Understanding the Symptoms and Causes of Anal Cancer
Anal cancer is a rare but serious condition that develops in the tissues of the anal canal. Although it accounts for a small percentage of cancer cases worldwide, its incidence has been rising steadily in recent years. For example:
Incidence rates increased by 1.3% annually from 2012 to 2021.
Mortality rates rose by 5.1% each year from 2013 to 2022.
Recognizing symptoms early can improve outcomes significantly. If you notice changes like rectal bleeding or a lump near the anus, consult a doctor promptly. While not all changes indicate cancer, early detection plays a crucial role in effective treatment.
Key Takeaways
Know the early signs of anal cancer like bleeding, pain, or bumps. Finding it early can help treatments work better.
Learn how HPV affects anal cancer. Getting the HPV vaccine can lower your risk by 90%. Ask your doctor about the vaccine.
Live healthier to reduce your risk. Stop smoking, eat good food, and practice safe sex to stay healthier.
Keep track of your health history. Regular doctor visits and tests are important, especially if cancer runs in your family.
See a doctor for serious or lasting symptoms. If symptoms last over two weeks or get worse, visit a doctor right away.
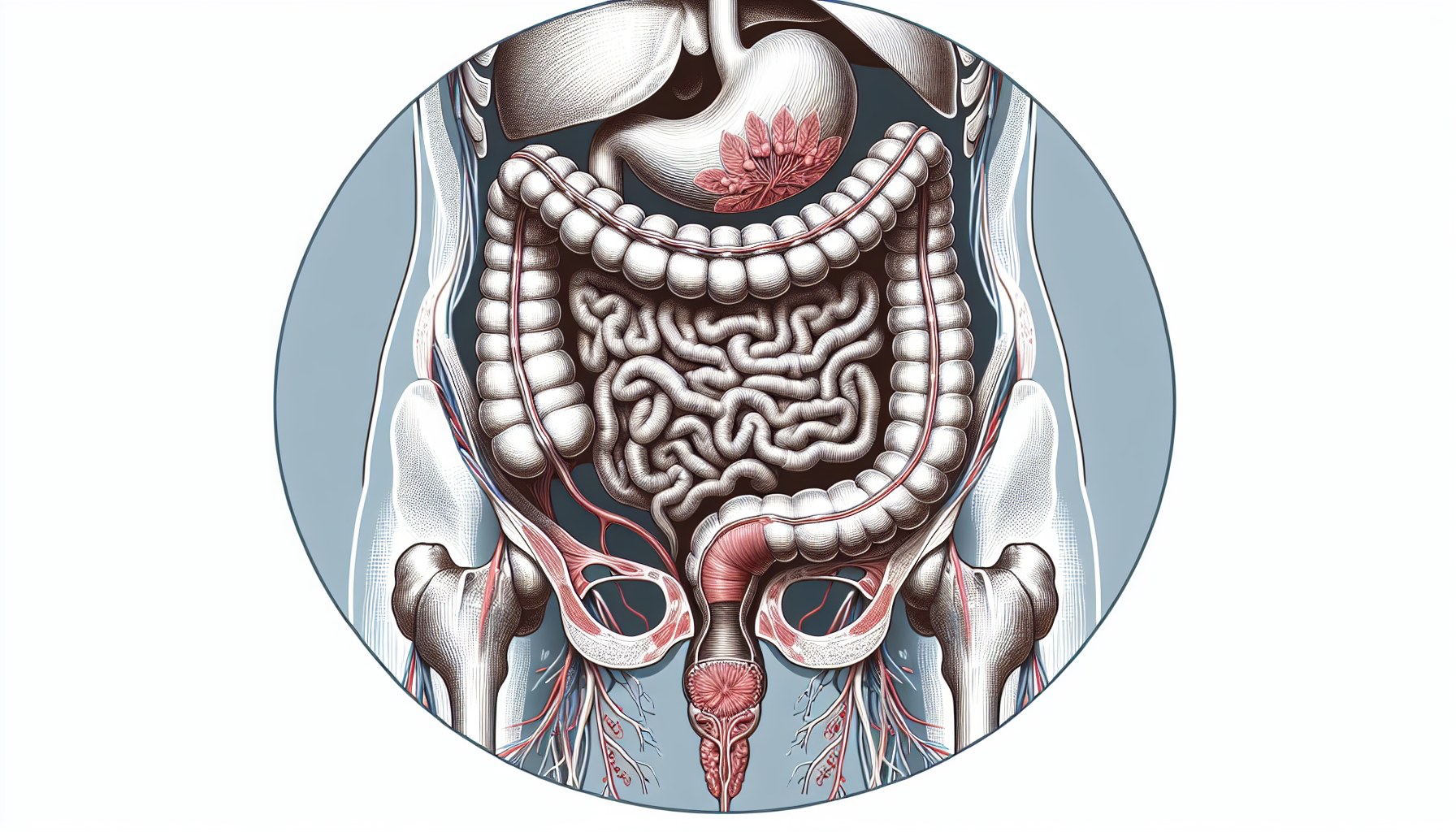
Symptoms of Anal Cancer
Common Symptoms
Recognizing the symptoms of anal cancer early can make a significant difference in treatment outcomes. Some of the most commonly reported symptoms include:
Rectal bleeding or blood in stool: You may notice bright red blood on toilet paper or in the toilet bowl after a bowel movement.
