Should Gene Editing be Used in Cancer Treatment for a Brighter Future?
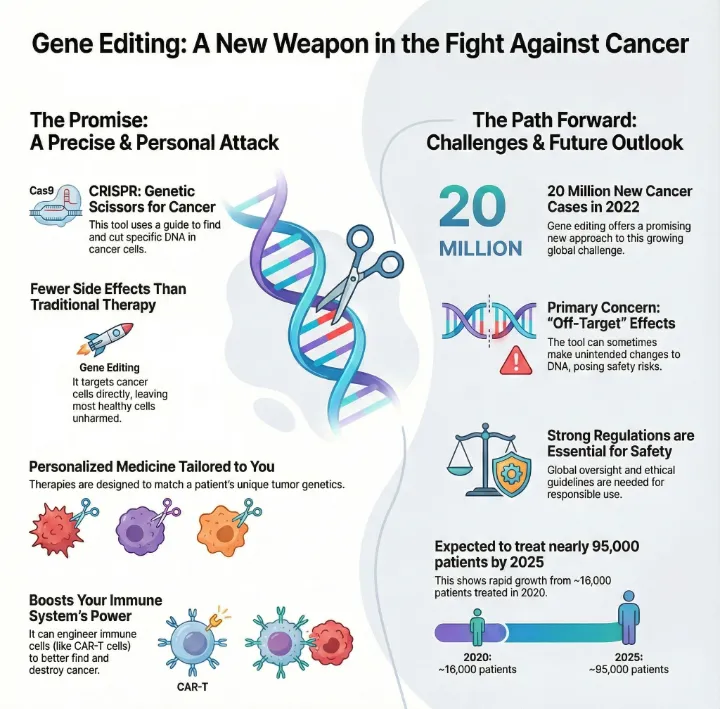
Gene editing is already being used in carefully controlled cancer clinical trials and shows promising results. Gene editing opens new doors for cancer care and brings hope to millions. Cancer affects people everywhere. In 2022, doctors diagnosed about 20 million new cases worldwide. Nearly 9.7 million people died from cancer that year. Experts predict cancer cases could reach 35 million by 2050. You can help shape a brighter future by supporting advanced treatments and using technology wisely.
Key Takeaways
Gene editing, especially CRISPR, offers precise targeting of cancer cells, leading to more effective treatments.
Personalized cancer therapies can be developed using genomic testing, allowing treatments tailored to individual patients.
New gene editing methods reduce side effects compared to traditional therapies, improving patient quality of life.
CRISPR enhances immune cell function, making them more effective at fighting cancer.
Support for strong regulations and ethical practices is essential for the safe use of gene editing in cancer treatment.
Should Gene Editing be Used in Cancer Treatment?

How Gene Editing Targets Cancer
You want answers to the question: Should Gene Editing be Used in Cancer Treatment? You deserve to know how this technology works. Gene editing, especially CRISPR, gives you a powerful tool to fight cancer at its roots. CRISPR uses a guide RNA to find the exact spot in your DNA that needs fixing. The Cas9 enzyme then cuts the DNA at that location. This process lets doctors change, add, or remove genetic material with high precision.
You benefit from new delivery systems that use lipid nanoparticles. These tiny carriers bring CRISPR components directly to tumors. Anti-EGFR antibodies coat the nanoparticles, helping them target cancer cells that express the epidermal growth factor receptor. This means you get treatment that attacks cancer cells while sparing healthy ones.
Tip: Precision matters. CRISPR can inactivate genes that drive cancer or add new DNA segments to repair faulty genes. It can even detect DNA from cancer-causing viruses and RNA from cancer cells.
Recent advances like base editing and prime editing allow you to change single DNA letters or modify genetic sequences without causing double-strand breaks. These improvements lower the risk of unwanted changes and make treatments safer.
You should consider these main arguments for gene editing in cancer treatment:
Gene editing offers high precision in targeting cancer cells.
It helps overcome drug resistance, a major challenge in cancer therapy.
The approach supports personalized medicine, tailoring treatments to your unique genetic profile.
New editing methods like base editing and prime editing improve safety and accuracy.
Integration with immunotherapies, such as CAR-T cells, boosts antitumor responses.
CRISPR and Immune Cell Engineering
Should Gene Editing be Used in Cancer Treatment? You see the answer in the way CRISPR transforms your immune system. Researchers use CRISPR to edit immune cells, making them better at finding and attacking cancer. For example, scientists can knock out genes that slow down immune responses. This boosts your body's ability to fight cancer.
You benefit from improved antigen presentation. CRISPR upregulates genes linked to MHC class I molecules, helping your immune cells show tumor-specific antigens more clearly. Doctors can also knock down the PD-1 gene in T cells. This change increases T cell activation and enhances their toxicity against cancer cells.
