New Breast Cancer Biomarker: Stromal Disruption Identified

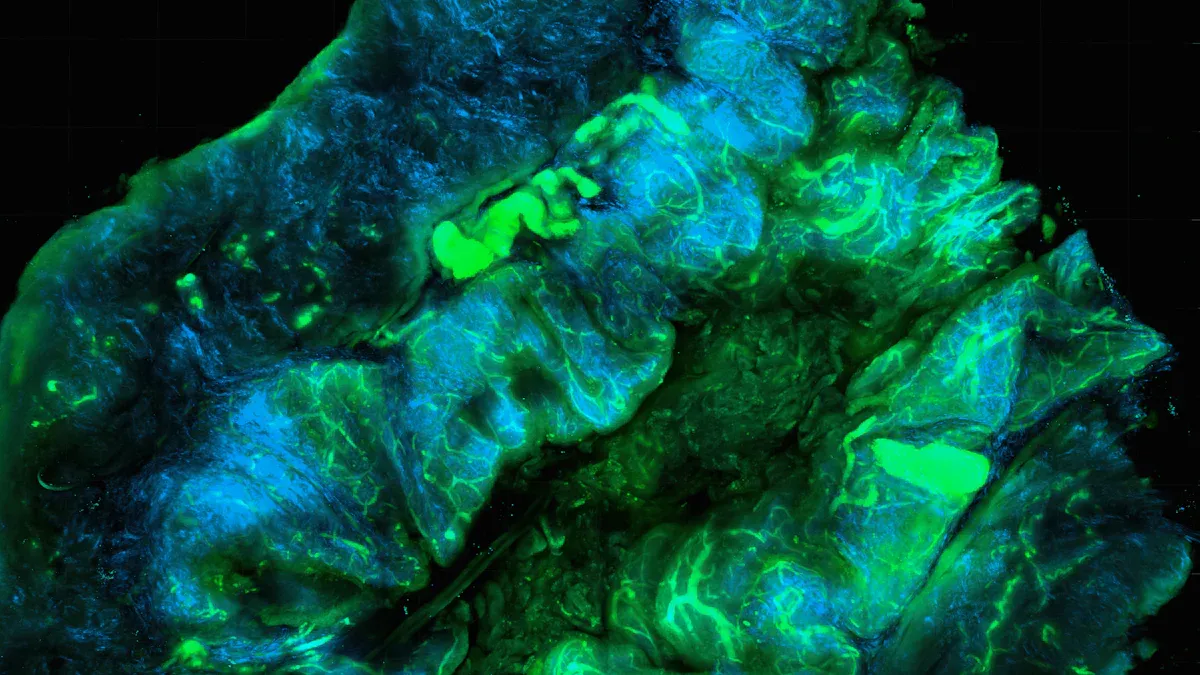
Scientists have identified stromal disruption in breast cancer as a key biomarker for aggressive disease risk. Stromal disruption refers to changes in the tissue surrounding breast cells, including alterations in the immune system and cell structure.
Breast
This disruption strongly links to high-grade tumors, faster cancer development, and poorer survival, especially in estrogen receptor-positive cases.
Risk factors such as younger age, multiparity, Black race, obesity, and family history often show increased stromal disruption.
Machine learning now allows for practical, cost-effective detection using large, diverse patient samples.
Key Takeaways
Stromal disruption means harmful changes in the tissue around breast cells that raise the risk of aggressive breast cancer.
Machine learning helps doctors detect stromal disruption quickly and affordably from tissue samples, improving early diagnosis.
Risk factors like younger age, obesity, Black race, and family history often link to stromal disruption and higher cancer risk.
Stromal disruption weakens natural barriers, allowing cancer to grow and spread, making it a key target for new treatments.
Early detection of stromal disruption can guide personalized care and prevention, improving survival and reducing recurrence.
Stromal Disruption in Breast Cancer
What Is Stromal Disruption?
Stromal disruption in breast cancer describes a series of changes in the connective tissue, or stroma, that surrounds breast cells. Scientists define this process as alterations in both the structure and cellular makeup of the breast’s supportive tissue. The mammary stroma contains many cell types and extracellular matrix components. These elements communicate with the breast’s epithelial cells, guiding normal development and repair. When stromal disruption occurs, this communication breaks down. The tissue may show signs of chronic inflammation and abnormal wound healing. Researchers have found that these changes can influence how breast cancer develops and spreads.