Pain or discomfort in the anal area: This can feel like a persistent ache or pressure, especially during bowel movements.
Persistent itching or irritation: Severe itching (pruritus) around the anus is a frequent complaint.
Changes in bowel habits: Stools may become narrower, or you might experience incontinence or looser stools.
Lump or mass near the anus: A lump or swelling in or around the anus is a common sign. Swelling in the groin area may also occur if lymph nodes are affected.
Note: These symptoms can overlap with other conditions like hemorrhoids or infections. However, if they persist, you should consult a healthcare provider.
Additional Symptoms
In some cases, anal cancer may cause systemic symptoms that affect your overall health. These include:
Unexplained weight loss: Losing weight without trying could indicate a more serious issue.
Fatigue or weakness: Feeling unusually tired or weak may result from the body fighting the disease.
Swollen lymph nodes in the groin area: This can occur when cancer spreads to nearby lymph nodes.
Condition | Symptoms Specific to Condition |
|---|---|
Anal Cancer | |
Lumps in or around the anus | |
Pain during bowel movements | |
Colorectal Cancer | Abdominal pain |
Bloating | |
A feeling that the bowels don’t empty completely |
Understanding these symptoms can help you differentiate anal cancer from other colorectal conditions. If you experience any of these signs, seek medical advice promptly.
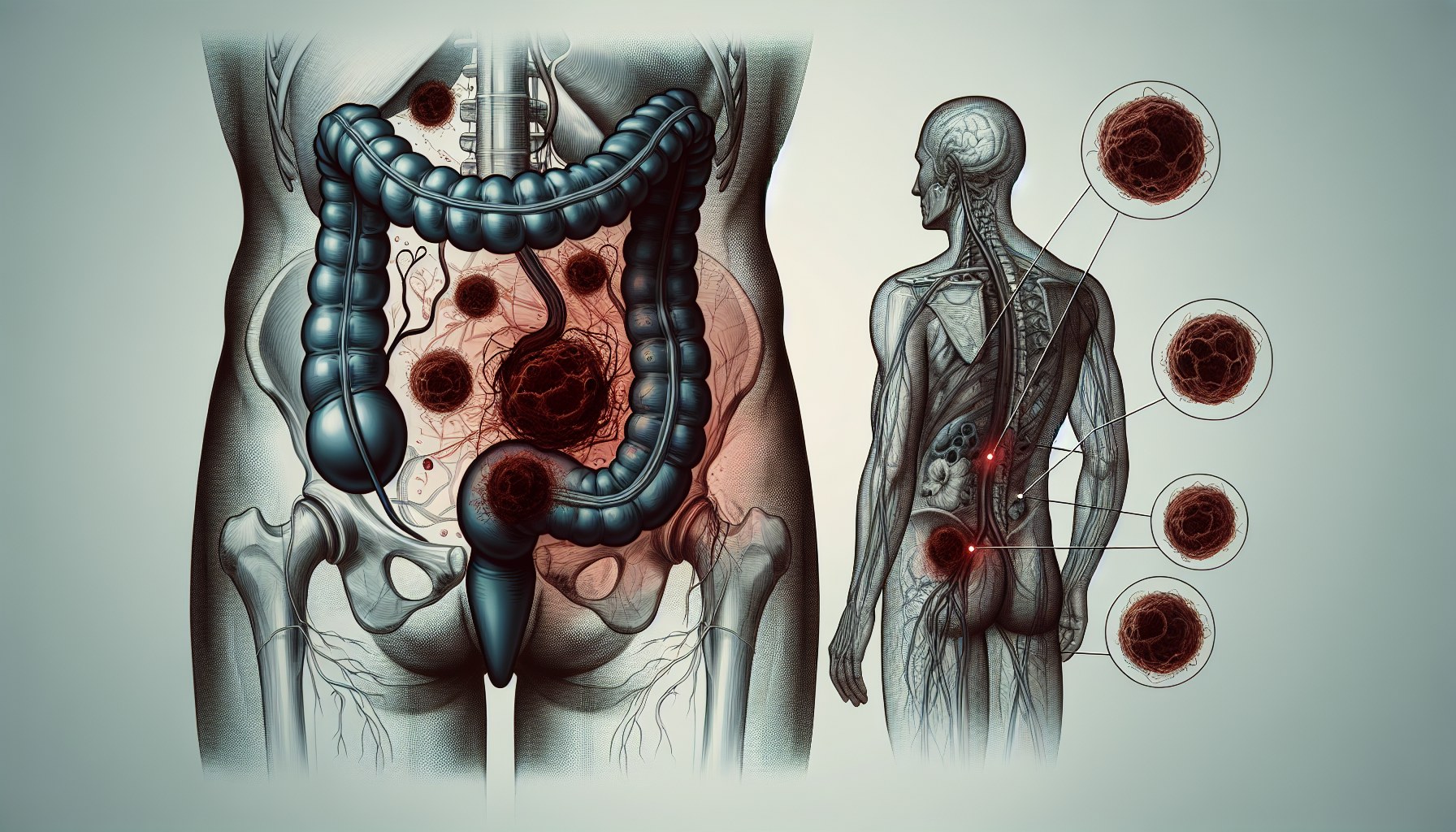
Causes of Anal Cancer
Human Papillomavirus (HPV)
Human Papillomavirus (HPV) plays a significant role in the development of anal cancer. About 90% of anal cancer cases occur in individuals with detectable HPV infections. Oncogenic strains of HPV, such as HPV-16 and HPV-18, are particularly dangerous. These strains can cause cellular changes in the anal canal, leading to squamous cell carcinoma. If you have a weakened immune system, the risk of persistent HPV infection and subsequent cancer increases.
A 2009 meta-analysis revealed that HPV-16 was present in nearly two-thirds of invasive squamous cell lesions, while HPV-18 accounted for about 5%. This highlights the importance of understanding HPV's role in anal cancer and taking preventive measures, such as vaccination, to reduce your risk.