Here is how CRISPR technology modifies immune cells to help you:
Knocks out genes that inhibit immune responses.
Improves antigen presentation for better tumor recognition.
Directly knocks down PD-1 in T cells, increasing their cancer-fighting power.
Allows precise genetic modifications to optimize engineered T cells.
You may wonder about real-world results. Clinical trials show promising outcomes. In a recent Phase I trial, doctors infused CRISPR-engineered T cells into patients with advanced cancers. The engineered cells traveled to tumor sites and made up 2-20% of immune cells in the tumors. Biopsies showed a reduction in target antigens, and some patients saw tumor regression.
Outcome Description | Details |
|---|---|
Trial Design | Phase I trial assessing safety and feasibility of CRISPR-engineered T cells in cancer patients. |
Patient Demographics | Three patients: two with refractory advanced myeloma, one with refractory metastatic sarcoma. |
Tumor Response | Engineered T cells trafficked to tumor sites; reduction in target antigens in myeloma patients. |
Cytotoxicity Assessment | Antigen-specific cytotoxicity observed 3 to 9 months post-infusion. |
Tumor Regression | Notable tumor regression in one patient after infusion. |
Side Effects | Expected side effects from chemotherapy; transient fevers and chills in two patients. |
You see early signs of clinical activity and tumor reduction. Should gene editing be used in cancer treatment? Gene editing is already being used in carefully controlled cancer clinical trials and shows promising results. Early studies suggest the potential for better outcomes and fewer side effects.
You should also know about CAR-T cell therapies. CRISPR helps create autologous CAR-T cells, which show long-lasting benefits. These therapies are expensive and time-consuming, but researchers are developing allogeneic CAR-T cells for a scalable solution. Initial high response rates have been observed, though challenges like immune rejection remain.
You have the power to support this technology. Should Gene Editing be Used in Cancer Treatment? You can help shape the future by advocating for safe, effective, and accessible gene editing therapies.
Benefits of Gene Editing in Oncology
Precision and Fewer Side Effects
You want cancer treatment that works for you, not against you. Gene editing gives you that chance. CRISPR/Cas9 and other advanced tools let doctors change your DNA with incredible accuracy. You get targeted therapy that attacks cancer cells while leaving healthy cells alone. This precision means you face fewer side effects than with chemotherapy or radiation.
Advances in guide RNA design and delivery methods help doctors avoid mistakes. These improvements make gene editing safer for you. CRISPR/Cas9 allows for specific changes to the cancer genome, so you get treatment that fits your needs. Doctors can now reduce off-target effects, which are a big problem in traditional therapies.
You may worry about side effects. Most gene editing therapies cause fewer problems than older treatments. Sometimes, unintended gene changes or immune responses happen, but researchers work hard to make these risks smaller. You deserve safer options, and gene editing brings you closer to that goal.
Gene editing therapies, especially CRISPR, can improve survival rates and quality of life for people with tough cancers like pancreatic cancer.
These therapies target specific mutations, giving you better results than conventional treatments.
Combining gene editing with standard care can boost your chances of beating cancer.
Personalized Cancer Therapies
You are unique, and your cancer is too. Gene editing lets doctors create treatments just for you. Genomic testing finds the exact mutations in your tumor. Doctors use this information to design therapies that block cancer growth signals and stop altered proteins.
CRISPR/Cas9 can change cancer or immune cells based on your tumor’s genetic profile.
CAR-T cell therapy engineers your T cells to recognize and attack your specific cancer.
New gene-editing tools help researchers study genetic changes and find the best therapy for you.
You see real-life success stories. Bryce Olson, a patient with advanced prostate cancer, used personalized genomic data to guide his therapy. He lived longer and enjoyed a better quality of life. Should Gene Editing be Used in Cancer Treatment? You see how personalized approaches give hope and real results.
You have the power to choose treatments that fit your body and your life. Gene editing makes personalized cancer care possible.
Risks and Ethics of Gene Editing
Safety and Ethical Issues
You want safe and trustworthy cancer treatments. Gene editing brings hope, but you must understand the risks. Sometimes, gene editing tools like CRISPR can make changes in the wrong place. These off-target effects may create faulty proteins. Your body could react with strong immune responses or inflammation. This can lead to serious health problems, such as heart attacks or strokes.
You may also face other dangers:
Hyperactive immune reactions can damage your organs.
Overactive cell death can harm healthy cells and cause lasting problems.
If gene editing changes the wrong gene, it could even create new cancers.
Note: Off-target effects can slow down clinical trials and delay new treatments for you.
