Exploring Treatment Options for Non Small Cell Lung Cancer
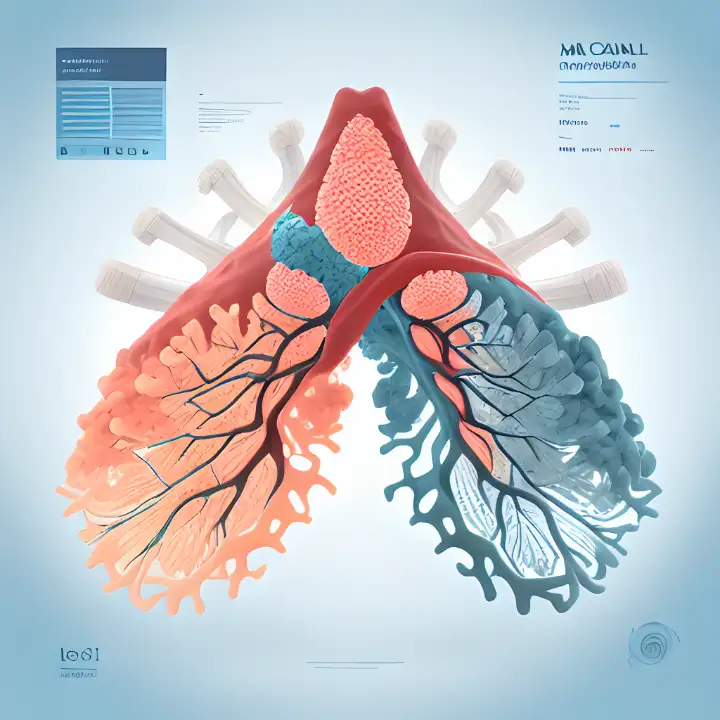
When you're facing non small cell lung cancer, understanding your treatment options can feel overwhelming. From chemotherapy and radiation to targeted therapies and immunotherapy, there are several approaches available. Each treatment works differently, and doctors often combine them to improve outcomes. For example, surgery might be an option for early-stage cancer, while advanced stages may rely on systemic therapies like immunotherapy or chemoradiation.
Treatments are tailored to your unique needs, considering factors like your overall health, cancer stage, and genetic markers. While these therapies can extend life or even cure the disease in some cases, they may also bring side effects. Common ones include fatigue, nausea, and hair loss, while rarer effects might involve nerve damage or changes in heart function. Knowing what to expect can help you feel more prepared and in control.
Key Takeaways
Learn about main treatments for non-small cell lung cancer: surgery, chemo, radiation, targeted therapy, and immunotherapy.
Treatment plans are made just for you. They look at your health, cancer stage, and genes to help you get better results.
Talk to your doctor about side effects. Knowing them early can help you handle problems during treatment.
Check out clinical trials for new treatments. These might give you more choices to improve your care.
Palliative care helps at any time. It works to make life better by easing symptoms and emotional stress.
Overview of Treatment Options
Surgery
Types of Surgical Procedures
Surgery is often the first step in treating non small cell lung cancer, especially in its early stages. Depending on your condition, doctors may recommend one of the following procedures:
Lobectomy: This involves removing an entire lobe of the lung and is the most common surgery for stage I and II cancers.
Wedge Resection: If your lung function is limited, this procedure removes only a small portion of the lung.
Pneumonectomy: In cases where the tumor is located centrally, the entire lung may need to be removed.
Surgical Procedure | Description | Effectiveness |
|---|---|---|
Lobectomy | Removal of a lobe of the lung | |
Wedge Resection | Removal of a small part of the lung | Suitable for patients with impaired lung function |
Pneumonectomy | Removal of an entire lung | Used when necessary based on tumor location |
Indications for Surgery
Surgery is typically an option if the tumor is localized and can be completely removed. Doctors consider several factors, including:
The stage of cancer: Surgery is most effective for stages I, II, and some IIIA cases.
Resectability: Imaging and biopsies help determine if the tumor can be safely removed.
Your overall health: You need to be strong enough to handle the procedure and recovery.