Smoking and Tobacco Use
Smoking significantly increases your risk of developing anal cancer. Studies show that current smokers face a much higher risk compared to non-smokers. For instance, a case-control study found a ninefold increase in risk for male smokers and an eightfold increase for female smokers. The risk also rises with a higher pack-year history, meaning the more you smoke over time, the greater your chances of developing this cancer.
Smoking not only damages your immune system but also makes it harder for your body to fight off HPV infections. If you smoke and have multiple sexual partners who also smoke, your risk of anal cancer becomes even higher. Quitting smoking can greatly reduce your risk and improve your overall health.
Chronic Inflammation or Anal Conditions
Chronic inflammatory conditions and autoimmune disorders can also contribute to anal cancer. Diseases like Crohn's disease and psoriasis are associated with a higher risk. For example, individuals with Crohn's disease have a standardized incidence ratio (SIR) of 3.1, while those with psoriasis share the same SIR.
Condition | Standardized Incidence Ratio (SIR) | 95% Confidence Interval (CI) |
|---|---|---|
Crohn disease | 3.1 | 1.2–6.4 |
Psoriasis | 3.1 | 1.8–5.1 |
Polyarteritis nodosa | 8.8 | 1.5–29.0 |
Wegener granulomatosis | 12.4 | 2.1–40.8 |
Autoimmune conditions may increase your risk due to the diseases themselves or the treatments used to manage them. If you have a chronic inflammatory condition, regular checkups can help detect any abnormalities early.
Genetic Mutations
Genetic mutations play a critical role in the development of anal cancer. These mutations alter the normal functioning of cells, leading to uncontrolled growth and tumor formation. One of the most significant genetic changes linked to anal cancer involves the Pik3ca gene.
Activating mutations in the Pik3ca gene are present in about 20% of anal cancer cases.
These mutations increase the likelihood of developing cancer, whether or not HPV is involved.
