Exploring the Current Role of Artificial Intelligence in Oncology Research

Artificial intelligence (AI) refers to computer systems that mimic human intelligence to solve complex problems. The role of artificial intelligence in oncology research is vital, as it significantly improves the detection, diagnosis, and treatment of cancer. You can see its impact in tools like Computer-Aided Detection (CADe), which help identify cancerous lesions faster and with greater accuracy. By optimizing resource allocation and expanding access to care in underserved communities, AI addresses critical challenges in cancer care. With advancements in computational tools and scalable algorithms, the role of artificial intelligence in oncology research is reshaping the field. How will AI continue to transform oncology research in the years ahead?
Key Takeaways
AI helps find cancer by studying medical images. It works faster and more accurately, leading to earlier detection and better chances of survival.
AI creates personalized treatment plans. It uses genetic data and patient details to choose the best therapies with fewer side effects.
AI speeds up drug discovery. It tests compounds quickly and predicts how well they work, saving time and money on new medicines.
AI uses predictive tools to track patient health. This helps doctors act early and use healthcare resources wisely.
AI and doctors work together to improve cancer care. Technology adds speed, while doctors bring care and good decision-making.
The Role of Artificial Intelligence in Oncology Research
Defining AI in the Context of Healthcare
Artificial intelligence in healthcare refers to machines designed to perform tasks that typically require human intelligence. These tasks include analyzing medical images, predicting patient outcomes, and even assisting in treatment decisions. AI encompasses several technologies, such as machine learning (ML), which enables computers to learn from data, and deep learning (DL), which uses neural networks to process complex datasets like medical imaging. For example, DL has revolutionized cancer diagnostics by improving the accuracy of tumor detection in radiology and pathology.
AI also includes large language models (LLMs), which generate new content based on user prompts. In oncology, these models can analyze clinical notes or research papers to identify patterns and insights. By simulating human cognitive abilities, AI has become a cornerstone of modern healthcare innovation.
Why Oncology is a Key Focus for AI Applications
Cancer remains one of the leading causes of death worldwide, making oncology a critical area for AI applications. AI's ability to process vast amounts of data quickly and accurately addresses the complexity of cancer care. For instance, AI tools improve diagnostic accuracy by identifying cancerous cells in medical images with precision. They also assist in personalized treatment planning by analyzing molecular profiles to recommend targeted therapies.
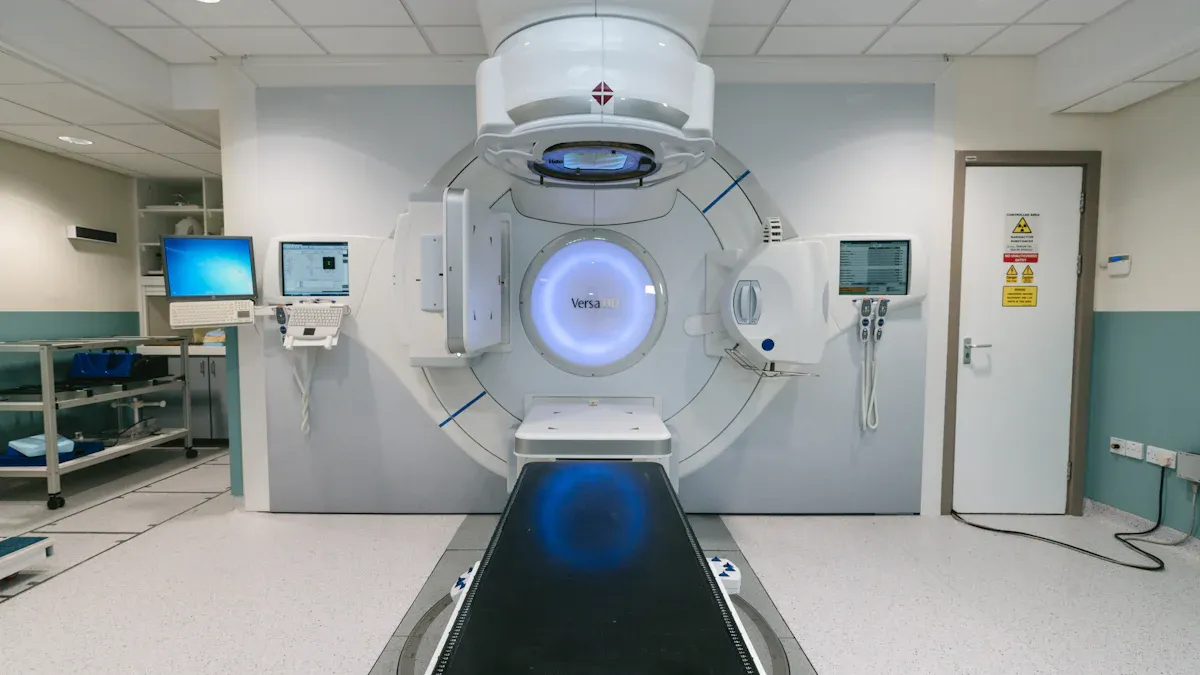
Statistics highlight oncology's prominence in AI research. A significant percentage of AI devices focus on cancer radiology (54.9%), pathology (19.7%), and radiation oncology (8.5%). These numbers reflect the growing reliance on AI to enhance cancer care across specialties.