If surgery is viable, it may be followed by chemotherapy to eliminate any remaining cancer cells.
Chemotherapy
Mechanism of Action
Chemotherapy works by targeting rapidly dividing cancer cells. Drugs like cisplatin and carboplatin disrupt DNA repair, causing cancer cells to die. Others, such as paclitaxel, interfere with cell division, halting tumor growth.
Common Chemotherapy Drugs
Doctors often use a combination of drugs to treat non small cell lung cancer. Some commonly prescribed options include:
Cisplatin and carboplatin
Paclitaxel (Taxol) and docetaxel (Taxotere)
Gemcitabine (Gemzar) and pemetrexed (Alimta)
While chemotherapy can be effective, it may cause side effects like fatigue, nausea, and hair loss. Discussing these with your doctor can help you prepare.
Radiation Therapy
Types of Radiation Therapy
Radiation therapy uses high-energy rays to destroy cancer cells. Depending on your needs, your doctor might suggest:
External Beam Radiation Therapy: Delivered from outside the body, this is the most common type.
Brachytherapy: Radioactive material is placed directly near the tumor using a bronchoscope.
Stereotactic Body Radiation Therapy (SBRT): High doses of radiation are delivered in fewer sessions, targeting the tumor precisely.
Description | |
|---|---|
External Beam Radiation Therapy | Focuses radiation from outside the body, typically over several weeks. |
Brachytherapy | Places radioactive material directly in the airways to shrink tumors. |
Proton Therapy | Uses protons for precise targeting, minimizing damage to surrounding tissue. |
Indications for Radiation
Radiation therapy is often used when surgery isn’t an option or to target any remaining cancer cells after surgery. It’s also effective for shrinking tumors before surgery or relieving symptoms in advanced stages. Factors like tumor size, location, and your overall health play a role in deciding if radiation is right for you.
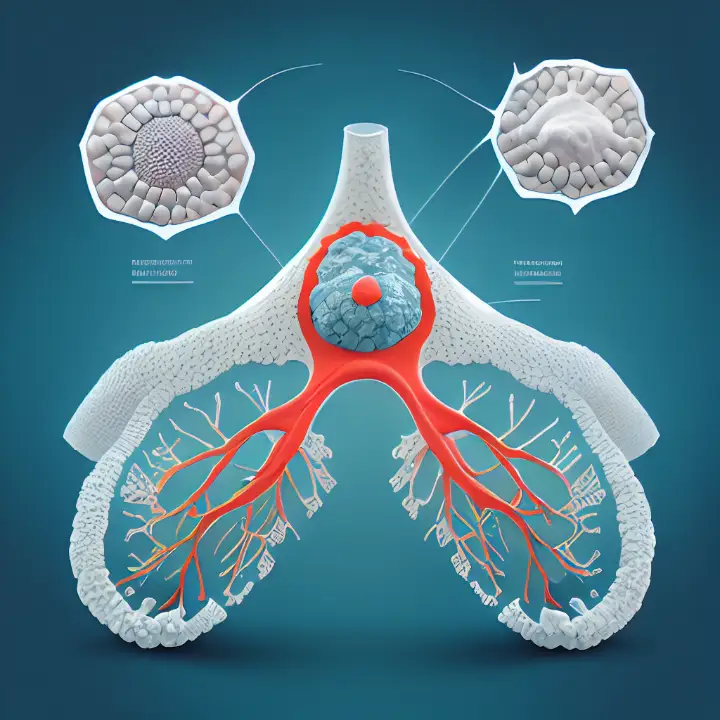
Targeted Therapy
Mechanism of Targeted Therapy
Targeted therapy focuses on specific molecules or pathways that help cancer cells grow and spread. Unlike chemotherapy, which attacks all rapidly dividing cells, targeted drugs aim at precise abnormalities in cancer cells. This approach minimizes damage to healthy cells and often results in fewer side effects.