Research shows that Pik3ca mutations can cause anal cancer even without exposure to chemical carcinogens.
These findings highlight how genetic changes can independently drive cancer development. If you have a family history of cancer, you might carry inherited mutations that increase your risk. While not all genetic mutations are inherited, some arise spontaneously due to environmental factors or errors during cell division.
Tip: If you know your family has a history of cancer, consider genetic counseling. It can help you understand your risk and explore preventive measures.
Understanding the role of genetic mutations emphasizes the importance of early detection. Regular screenings and discussions with your doctor can help identify potential risks before they progress. By staying informed, you can take proactive steps to protect your health.
Risk Factors for Anal Cancer
Age and Gender
Your risk of developing anal cancer increases with age. The average age of diagnosis is 64 years. Women are slightly more likely to develop this cancer than men. This gender difference may be due to hormonal factors or a history of other cancers.
Gender | Rate of New Cases per 100,000 Persons |
|---|---|
Males | 1.6 |
Females | 2.3 |
Women with a history of cervical, vaginal, or vulvar cancer face a higher risk of anal cancer. This connection is often linked to persistent HPV infections. Men, however, do not experience the same increased risk from these cancers.
Sexual Activity and HPV Exposure
HPV infection is the most significant risk factor for anal cancer. This virus spreads through skin-to-skin contact, especially during sexual activities. Certain behaviors increase your risk of HPV exposure, including:
Having multiple sexual partners.
Engaging in receptive anal intercourse.
Chronic infections with high-risk HPV types.
Most squamous cell anal cancers are directly linked to HPV. If you practice safe sex and consider HPV vaccination, you can reduce your risk significantly.
Lifestyle Factors
Your lifestyle choices can also influence your risk of anal cancer. Smoking, for instance, damages your immune system and makes it harder to fight off HPV infections. The more you smoke, the higher your risk becomes. Other factors include:
Having multiple sexual partners, which raises the likelihood of HPV and HIV infections.
Engaging in receptive anal sex, which increases risk for both men and women.
By quitting smoking and adopting safer sexual practices, you can lower your chances of developing anal cancer.
Medical History
Your medical history can significantly influence your risk of developing anal cancer. Certain conditions or past diagnoses may increase your susceptibility. Understanding these connections can help you take proactive steps toward prevention.
History of cervical cancer or pre-cancer: Women who have had cervical cancer or pre-cancer face a higher risk of anal cancer. This link often stems from persistent HPV infections, which can affect multiple areas of the body.
Other cancers: A history of vaginal or vulvar cancer may also elevate your risk. These cancers share similar risk factors, such as HPV exposure, which can lead to cellular changes in the anal canal.
Tip: If you have been treated for any of these cancers, regular follow-ups with your doctor are essential. Early detection of abnormalities can improve outcomes.
Autoimmune diseases or chronic inflammatory conditions, such as Crohn's disease, may also play a role. These conditions weaken your immune system, making it harder for your body to fight infections like HPV. Treatments for these diseases, such as immunosuppressive drugs, can further increase your vulnerability.
Family history matters too. If close relatives have had anal cancer or related cancers, your genetic predisposition may put you at greater risk. Genetic counseling can help you understand your inherited risks and explore preventive measures.
By staying informed about your medical history and discussing it with your healthcare provider, you can better manage your risk. Regular screenings and lifestyle changes can make a significant difference in protecting your health.
When to Seek Medical Attention
Persistent Symptoms
Persistent symptoms often signal that something may be wrong. If you experience rectal bleeding, itching, or pain around the anus that does not improve, it is time to consult a healthcare provider. Changes in bowel habits, such as narrower stools or increased frequency, also require attention. Lumps or swelling near the anus, even if they resemble hemorrhoids, should not be ignored. These signs could indicate anal cancer or another serious condition.
Tip: Keep track of how long these symptoms last. If they persist for more than two weeks, schedule a medical evaluation.
Sudden or Severe Symptoms
Certain symptoms demand immediate medical attention due to their severity. Bleeding from the rectum, especially if it is heavy or accompanied by mucus discharge, should not be overlooked. Severe pain or pressure around the anus may also point to a more urgent issue. Swollen lymph nodes in the groin or anal area could suggest that the condition has progressed.
If you notice sudden changes in bowel movements, such as looser stools or difficulty passing stool, seek help promptly. These symptoms can escalate quickly and may require urgent care.