Several cellular and molecular changes mark stromal disruption in breast cancer:
The architecture and cellular composition of the stroma shift.
Chronic inflammation becomes more common.
Mesenchymal stromal cells change how they produce cytokines, chemokines, and growth factors.
These changes link to higher risk and more aggressive forms of breast cancer.
Chemotherapy can further alter the stroma, affecting cell survival and secretory activity.
The stroma does not just support breast tissue; it actively shapes cancer risk and progression.
Why It Matters
Stromal disruption in breast cancer plays a critical role in how tumors form and grow. Normally, myoepithelial cells and the basement membrane act as barriers, stopping cancer cells from invading nearby tissue. When stromal disruption occurs, these barriers weaken or disappear. This loss allows tumor cells to invade and spread. Stromal cells, such as fibroblasts and carcinoma-associated fibroblasts, begin to secrete factors that help tumors grow, invade, and form new blood vessels.
Tumor-associated macrophages in the stroma promote invasion and metastasis.
Changes in the extracellular matrix, like increased collagen and stiffness, make the tissue more likely to support cancer.
Researchers now see the stroma as an active player in breast cancer, not just a bystander. By understanding and detecting stromal disruption in breast cancer, doctors can better predict which patients face higher risks and may need more aggressive care.
Study Overview

Research Methods
Researchers designed a large, multi-institutional study to investigate stromal disruption in breast cancer. They collected breast tissue samples from thousands of women with diverse backgrounds. Scientists used advanced molecular biology and bioinformatics techniques to detect and measure stromal disruption at the genetic level. The main steps included:
Transcriptomics Analysis: Scientists extracted RNA from both stromal and epithelial cells. They used microarray and RNA sequencing to study gene expression.
Data Preprocessing: The team normalized the data and mapped gene IDs to prepare for analysis.
Exploratory Data Analysis: Principal Component Analysis (PCA) helped visualize differences between cancerous and normal tissues.
Differential Gene Expression: Researchers identified genes that were up- or down-regulated in disrupted stroma using statistical tests.
Clustering and Visualization: Hierarchical clustering and heatmaps revealed patterns in gene expression.
Gene Enrichment Analysis: The team used software to interpret which biological pathways were affected.
Laser Capture Microdissection: This technique allowed precise separation of stromal and epithelial compartments for detailed study.
To ensure reliable results, the study confirmed that measurements remained consistent across four different laboratories. The researchers also used both human and mouse cells, and validated their findings with molecular studies.
The study’s use of machine learning, such as the CollaTIL framework, enabled automated detection of stromal disruption from digital pathology slides. This approach proved practical and accurate, with over 90% of results rated as good or fair by expert pathologists.
Key Risk Factors
The study identified several risk factors that strongly associate with stromal disruption:
Multiparity (having given birth to more than one child)
Black race
Obesity
Family history of breast cancer
These factors often appear before tumor development, suggesting a shared pathway in the stroma that leads to aggressive breast cancer. The findings imply that lifestyle changes and anti-inflammatory treatments could help lower risk.
Aspect | Stromal Disruption (TSR) | Traditional Risk Factors |
|---|---|---|
Prognostic Value | Strongly predicts survival and response to therapy, especially in aggressive subtypes | Useful but limited in predicting outcomes for all patients |
Clinical Use | Non-invasive, cost-effective, and practical for widespread screening | Well-established but may miss microenvironment effects |
Including women from many racial and demographic groups made the study’s results more generalizable. This diversity ensures that new detection methods and therapies will benefit a broad range of patients.
Findings and Implications
Benign and Invasive Cases
Researchers found that stromal disruption in breast cancer can appear even before a tumor forms. In benign breast tissue, an increased epithelium-to-stroma proportion (ESP) signals a higher risk for future cancer, especially in women with nonproliferative benign breast disease. About 70% of benign breast disease cases fall into this category. When the epithelial area increases and the ESP rises in benign biopsies, the odds of developing invasive breast cancer also increase. In contrast, a larger stromal area in benign tissue links to a lower risk.
The study also showed that stromal disruption in invasive breast cancer differs from benign conditions. In invasive cases, the stroma contains immune cells, such as mast cells, which are not present in benign tissue. Patients with mast cell infiltration in the stroma tend to have better outcomes. Invasive tumors also show unique gene expression changes, including higher levels of integrins and matrix metalloproteinases, and lower levels of laminins. These changes reflect active remodeling of the tissue around the tumor. Some benign lesions, like radial scars, share certain features with invasive cancers, but the overall pattern of stromal disruption in invasive disease is more complex and involves additional immune and molecular changes.