Here’s a breakdown of how these therapies work:
Therapy Type | Mechanism of Action |
|---|---|
Angiogenesis Inhibitors | Block the formation of new blood vessels by targeting VEGF, cutting off the tumor's blood supply. |
KRAS Inhibitors | Target abnormal KRAS proteins to stop cancer cell growth and spread. |
EGFR Inhibitors | Block signals from mutated EGFR genes that drive uncontrolled cell growth. |
MET Inhibitors | Attack abnormal MET proteins caused by gene mutations to slow tumor progression. |
HER2-directed Drugs | Target HER2 gene changes that promote cancer cell growth in some cases of non small cell lung cancer. |
TRK Inhibitors | Disable abnormal TRK proteins caused by NTRK gene fusions, halting cancer growth. |
BRAF Inhibitors | Target altered BRAF proteins to inhibit cancer cell growth. |
RET Inhibitors | Block abnormal RET proteins caused by gene rearrangements to slow tumor growth. |
Examples of Targeted Drugs
Several targeted drugs are available for treating non small cell lung cancer. These drugs are often chosen based on the genetic mutations present in your tumor.
Drug Name | Type | Mechanism | Median Progression-Free Survival (mPFS) |
|---|---|---|---|
Sotorasib (Lumakras) | KRAS inhibitor | Targets KRAS G12C mutation | N/A |
Afatinib (Gilotrif) | EGFR inhibitor | Targets exon 19 or 21 mutations | ~48 months |
Osimertinib (Tagresso) | EGFR inhibitor | Targets exon 19 or 21 mutations | ~18 months |
Capmatinib (Tabrecta) | MET inhibitor | Targets MET exon 14 skipping mutation | N/A |
Larotrectinib (Vitrakyi) | TRK inhibitor | Targets NTRK gene fusion mutation | N/A |
These therapies can significantly improve outcomes, especially when matched to the right genetic profile.
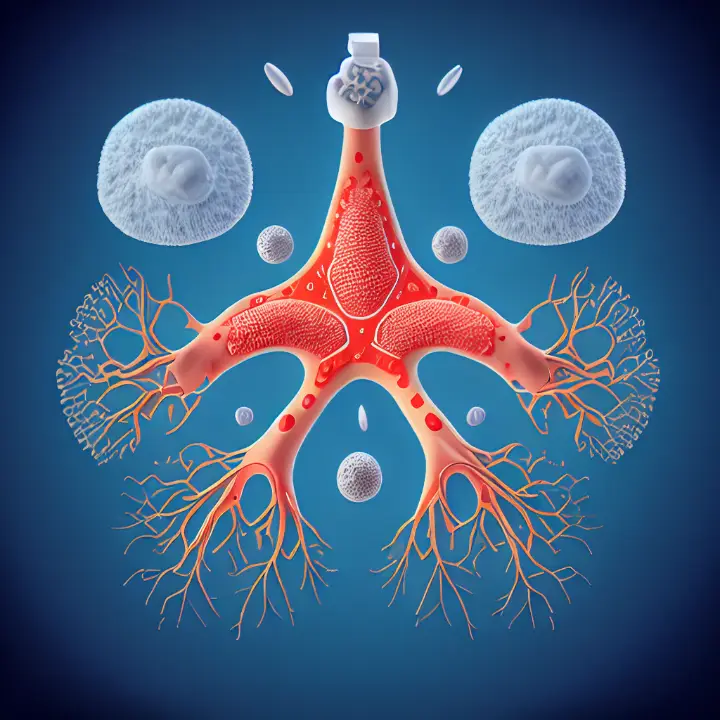
Immunotherapy
Mechanism of Immunotherapy
Immunotherapy helps your immune system recognize and attack cancer cells. It uses antibodies to block proteins like CTLA-4, PD-1, and PD-L1, which tumors exploit to evade immune responses. By targeting these proteins, immunotherapy reactivates your immune system to fight cancer.
For example:
Anti-CTLA-4 drugs like ipilimumab improve survival by enhancing T-cell activity.
PD-1 inhibitors such as nivolumab and pembrolizumab block the PD-1 protein, allowing immune cells to attack tumors more effectively.
Patients with high PD-L1 expression often see better outcomes, with some achieving a median survival of 15.5 months using pembrolizumab.