Family or Personal History
Your family and personal medical history play a crucial role in determining your risk. If you have a family history of anal cancer or related cancers, you may face a higher likelihood of developing the disease. Similarly, a personal history of conditions like cervical or vulvar cancer increases your risk.
Note: Share your medical history with your doctor during routine checkups. This information helps them assess your risk and recommend appropriate screenings.
By staying vigilant and seeking medical advice when necessary, you can catch potential issues early. Early detection improves treatment outcomes and can save lives.
Prevention of Anal Cancer
HPV Vaccination
Getting vaccinated against HPV is one of the most effective ways to prevent anal cancer. The vaccine works best when administered before exposure to the virus. Studies show that early vaccination can reduce the risk of persistent HPV infections by up to 90% in individuals who are seronegative for high-risk strains like HPV-16 and HPV-18.
Population-level data highlights the vaccine's impact. Since its introduction in 2008, the incidence of anal carcinoma in situ has decreased by 24%, while invasive anal cancer cases have dropped by 15% among individuals aged 20 to 44 years.
Evidence Type | Efficacy | Confidence Interval |
|---|---|---|
Persistent HPV Infection | 59% | 43.0%–71.4% |
AIN (any grade) | 50% | 25.7%–67.2% |
High-grade AIN | 54.2% | 18.0%–75.3% |
Tip: Talk to your doctor about the HPV vaccine, especially if you are under 45 years old. Early vaccination can protect you from HPV-related cancers, including anal cancer.
Lifestyle Changes
Your lifestyle choices play a significant role in reducing the risk of anal cancer. Quitting smoking is one of the most impactful changes you can make. Smoking weakens your immune system, making it harder to fight off HPV infections.
Other beneficial changes include:
Improving your diet by eating more fruits and vegetables.
Increasing physical activity to boost your overall health.
Practicing safe sex by using condoms to lower the risk of HPV transmission.
Note: Small, consistent changes in your daily habits can lead to long-term health benefits. Start by setting achievable goals, like reducing tobacco use or adding more greens to your meals.
Regular Medical Checkups
Regular screenings and medical checkups are essential for early detection of anal cancer, especially if you belong to a high-risk group. Screening methods like anal cytology (similar to a Pap smear) and high-resolution anoscopy (HRA) can identify precancerous lesions early.
Age/Condition | Recommendation |
|---|---|
35 years | MSM and TW with HIV infection should begin screening |
45 years | HIV+ patients (non-MSM/TW) and MSM and TW without HIV infection should begin screening |
10 years post-transplant | Solid organ transplant recipients should begin screening |
1 year post-diagnosis | History of vulvar pre-cancer or cancer should begin screening |
Callout: If you have a history of anal or genital warts, or if you belong to a high-risk group, schedule regular screenings. Early detection can save lives.
Understanding the symptoms, causes, and risk factors of anal cancer empowers you to take control of your health. Early detection significantly improves survival rates, with localized cases showing an 82% five-year survival rate compared to 35% for distant stages. Proactive measures, like HPV vaccination and regular screenings, can prevent cancer from developing. The ANCHOR trial highlights how early treatment of precancerous lesions reduces risks, especially for high-risk individuals. If you notice persistent symptoms or have a family history of cancer, consult your healthcare provider promptly. Taking action early can save lives.
FAQ
What is the survival rate for anal cancer?
The survival rate depends on the stage at diagnosis. Localized anal cancer has an 82% five-year survival rate. If the cancer spreads to distant areas, the rate drops to 35%. Early detection improves outcomes significantly.
Can anal cancer be prevented?
Yes, you can reduce your risk by getting the HPV vaccine, quitting smoking, and practicing safe sex. Regular screenings also help detect precancerous changes early, especially if you belong to a high-risk group.
Is anal cancer contagious?
No, anal cancer itself is not contagious. However, HPV, a major cause of anal cancer, spreads through skin-to-skin contact. Practicing safe sex and getting vaccinated can lower your risk of HPV infection.
How common is anal cancer?
Anal cancer is rare compared to other cancers. It accounts for less than 3% of all gastrointestinal cancers. However, its incidence has been rising, making awareness and prevention crucial.
What should I do if I notice symptoms?
If you experience symptoms like rectal bleeding, pain, or a lump near the anus, consult a healthcare provider immediately. Persistent symptoms lasting more than two weeks should never be ignored.
See Also
An In-Depth Overview of Various Cancer Types
Understanding Symptoms and Triggers of Acute Eosinophilic Leukemia