Technologies Powering AI in Oncology
Several advanced technologies drive the role of artificial intelligence in oncology research. Machine learning plays a pivotal role in analyzing DNA data to identify genetic mutations linked to cancer. Deep learning excels in image classification, enabling faster and more accurate cancer detection in radiology and pathology. High-throughput sequencing and multi-omic data integration further enhance AI's capabilities, paving the way for comprehensive cancer profiling.
AI also accelerates drug discovery by analyzing datasets to identify potential therapeutic targets. For example, it can link drug profiles to cancer pathways, maximizing the utility of existing pharmaceuticals. These technologies not only improve efficiency but also open new avenues for personalized medicine, ensuring better outcomes for patients.
Current Applications of AI in Oncology
AI in Early Cancer Detection and Diagnostics
Artificial intelligence has revolutionized early cancer detection by improving diagnostic accuracy and speed. AI algorithms analyze medical images, such as mammograms and colonoscopy scans, to identify abnormalities that might be missed by the human eye. For instance, FDA-approved AI tools have enhanced breast cancer detection by interpreting mammograms with greater precision. Similarly, machine learning models used in colonoscopy improve the identification of polyps and precancerous lesions, which can significantly reduce the risk of colorectal cancer.
AI platforms also predict the effectiveness of cancer immunotherapy by identifying early disease signatures. These advancements enable clinicians to detect cancer at its earliest stages, improving patient outcomes and survival rates.
AI in Personalized Treatment Planning
AI plays a critical role in tailoring cancer treatments to individual patients. By analyzing genomic data, radiomics, and patient demographics, AI identifies disease markers and predicts responses to therapies like chemotherapy. This precision ensures that patients receive the most effective treatments while minimizing side effects. For example, deep learning models can forecast how a patient will respond to specific drugs, helping oncologists make informed decisions.
AI also supports collaborative research through federated learning frameworks. These frameworks allow researchers to share insights without compromising patient privacy, fostering innovation in personalized medicine. As a result, AI-driven treatment planning improves outcomes and reduces complications for cancer patients.
