-of-life discussions remain rare. In one study, only 5% of doctor visits included these conversations. Many opportunities to discuss end-of-life care were missed.
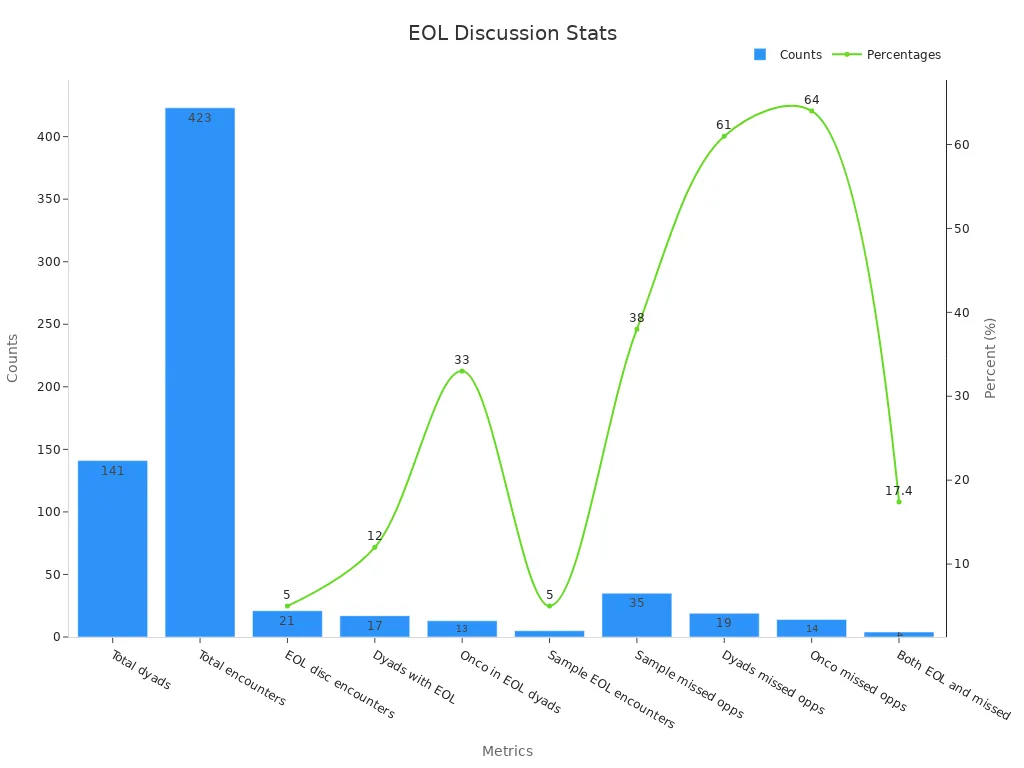
Doctors often avoid these talks because they worry about upsetting patients or feel uncomfortable. As a result, some patients continue aggressive treatments near the end of life, even when they might prefer comfort care. Navigating the Moral Maze: Ethical Issues in Cancer Treatment at this stage requires clear communication and support for patient choices.
Resource Allocation
Resource allocation is another key issue in Navigating the Moral Maze: Ethical Issues in Cancer Treatment. Cancer care needs many resources, including medicines, staff, and technology. Not all hospitals or countries have the same resources. This leads to tough choices about who gets which treatments.
Many cancer programs struggle to pay for all the services patients need. Some rely on grants, donations, or profits from drug sales to cover costs. Workforce shortages, especially in supportive roles like social workers and dietitians, limit care. New payment models try to help, but gaps remain.
Only 27% of national cancer plans now include financing strategies, up from 7% in 2018.
In high-income countries, 90% of patients have access to radiotherapy. In low-income countries, only 10% do. Twenty African countries have no radiotherapy at all.
Many plans do not mention essential medicines or evidence-based strategies.
The 4D PICTURE project uses data from Europe to predict outcomes and guide treatment. These models help doctors and patients make informed choices, but they also raise ethical questions. For example, if a model uses a patient’s postal code or income to decide who gets treatment, it could make inequalities worse. Navigating the Moral Maze: Ethical Issues in Cancer Treatment means making sure that everyone has fair access to care, no matter where they live or how much money they have.
Navigating the Moral Maze: Ethical Issues in Cancer Treatment involves many difficult choices. Each stage, from diagnosis to end-of-life, brings new challenges. Patients, families, and doctors must work together to find the best path forward.
Impact on Patient Care

Decision-Making Challenges
Ethical dilemmas in cancer care often make decision-making hard for patients and families. Many patients face cancer for the first time and do not know what to expect. They need help to understand their choices. Sometimes, doctors give too much or too little information, which can confuse patients. Patients may also get conflicting advice from different sources. Limited time with doctors can make it harder for patients to ask questions or share their concerns.
Patients often struggle to match the information they need with what they receive.
Some patients cannot remember which decisions they made or why.
Fear of making the wrong choice can cause stress and regret.
Patients feel less burdened when they have enough time, talk with experts or family, and get clear advice from doctors.