Common Immunotherapy Drugs
Here are some commonly used immunotherapy drugs and their potential side effects:
Drug Type | Common Drugs | Side Effects |
|---|---|---|
PD-1 Immune Checkpoint Inhibitors | nivolumab, pembrolizumab, atezolizumab, durvalumab | Fatigue, skin rash, flu-like symptoms, organ inflammation, and joint pain. |
CTLA-4 Immune Checkpoint Inhibitors | ipilimumab, tremelimumab | Similar to PD-1 inhibitors, with potential severe immune-related reactions. |
While immunotherapy offers hope, it’s essential to discuss potential side effects with your doctor.
Symptom Management
Palliative Care Options
Palliative care focuses on improving your quality of life by managing symptoms and side effects. It’s not just for advanced stages; you can benefit from it at any point during your treatment.
Palliative care helps relieve symptoms like pain, fatigue, and shortness of breath. It can also address emotional and psychological challenges.
This type of care often includes medications, counseling, and therapies like radiation or chemotherapy to ease discomfort.
Managing Treatment Side Effects
Dealing with side effects can be challenging, but there are ways to make it easier:
Fatigue: Rest often, eat well, and engage in light activities.
Shortness of Breath: Practice relaxation exercises and follow your doctor’s advice.
Skin Reactions: Use gentle skincare products and avoid sun exposure.
Throat and Mouth Soreness: Stick to soft foods and rinse with saltwater.
By staying proactive and communicating with your healthcare team, you can manage these challenges effectively.
Factors Influencing Treatment Decisions
Cancer Type and Stage
Differences in Cancer Types
The type of non small cell lung cancer you have can significantly influence your treatment plan. For example, adenocarcinoma, the most common type, often responds well to targeted therapies if specific mutations are present. On the other hand, squamous cell carcinoma may require a different approach, such as chemotherapy or immunotherapy. Understanding the type of cancer helps your doctor choose the most effective treatment for you.
Impact of Staging on Treatment
The stage of your cancer plays a huge role in determining your treatment options. Early-stage cancers, like stage II, might involve surgery followed by chemotherapy to ensure all cancer cells are eliminated. For stage IIIA, a combination of chemotherapy, radiation, and sometimes surgery is common. Advanced stages, such as IVA or IVB, focus on systemic therapies like targeted drugs or immunotherapy to manage symptoms and improve quality of life.
Patient Health and Preferences
Role of Overall Health
Your overall health is a key factor in deciding your treatment. If you're in good health, you might tolerate aggressive treatments like surgery or combined therapies. However, if you have other health conditions, your doctor may recommend less intensive options to minimize risks.
Importance of Patient Goals
Your personal goals and preferences matter too. Some patients prioritize longer progression-free survival, while others focus on minimizing side effects like fatigue or nausea. Treatment costs can also influence your decisions. Discussing these factors with your doctor ensures your treatment aligns with what matters most to you.
Genetic and Molecular Testing
Identifying Genetic Mutations
Genetic testing has become a standard part of diagnosing and staging non small cell lung cancer. It identifies mutations like EGFR, ALK, or KRAS, which can guide your treatment. For instance, if your tumor has an EGFR mutation, targeted drugs like osimertinib may be highly effective.
Guiding Targeted Therapy
Molecular testing methods like PCR, FISH, and NGS help pinpoint specific mutations. Here's a quick overview:
Testing Method | Application | Approved by FDA |
|---|---|---|
PCR | Identifies EGFR mutations | Yes |
FISH | Tests ALK rearrangements | Yes |
IHC | Tests mutations of PD-L1, ROS1, EGFR, BRAF-V600E, RET, and ALK | Yes |
NGS | Identifies multiple mutations including EGFR, RET, MET, ALK, HER2, BRAF, ROS1, KRAS, NTRK, and new biomarkers like PIK3CA | N/A |
These tests not only guide targeted therapy but may also qualify you for clinical trials, offering access to innovative treatments.
Treatment by Cancer Stage
Early-Stage (Stages 1 and 2)
Primary Role of Surgery
If you’re diagnosed with early-stage non small cell lung cancer, surgery is often the first and most effective treatment option. Here’s how it works:
Doctors assess whether the tumor is resectable using imaging studies and biopsies.