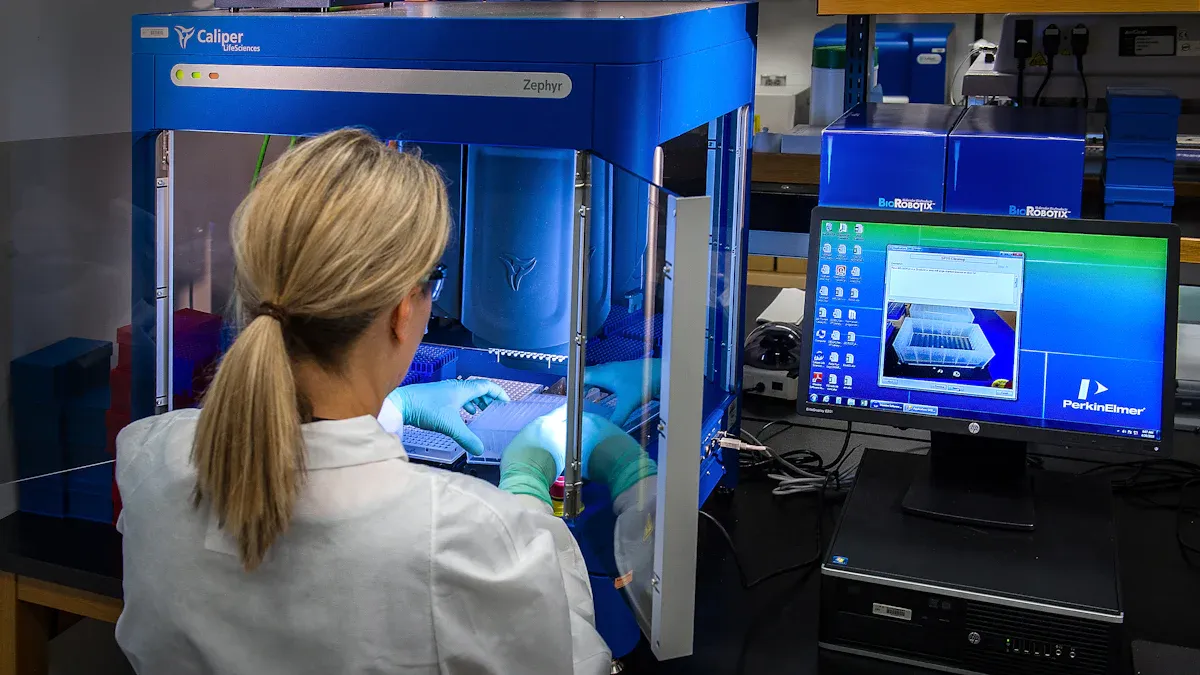
AI in Drug Discovery and Development
The drug development process in oncology is notoriously slow and expensive, with fewer than 4% of anti-cancer drug candidates gaining FDA approval. AI addresses this challenge by rapidly screening thousands of compounds to identify those with the highest potential for success. This approach reduces costs and accelerates the timeline for bringing new treatments to market.
AI also links drug profiles to cancer pathways, enabling researchers to repurpose existing drugs for new applications. By streamlining drug discovery, AI contributes to more efficient and effective cancer therapies, ultimately benefiting patients worldwide.
AI in Predictive Analytics and Patient Monitoring
Artificial intelligence (AI) is transforming how you monitor and manage patient health. Predictive analytics, powered by AI, allows healthcare providers to anticipate potential health issues before they become critical. This proactive approach improves patient outcomes and reduces the strain on healthcare systems.
AI-powered devices, such as wearable technologies, continuously track vital signs like heart rate and oxygen levels. These devices detect irregularities in real time, enabling early medical intervention. For example, a wearable device can identify abnormal heart rhythms and alert you or your healthcare provider immediately. This reduces the need for frequent hospital visits and ensures timely care.
AI also enhances resource allocation in healthcare. Predictive analytics identifies high-risk patients who require immediate attention. By focusing on these individuals, healthcare providers can optimize resources and reduce overall costs. This approach ensures that patients with urgent needs receive personalized care, improving satisfaction and outcomes.
Here’s how AI works in predictive analytics and patient monitoring:
Data Collection: Remote patient monitoring (RPM) systems gather data on vital signs, medication adherence, and lifestyle habits.
Machine Learning Algorithms: AI analyzes this data to uncover patterns and trends.
Risk Stratification: Based on these patterns, AI categorizes patients into risk groups, helping providers prioritize care.
AI-driven systems also support patient-centric care. By tailoring interventions to individual needs, these technologies enhance the quality of care you receive. Early detection of health issues not only prevents complications but also empowers you to take control of your health.
With AI, healthcare is shifting from reactive to proactive care. This innovation ensures better outcomes for patients while making healthcare systems more efficient.
Benefits of AI in Oncology Research
Enhancing Diagnostic Accuracy and Precision
Artificial intelligence improves diagnostic accuracy by analyzing medical data with unmatched precision. For example, AI tools in oncology help detect skin cancer more effectively. Without AI, healthcare practitioners achieve a sensitivity of about 75%. With AI assistance, sensitivity increases to 81.1%, while specificity improves to 86.1%. Medical students and primary care providers also see significant gains, with sensitivity rising by an average of 13 points. These advancements reduce diagnostic errors and ensure you receive timely and accurate care.