Purpose/Focus | Impact on Patient Care Processes | |
|---|---|---|
Patient Experience (PE) | Measures quality of communication, patient involvement, and satisfaction | Identifies barriers in decision-making and care flow affecting patient engagement |
Cost Outcomes (CO) | Evaluates financial impact and resource utilization | Assesses efficiency of care processes influenced by decision-making challenges |
Return on Investment (ROI) | Quantifies value of navigation programs and interventions | Supports justification for resources addressing decision-making barriers |
Communication and Trust
Good communication builds trust between patients and care teams. When doctors listen and show empathy, patients feel safer and more respected. Open talks help patients share their feelings and make better choices. However, not all doctors use these skills. Some ignore strong emotions or do not explain things clearly. This can break trust and make patients feel alone.
A study found that only 38% of patients with advanced cancer remembered talking about end-of-life wishes with their doctor. When these talks do not happen, patients may get treatments they do not want. Patient-centered communication increases trust and helps patients take part in decisions. If doctors do not match their style to what patients want, trust can suffer.
Emotional and Psychological Effects
Ethical dilemmas in cancer care can cause strong emotions. Patients may feel shock, anxiety, or fear about their future. Some worry about making the wrong choice or regret past decisions. Healthcare workers who become patients often feel embarrassed or hopeless. Younger patients may worry about work, money, or unfinished goals.
A national study showed that patients with high stress felt less satisfied with their care. They also had trouble understanding treatment plans and felt doctors did not spend enough time with them. Emotional distress can start before diagnosis and get worse if patients get mixed messages from their care team. These feelings affect not only patients but also families and healthcare providers. Support and clear communication can help ease this burden.
Strategies for Resolution
Shared Decision-Making
Shared decision-making (SDM) helps patients, families, and providers work together to make choices that fit patient values and medical facts. SDM uses tools like decision aids and patient-reported data to improve understanding and reduce confusion. Research shows that when oncologists use patient-reported data, they see higher engagement in SDM. Decision aids also lower anxiety and help patients feel more confident about their choices.
Study (Author, Year) | Cancer Type | Intervention/Tool | Key Findings |
|---|---|---|---|
Berry et al. (RCT) | Prostate | P3P Decision Aid | Reduced decisional conflict, especially for older, anxious, or less supported patients |
Frey et al. | Ovarian | Priorities Tool | Over half felt more comfortable with SDM; most found it helpful for future decisions |
Giannitrapani et al. | Various | Informed Consent | Helped clarify risks and benefits, making SDM easier |
Colley et al. | Multiple | Control Preferences Scale | Showed the need for tailored SDM based on patient background |
A five-step SDM process guides clinicians to identify key decisions, explain options, ask about patient preferences, and agree on next steps. Oncology nurses play a key role by teaching, supporting, and advocating for patients.
Early Palliative Care
Early palliative care supports patients from the start of cancer treatment. It focuses on comfort, symptom control, and emotional support. Randomized trials show that early palliative care improves quality of life, reduces depression, and helps patients make better treatment choices. Patients who receive early palliative care often spend less time in the hospital and more time at home.
Early palliative care helps patients and families talk about goals, plan for the future, and manage symptoms. This approach respects patient wishes and reduces stress during difficult times.
Clinical guidelines now recommend starting palliative care early for advanced cancer. This helps address ethical dilemmas by supporting patient-centered decisions and improving satisfaction.
Clear Communication
Clear communication builds trust and helps everyone understand the choices ahead. Good communication ensures patients know their options and can match decisions to their values. Nurses and doctors who use structured communication models, like the COMFORT framework, feel more confident in tough conversations.
Decision aids and tailored talks help patients with different backgrounds understand risks and benefits.
Ongoing training for care teams improves communication skills and reduces ethical conflicts.
Strong communication supports ethical care by making sure every voice is heard and respected.
Ethical dilemmas in cancer treatment often arise from conflicting values, uncertainty, and limited resources. These challenges can affect patient care and decision-making. Effective strategies, such as shared decision-making and early palliative care, help patients and families feel supported. Clinical trials using ethical frameworks have led to positive outcomes, as shown below:
Metric | Value/Description |
|---|---|
Trials analyzed | |
Success rate of new treatments | 25%–50% |
Breakthrough interventions discovered | 15% |
Open communication and teamwork empower patients and families to face tough choices with confidence.
FAQ
What is an ethical dilemma in cancer treatment?
An ethical dilemma happens when doctors, patients, or families face a tough choice with no clear right answer. These situations often involve conflicts between medical advice and personal values.
Why do patients and doctors sometimes disagree about treatment?
Patients may value comfort or quality of life, while doctors focus on survival or medical guidelines. Different backgrounds, beliefs, and goals can lead to disagreements about the best path forward.
How can families support loved ones facing tough decisions?
Families can listen, ask questions, and encourage open talks with the care team. Support helps patients feel less alone and more confident in their choices.
What role does communication play in solving ethical dilemmas?
Clear, honest communication builds trust and helps everyone understand the options. Good conversations make it easier to match treatment plans with patient wishes.
Are there resources to help with ethical decisions in cancer care?
Yes. Many hospitals offer ethics committees, social workers, or patient navigators. These resources guide families and patients through difficult choices and provide extra support.
See Also
Recognizing Signs And Treatment Options For Duodenal Cancer
Identifying Causes And Symptoms Of Esophageal Cancer
An Overview Of Endometrial Cancer And Its Symptoms