If the tumor can be removed, surgery is performed to eliminate it completely.
Common procedures include lobectomy, wedge resection, or segmentectomy, depending on the tumor’s size and location.
Surgery offers the best chance for a cure in stages I and II. However, your overall health and lung function play a big role in determining if surgery is right for you.
Adjuvant Therapies
After surgery, adjuvant therapies help reduce the risk of cancer coming back. These treatments target any remaining cancer cells that surgery might have missed. Options include:
Chemotherapy: Often used for stage IIA and IIB to improve survival rates.
Targeted Therapy: Effective for patients with specific genetic mutations like EGFR or ALK.
Immunotherapy: Studies like IMpower-010 show it can lower the chances of metastasis.
Radiation Therapy: Sometimes used if the surgical margins aren’t clear.
Combining these therapies with surgery has shown promising results, especially when tailored to your genetic profile.
Locally Advanced (Stage 3)
Combining Treatments
For stage III non small cell lung cancer, combining treatments is key. Doctors often recommend chemoradiotherapy followed by immunotherapy to improve outcomes. Here’s a quick look at some effective combinations:
Treatment Combination | Phase | PFS | OS |
|---|---|---|---|
Chemoradiotherapy + Durvalumab | III | 3 years | 4 years |
Pembrolizumab + Radiotherapy | III | Significant improvement | N/A |
Nivolumab + Ipilimumab + Chemotherapy | N/A | N/A | Extended OS |
These combinations work by shrinking the tumor, boosting your immune system, and preventing recurrence.
Surgical Options
Surgery may still be an option for some stage IIIA cases if the tumor is resectable. Techniques like lobectomy or segmentectomy are common, and minimally invasive methods like video-assisted thoracoscopic surgery (VATS) are often used. However, surgery is usually combined with induction therapy, such as chemotherapy or radiation, to improve success rates.
Advanced or Metastatic (Stage 4)
Focus on Systemic Therapies
When cancer has spread to other parts of your body, systemic therapies become the focus. These treatments work throughout your body to control the disease and improve your quality of life. Common options include:
Targeted Drug Therapy: Ideal for cancers with mutations like EGFR or KRAS.
Immunotherapy: Drugs like pembrolizumab and nivolumab help your immune system fight cancer.
Chemotherapy: Often combined with other therapies to enhance effectiveness.
Angiogenesis Inhibitors: Medications like bevacizumab cut off the tumor’s blood supply.
Your doctor will choose the best combination based on your cancer’s genetic profile and your overall health.
Palliative Care
Palliative care plays a vital role in advanced stages. It focuses on relieving symptoms like pain, fatigue, and shortness of breath. This type of care also helps you cope emotionally and make informed decisions about your treatment.
Remember, palliative care isn’t just for end-of-life situations. It’s about improving your quality of life at any stage of your journey.
By combining systemic therapies with palliative care, you can manage symptoms effectively and maintain a better quality of life.
Emerging Therapies and Clinical Trials
Innovative Treatments
Advances in Precision Medicine
Precision medicine is transforming how non-small cell lung cancer (NSCLC) is treated. It focuses on tailoring therapies to your tumor’s unique genetic makeup. For example, targeted drugs like sotorasib and adagrasib are now available for KRAS mutations, which were once considered untreatable. These advancements mean you could receive treatments designed specifically for your cancer type, improving outcomes and reducing side effects.
Researchers are also exploring new ways to combine therapies. For instance, adding immunotherapy to chemoradiotherapy has shown significant improvements in survival rates for stage III NSCLC. This approach enhances your immune system’s ability to fight cancer while addressing the tumor directly.