You should also think about the ethics. Changing your genes raises big questions. Some people worry that gene editing changes what it means to be human. Editing genes in eggs or sperm could limit your freedom or change future generations forever. You might lose genetic diversity, which helps humans survive.
Some say gene editing could hurt human dignity.
Others ask if it is right to change lives before birth.
Many believe gene editing could help end diseases, but you must consider safety and consent.
The debate continues. You need strong rules to protect yourself and others.
Regulatory and Technical Barriers
You want treatments that follow strict rules. Different countries have their own systems:
Region | Regulatory Body/Framework | Key Features |
|---|---|---|
United States | FDA, NIH, CDC | Many laws control drug approval and clinical trials. |
China | NHC, NMPA, MoST | Clear rules separate therapy from enhancement; only therapy gets approval. |
United Kingdom | HFEA | One main authority; no germline editing allowed in clinics. |
You also face technical barriers. Delivering gene editing tools into your cells is hard. The tools are large and unstable. They have trouble crossing cell membranes. Some methods, like electroporation, can damage cells and need special machines. Microinjection is precise but slow and costly. Viral vectors cannot carry large genes.
You deserve safe, effective, and fair access to gene editing. You must support strong rules and better technology for a brighter future.
Future Impact on Cancer Care
Transforming Treatment Strategies
You stand at the edge of a new era in cancer care. Gene editing, especially CRISPR, will change how you fight cancer. You will see treatments designed just for you. Doctors will use your unique genetic code to target cancer cells with precision. This approach moves away from one-size-fits-all treatments. You will not have to settle for therapies that do not match your needs.
CRISPR technology will let doctors edit the exact genes that cause your cancer.
You will get therapies that match your tumor’s mutations, not someone else’s.
New tools will help doctors sort patients in real time and find the best drugs for you.
You will benefit from faster drug development and more treatment options.
You will notice more people getting gene therapy. The number of patients treated with gene therapies will rise from about 16,000 in 2020 to nearly 95,000 in 2025. You will see spending on these therapies reach over $2 billion a month by 2026. Over time, costs will go down, but the benefits will last. You could gain more than five extra years of life from these treatments.
You deserve hope. Gene editing gives you a real chance for longer, healthier years.
Steps for Responsible Adoption
You want safe and ethical care. You must support strong rules for gene editing. You need doctors and researchers to protect you and your community. Best practices help keep you safe during clinical trials.
Doctors should tell you about all risks, including those that affect others, before you join a trial.
Researchers must share risk information and safety plans with all staff involved in your care.
You should get clear instructions on how to reduce risks to others, written in simple language.
You play a role in shaping the future. Ask questions. Demand transparency. Support policies that put your safety first. When you do, you help make gene editing a tool for good.
You can help build a future where cancer care is safer, smarter, and more personal.
You see gene editing as a powerful tool for cancer care. You benefit from safer treatments, fewer side effects, and therapies designed just for you.
CRISPR improves immune cell function and helps stop cancer growth.
New editing methods make treatments more precise.
Some risks remain, like unwanted genetic changes. Experts urge strong rules and public debate to guide safe use.
Principle | Description |
|---|---|
Governance | |
Public Engagement | Policy debates include many voices |
Ethical Oversight | Societal values shape clinical decisions |
You can support research and join conversations. You help build a future where cancer care is smarter and safer.
FAQ
What is gene editing and how does it help you fight cancer?
Gene editing changes your DNA to fix or remove harmful genes. You get targeted treatment that attacks cancer cells. This approach gives you hope for better results and fewer side effects.
Is gene editing safe for you?
You face some risks, like unwanted genetic changes. Researchers work hard to make treatments safer.
You should always ask your doctor about safety before starting gene editing therapy.
Can you get gene editing treatment for any type of cancer?
You may not qualify for every cancer type. Doctors use gene editing mostly for blood cancers and some solid tumors.
Ask your doctor if gene editing fits your diagnosis.
How much does gene editing therapy cost you?
Gene editing therapy costs a lot right now. Prices may drop as technology improves.
Therapy Type | Estimated Cost |
|---|---|
CAR-T Cells | $400,000+ |
CRISPR Trials | $10,000–$50,000 |
This article is for educational purposes only and is not a substitute for professional medical advice. For more details, please see our Disclaimer. To understand how we create and review our content, please see our Editorial Policy.
See Also
Recognizing Duodenal Cancer: Key Symptoms and Treatment Options
An In-Depth Overview of Various Types of Cancer
Choriocarcinoma: Definition, Symptoms, and Treatment Approaches
Understanding Carcinoid Tumors: Essential Information for Patients
Conjunctival Melanoma: Symptoms to Watch and Treatment Options