AI-powered systems also excel in imaging analysis. They identify subtle patterns in mammograms, CT scans, and MRIs that might be missed by the human eye. This capability leads to earlier cancer detection, which improves survival rates. By enhancing precision, AI transforms how you experience cancer diagnostics.
Improving Efficiency in Clinical and Research Workflows
AI streamlines workflows in oncology, saving time and resources. Traditional processes like SDTM (Study Data Tabulation Model) transformation take up to 12 weeks. With AI, this timeline reduces by 50%, completing in just six weeks. Automated data management and reporting further enhance efficiency, allowing researchers to focus on innovation rather than administrative tasks.
In clinical settings, AI predicts patient no-shows and manages appointment confirmations. This ensures smoother operations and better resource allocation. By automating repetitive tasks, AI gives healthcare providers more time to interact with you, improving the quality of care.
Advancing Personalized Medicine for Better Patient Outcomes
AI enables personalized cancer treatments tailored to your unique needs. It analyzes genetic profiles, tumor characteristics, and other data to create customized care plans. For instance, AI predicts how you might respond to specific therapies, helping oncologists choose the most effective options. This reduces side effects and improves treatment success rates.
AI also continuously learns from new data, refining its recommendations over time. This adaptability ensures that your treatment evolves with the latest advancements in oncology. By advancing personalized medicine, AI enhances your chances of recovery and long-term health.
The Role of Artificial Intelligence in Oncology Research continues to revolutionize cancer care, offering precise diagnostics, efficient workflows, and personalized treatments that improve outcomes for patients like you.
Accelerating the Drug Development Process
Artificial intelligence (AI) is transforming how new cancer treatments are developed. Traditional drug development often takes years and involves high costs. AI reduces this timeline by analyzing vast datasets quickly and identifying promising drug candidates. This efficiency allows researchers to focus on the most viable options, saving time and resources.
AI-powered platforms can simulate how drugs interact with cancer cells. These simulations predict the effectiveness of potential treatments before clinical trials begin. For example, AI models analyze molecular structures to identify compounds that target specific cancer pathways. This process eliminates the need for extensive trial-and-error experiments, accelerating the discovery phase.
You benefit from AI's ability to repurpose existing drugs. AI systems compare the properties of approved medications with cancer profiles. This approach identifies new uses for existing drugs, offering faster solutions for patients. Repurposing drugs also reduces the risks associated with developing entirely new treatments.
AI is significantly changing the landscape of drug discovery, particularly by speeding up the creation of new cancer treatments and other challenging medical conditions.
AI also improves the success rate of clinical trials. Machine learning algorithms analyze patient data to match individuals with the most suitable trials. This ensures that trials enroll participants who are more likely to respond positively, increasing the chances of success. As a result, you gain access to innovative treatments sooner.
The integration of AI into drug development is a game-changer. It shortens timelines, reduces costs, and improves the precision of cancer therapies. These advancements bring hope to millions of patients worldwide, offering faster and more effective treatment options.
Challenges in Implementing AI in Oncology
Addressing Ethical Concerns and Algorithmic Bias
AI systems in oncology often face ethical challenges, particularly when biases in training data affect outcomes. For example, an AI system designed to identify patients needing additional care mistakenly predicted healthcare costs instead. This led to worse outcomes for Black patients, as the system failed to allocate appropriate care levels. Similarly, oncology chatbots have shown biases due to non-diverse training datasets, potentially harming patients by providing inaccurate recommendations.
To address these issues, you must ensure that AI systems follow ethical principles like transparency and fairness. Using diverse datasets and implementing continuous monitoring can help reduce bias. These steps not only improve AI performance but also promote health equity in cancer care.
Ensuring Data Privacy and Security
AI technologies in oncology rely on vast amounts of patient data, raising significant privacy concerns. Many of these systems are managed by private companies, which can lead to questions about how your data is handled. Additionally, new algorithms have demonstrated the ability to reidentify anonymized patient information, increasing the risk of privacy breaches.
Concern Type | Description |
|---|---|
Private Custodianship | Private entities managing AI systems may misuse or mishandle patient data. |
Reidentification Risks | Algorithms can reidentify anonymized data, compromising patient privacy. |
Public Trust Issues | Only 11% of Americans trust tech companies with their health data. |
To protect your data, AI developers must prioritize robust security measures and transparent practices. Building public trust is essential for the successful adoption of AI in oncology.