New Immunotherapy Combinations
Immunotherapy combinations are another exciting area of innovation. Drugs like durvalumab, pembrolizumab, and atezolizumab are being paired with other treatments to boost their effectiveness. Here’s a quick look at some promising combinations:
Treatment | Mechanism | Outcome |
|---|---|---|
Durvalumab + Chemoradiotherapy | Immune checkpoint inhibitor | OS up to 4 years, PFS up to 3 years in stage III NSCLC |
Pembrolizumab | Immune checkpoint inhibitor | mPFS for 10.3 months, median OS for 15.5 months in high PD-L1 expression patients |
Sugemalimab | Anti-PD-L1 monoclonal antibody | Better PFS compared to Durvalumab in stage IV NSCLC |
These combinations could offer you more effective options, especially if your cancer has specific biomarkers.
Clinical Trials
Finding and Enrolling in Trials
Clinical trials give you access to cutting-edge treatments. You can find trials through resources like:
LUNGevity’s Clinical Trial Finder, which matches you to trials based on your cancer type and location.
EmergingMed, offering navigators to guide you through the enrollment process.
ClinicalTrials.gov, where you can search for trials by eligibility and location.
My Cancer Genome, which links genetic mutations to relevant trials.
Lung-MAP, a program that matches advanced NSCLC patients to drug trials.
These tools make it easier for you to explore new treatment possibilities.
Benefits and Risks
Participating in a trial can give you early access to innovative therapies. However, it’s important to weigh the risks, like potential side effects or the chance that the treatment may not work. Discussing these with your doctor can help you make an informed decision.
Future Directions
Promising Research Areas
Research is advancing rapidly in NSCLC treatment. Scientists are focusing on targeting genetic mutations like KRAS and ALK, which could open doors to more effective therapies. Combining immunotherapy with traditional treatments, such as chemoradiotherapy, has also shown promise in improving survival rates.
The National Cancer Institute continues to fund trials for new therapies, highlighting the commitment to finding better solutions for you.
Potential Breakthroughs
The future looks bright with potential breakthroughs on the horizon. Immunotherapy is evolving to enhance your immune system’s ability to fight cancer. For example, higher levels of immune cells like CD4+ T cells and natural killer cells are linked to better outcomes.
Here’s a snapshot of what’s coming:
Sotorasib and adagrasib for KRAS mutations.
Crizotinib for ALK-positive NSCLC, offering a PFS of 10.9 months.
New combinations like chemoradiotherapy with durvalumab, extending OS up to 4 years.
These advancements could revolutionize how NSCLC is treated, giving you more hope for the future.
When it comes to treating non small cell lung cancer, you have a variety of options. From surgery and chemotherapy to targeted therapies and immunotherapy, each approach offers unique benefits. The key is finding the right combination that fits your specific needs. Personalized treatment plans take into account your health, cancer stage, and genetic profile, giving you the best chance for success.
Don’t hesitate to talk to your doctor about your options. Clinical trials might also open doors to cutting-edge therapies that could make a difference in your journey.
FAQ
What is the most common treatment for non-small cell lung cancer?
The most common treatment depends on the stage of your cancer. Early stages often involve surgery, while advanced stages may require chemotherapy, targeted therapy, or immunotherapy. Your doctor will recommend the best option based on your specific case.
Can I combine different treatments?
Yes, combining treatments is common. For example, doctors may pair chemotherapy with radiation or add immunotherapy to improve results. Your treatment plan will depend on your cancer type, stage, and overall health.
Are there side effects from these treatments?
Yes, treatments like chemotherapy and radiation can cause side effects such as fatigue, nausea, or hair loss. Targeted therapies and immunotherapy may have fewer side effects but can still cause issues like skin rash or inflammation. Always discuss potential side effects with your doctor.
How do I know if I qualify for clinical trials?
You may qualify if your cancer has specific genetic mutations or if standard treatments haven’t worked. Tools like ClinicalTrials.gov or your doctor can help you find trials that match your condition.
Is palliative care only for end-of-life situations?
No, palliative care isn’t just for end-of-life. It helps manage symptoms and improve your quality of life at any stage of treatment. You can benefit from it alongside other therapies.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Exploring Symptoms and Therapies for Large Granular Lymphocyte Leukemia
Anaplastic Large Cell Lymphoma: Definition and Treatment Options
A Guide to Large-Cell Lung Carcinoma and Its Types
Recognizing Symptoms and Treatment Approaches for Duodenal Cancer