The presence and type of stromal disruption in breast tissue help doctors predict which patients face a higher risk of aggressive cancer.
Survival and Outcomes
Stromal disruption in breast cancer strongly influences patient survival and disease progression. Scientists identified four main stromal cell types in triple-negative breast cancer: two fibroblast-like and two perivascular-like cells. Patients with a low inflammatory cancer-associated fibroblast signature and high cytotoxic T lymphocyte infiltration had better survival rates. In contrast, high inflammatory fibroblast signatures linked to poor immune response and worse outcomes. Differentiated perivascular-like cells also related to lower immune cell presence and potentially poorer survival.
Stromal gene expression profiles correlate with higher tumor grade and worse clinical outcomes.
Tumor stroma dysregulation plays a key role in cancer progression, immune evasion, and treatment resistance.
A low stromal ratio, especially after chemotherapy, predicts shorter recurrence-free survival and higher risk of metastasis.
These findings highlight the importance of the tumor microenvironment in shaping cancer behavior. The ability to assess stromal disruption in breast cancer provides doctors with a powerful tool to identify high-risk patients and tailor their care.
Prevention and Treatment
The discovery of stromal disruption in breast cancer as a key biomarker opens new doors for prevention and therapy. Doctors can now identify women at higher risk by examining changes in the stroma, even before cancer develops. This allows for early intervention and closer monitoring.
Prevention strategies may focus on reducing inflammation in breast tissue. Chronic inflammation and abnormal wound healing drive stromal disruption, so lifestyle changes and anti-inflammatory medications could help lower risk. Regular use of aspirin, for example, has been linked to reduced breast cancer risk, especially in aggressive subtypes. Higher levels of anti-inflammatory markers in breast tissue also associate with lower cancer risk.
New treatment approaches target the stromal microenvironment directly. Researchers are testing therapies that combine ultrasound with drugs that normalize the stroma. These treatments reduce tumor stiffness, improve blood flow, and boost the effectiveness of immunotherapy. In animal studies, this strategy led to smaller tumors, complete cures, and lasting immune protection. Machine learning helps identify which patients will benefit most from these therapies by analyzing tumor stiffness and immune cell patterns.
The identification of stromal disruption in breast cancer as a biomarker supports precision medicine. Doctors can now match patients to therapies that target both the tumor and its surrounding environment, improving outcomes and reducing the risk of recurrence.
The ability to detect stromal disruption using cost-effective methods means that these advances can reach more patients, including those in low-resource settings. This breakthrough has the potential to transform breast cancer prevention, diagnosis, and treatment worldwide.
Researchers have shown that stromal disruption in breast cancer offers a strong signal for aggressive disease and poor survival.
Artificial intelligence now helps doctors detect these changes in tissue samples from thousands of women.
The stroma’s role in tumor growth and immune response makes it a promising target for new treatments and prevention strategies.
Future studies should use advanced models and standardized methods to better understand how stromal changes affect risk and therapy response.
Early detection and targeted care based on stromal disruption could improve outcomes for high-risk groups.
FAQ
What is stromal disruption in breast tissue?
Stromal disruption means changes in the tissue that supports breast cells. These changes include inflammation and altered cell structure. Scientists link these changes to a higher risk of aggressive breast cancer.
How do doctors detect stromal disruption?
Doctors use digital pathology slides and machine learning tools to spot stromal disruption. These methods analyze tissue samples quickly and accurately. The process is cost-effective and works well in many settings.
Why does stromal disruption increase cancer risk?
Stromal disruption weakens the barriers that protect breast tissue. This allows cancer cells to invade and spread. The disrupted stroma also supports tumor growth and makes treatment harder.
Can lifestyle changes reduce stromal disruption?
Healthy habits, such as regular exercise and a balanced diet, may lower inflammation in breast tissue. Some studies suggest that anti-inflammatory medicines could help reduce risk, but patients should always consult a doctor first.
Who benefits most from stromal disruption testing?
Women with risk factors like obesity, family history, or certain racial backgrounds may benefit most. Early detection helps doctors plan better prevention and treatment strategies for these groups.
See Also
Understanding Invasive Lobular Carcinoma And Its Symptoms
A Clear Guide To Causes Of Gastrointestinal Stromal Tumors
Key Characteristics And Facts About Glioblastoma Tumors
Recognizing Symptoms Of Inflammatory Breast Cancer Explained