Overcoming Integration Barriers in Clinical Settings
Integrating AI into clinical oncology presents several challenges. Busy clinic workflows often lack the flexibility needed for AI tools. For instance, some AI systems misquote literature or provide inaccurate recommendations, which can mislead clinicians. High "hallucination rates" in AI chatbots further complicate their reliability.
Regulatory uncertainties also hinder AI adoption. Without clear guidelines, healthcare providers may hesitate to implement these technologies. Additionally, the lack of diversity in training datasets can perpetuate biases, exacerbating healthcare disparities. Environmental concerns, such as the energy demands of AI systems, add another layer of complexity.
To overcome these barriers, you need well-validated AI tools and clear regulatory frameworks. Streamlining workflows and ensuring diverse training datasets can make AI more effective and equitable in oncology care.
Establishing Regulatory Standards and Oversight
The rapid growth of artificial intelligence (AI) in oncology demands clear regulatory standards. Without proper oversight, you might face risks like unreliable AI tools or inconsistent care. Establishing strong regulations ensures that AI systems meet safety, accuracy, and ethical requirements before they reach clinical settings.
Regulatory standards help you trust AI technologies. For example, the FDA evaluates AI-based medical devices to ensure they deliver accurate results. These evaluations focus on performance, data quality, and patient safety. By adhering to such standards, developers create tools that you can rely on for critical decisions.
Did you know? The FDA has already approved over 500 AI-based medical devices, many of which focus on cancer care.
Oversight also addresses the dynamic nature of AI. Unlike traditional medical devices, AI systems evolve through continuous learning. This adaptability improves performance but introduces challenges. Regulators must monitor these updates to ensure they don’t compromise safety or introduce errors. You benefit from this ongoing oversight because it keeps AI tools reliable over time.
Here’s how regulatory frameworks can improve AI in oncology:
Pre-market Evaluation: Ensures AI tools meet safety and efficacy standards before use.
Post-market Surveillance: Monitors AI performance after deployment to catch issues early.
Transparency Requirements: Mandates clear documentation so you understand how AI makes decisions.
Global collaboration is essential for consistent standards. Countries like the U.S., EU, and Japan are working together to align regulations. This cooperation ensures that AI tools meet universal benchmarks, no matter where you live.
Strong regulatory oversight protects you and ensures that AI technologies in oncology deliver safe, effective, and ethical care.
The Future of AI in Oncology Research
Emerging Trends in AI for Cancer Care
AI is rapidly evolving from algorithm development to clinical integration, transforming cancer care. You can see its impact in areas like early detection, diagnosis, and treatment optimization. For example, AI-assisted imaging now identifies cancer earlier than traditional methods, improving survival rates. It also optimizes radiation doses and supports surgical procedures, enhancing precision and safety.
AI's ability to process large genomic datasets is another game-changer. It produces actionable insights that inform personalized treatment plans. This efficiency surpasses traditional computing methods, making cancer care more effective. As AI continues to integrate into clinical practice, it addresses challenges like workflow inefficiencies and improves patient outcomes.
Innovations in AI-Driven Therapies
AI-driven therapies are revolutionizing oncology by offering precision and predictive capabilities. For instance, AI tools predict how your tumor will respond to specific drugs, enabling tailored treatments. Predictive modeling also forecasts survival outcomes for breast cancer patients using digital pathology images. These innovations ensure you receive the most effective care.
Innovation Type | Description |
|---|---|
Precision Cancer Treatment | AI tool predicts responses to cancer drugs, aiding in treatment decisions based on tumor biomarkers. |
Predictive Modeling | AI model predicts survival outcomes for breast cancer patients using digital pathology images. |
Drug Response Prediction | AI methods integrate histopathology and molecular data to enhance outcome predictions for brain cancer. |
Accelerating Drug Discovery | AI predicts T-cell responses to tumors, improving immunotherapy effectiveness. |
Understanding Drug Response Mechanisms | Predictive AI models map common drug response pathways using deep learning. |
These advancements not only improve treatment accuracy but also accelerate drug discovery, offering hope to millions of patients worldwide.
Expanding Global Access to AI in Oncology
AI is bridging gaps in cancer care, especially in low-resource settings. Systems designed to analyze medical images and assess risk are improving cancer detection where resources are limited. For example, digital pathology algorithms provide faster and more affordable tissue assessments compared to traditional methods. This makes high-quality diagnostics accessible to underserved populations.
Initiatives like the Medical Imaging and Data Resource Center (MIDRC) are also driving progress. By collecting diverse imaging data, MIDRC supports the development of AI tools for cancer detection. These efforts ensure that AI technologies benefit patients globally, regardless of their location or economic status.
AI's role in oncology research is expanding, offering innovative solutions to improve access, precision, and outcomes in cancer care.
Strengthening Collaboration Between AI and Human Expertise
Artificial intelligence (AI) works best when paired with human expertise. In oncology, this partnership enhances cancer care by combining the strengths of both. AI excels at processing large datasets and identifying patterns, while human doctors bring critical thinking and empathy to decision-making. Together, they create a powerful team that improves outcomes for patients like you.
AI systems assist radiologists by analyzing medical scans to flag potential issues. Radiologists then review these flagged areas to confirm or refine the diagnosis. This collaboration increases cancer detection rates and reduces the chances of missing abnormalities. For example:
AI imaging tools help radiologists identify early-stage cancers in mammograms and CT scans.
Human doctors make the final diagnostic decisions, ensuring accuracy and reliability.
In personalized treatment planning, AI analyzes vast databases of patient outcomes to suggest tailored therapies. Oncologists use these insights to design treatment plans that suit your unique needs. At the Dana-Farber Cancer Institute, IBM Watson for Oncology demonstrated this synergy. Watson analyzed genetic profiles and medical records to recommend personalized treatments. Impressively, 90% of its recommendations aligned with the tumor board's decisions for breast cancer patients. Watson also delivered these suggestions in just 40 seconds, compared to the 20 minutes required by manual methods.
Did you know? AI doesn’t replace doctors—it empowers them. By handling repetitive tasks, AI allows oncologists to focus on what matters most: providing compassionate care.
This collaboration ensures that you benefit from both cutting-edge technology and human judgment. As AI continues to evolve, its partnership with healthcare professionals will only grow stronger, offering you more precise and effective cancer care.
The role of artificial intelligence in oncology research has transformed cancer care. You now benefit from enhanced diagnostic accuracy, especially in breast cancer pathology and tumor identification. AI surpasses traditional methods in grading and treatment predictions, improving outcomes. Despite challenges like ethical concerns and data security, AI continues to revolutionize oncology. Its ability to combine advanced technology with human expertise ensures better care for you. As AI evolves, it promises to make cancer treatment more precise, accessible, and effective, offering hope for a future where cancer care is significantly improved.
FAQ
What is the role of AI in cancer detection?
AI helps detect cancer early by analyzing medical images like mammograms and CT scans. It identifies patterns that might be missed by the human eye. This improves accuracy and ensures you receive timely diagnoses, which can significantly increase survival rates.
How does AI personalize cancer treatments?
AI analyzes your genetic data, tumor characteristics, and medical history to recommend treatments tailored to your needs. This ensures you receive therapies that are most effective for your condition, reducing side effects and improving outcomes.
Can AI replace doctors in oncology?
No, AI supports doctors by handling repetitive tasks and analyzing large datasets. It provides insights that help doctors make better decisions. You still benefit from the expertise and empathy of healthcare professionals working alongside AI.
Is AI safe to use in cancer care?
Yes, AI tools undergo rigorous testing and regulatory approval to ensure safety and accuracy. For example, the FDA has approved many AI-based devices for cancer care. Developers also monitor these tools to maintain their reliability over time.
How does AI improve drug discovery for cancer?
AI speeds up drug discovery by analyzing vast datasets to identify promising compounds. It predicts how drugs interact with cancer cells, reducing trial-and-error experiments. This accelerates the development of new treatments, giving you access to innovative therapies faster.
Tip: AI doesn’t just make cancer care faster—it makes it smarter, ensuring you receive the best possible treatment.
See Also
An In-Depth Overview of Various Cancer Types
Key Characteristics of Glioblastoma You Need to Know
Exploring Islet Cell Carcinoma Within The Endocrine Pancreas
Recognizing Symptoms and Treatments for Conjunctival Melanoma
Essential Information About Carcinoid Tumors You Should Have

