What Are the Symptoms and Causes of Colon Cancer
Colon cancer affects millions of people worldwide and often begins with subtle signs. You might notice changes in bowel habits, such as thinner stools or irregular bowel movements. See also: Rectal Cancer Bright red blood in the toilet bowl or on toilet paper could indicate rectal bleeding, a common symptom. This condition has serious implications, as colorectal cancer is the third-leading cause of cancer-related deaths in men and the fourth in women in the U.S. Lifestyle choices, genetic predisposition, and certain medical conditions often contribute to its development. Early detection can save lives.
Key Takeaways
Look for early signs of colon cancer, like changes in bathroom habits or blood in poop. Finding it early can help a lot.
Eat healthy foods like fruits, veggies, and whole grains. This can lower your chance of getting colon cancer.
Get checked regularly starting at age 45. Tests like colonoscopies and stool checks can find problems early.
Know your family’s health history. If colon cancer runs in your family, think about genetic testing to check your risk.
Take care of long-term health problems and avoid bad habits like smoking or drinking too much alcohol. These can help keep you safer.
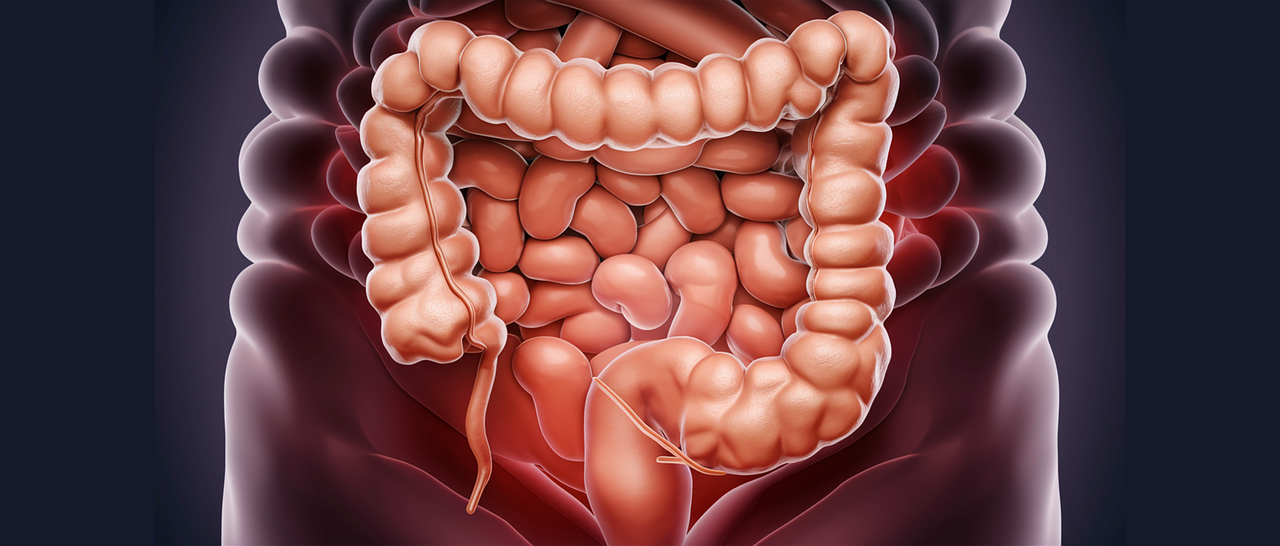
Symptoms of Colon Cancer
Common Symptoms
Changes in bowel habits
You might notice changes in your bowel habits as one of the first signs of colon cancer. These changes could include diarrhea, constipation, or stools that appear narrower than usual. These symptoms often persist for several days and may not improve with dietary adjustments.
Blood in stool or rectal bleeding
Blood in your stool or rectal bleeding is another common symptom. The blood may appear bright red or dark, depending on its source. While this can result from other conditions like hemorrhoids, it’s important to consult a healthcare provider if you notice this symptom.
Persistent abdominal discomfort
Persistent abdominal discomfort, such as cramps, bloating, or gas, can also indicate colon cancer. This discomfort may not go away and could worsen over time.
Early Warning Signs
Unexplained weight loss
Losing weight without trying is often an early warning sign. This happens because colon cancer can affect your body’s ability to absorb nutrients or increase your metabolism due to the disease.
Fatigue or weakness
Fatigue and weakness are common but often overlooked symptoms. These may result from anemia caused by intestinal bleeding, even if the bleeding isn’t visible.
Feeling of incomplete bowel emptying
You might feel like your bowel doesn’t completely empty after a movement. This sensation can occur even when there’s no stool left in the colon, signaling a potential blockage or tumor.
Note: Early symptoms like rectal bleeding, changes in bowel habits, and unexplained weight loss are often overlooked. Paying attention to these signs can lead to earlier detection and better outcomes.
Advanced Symptoms
Severe abdominal pain
As colon cancer progresses, you may experience severe abdominal pain. This pain often results from the tumor growing and pressing against nearby organs or tissues.
Colon obstruction
A tumor can block the colon, leading to symptoms like severe constipation, vomiting, and abdominal swelling. This condition requires immediate medical attention.
Jaundice (if cancer spreads to the liver)
If colon cancer spreads to your liver, you might develop jaundice. This condition causes yellowing of the skin and eyes and indicates advanced disease.
Early symptoms like blood in the stool and fatigue differ significantly from advanced symptoms such as colon obstruction and jaundice. Recognizing these differences can help you understand the progression of the disease.
Causes of Colon Cancer
Genetic Factors
Family history of colon cancer
Your family history plays a significant role in your risk of developing colon cancer. If close relatives, such as parents or siblings, have had colon cancer, your chances of developing the disease increase. This is because genetic mutations can be passed down, making you more susceptible.
Inherited syndromes like Lynch syndrome
Certain inherited syndromes, like Lynch syndrome, significantly raise your risk. Lynch syndrome, caused by mutations in genes such as MLH1 and MSH2, accounts for 2% to 4% of all colorectal cancers. Individuals with this syndrome face a lifetime risk of up to 50% for developing colon cancer. Other syndromes, like familial adenomatous polyposis (FAP), also contribute to higher risks due to mutations in the APC gene.
Tip: If you have a family history of Lynch syndrome or FAP, consider genetic testing to assess your risk.
Lifestyle Factors
Diet high in red or processed meats
Your diet can directly impact your colon health. Consuming large amounts of red or processed meats increases your risk of colon cancer. Studies show that red meat raises the risk by 30%, while processed meat increases it by 40%. This correlation becomes even stronger in older adults or individuals with obesity.
Meat Type | Increased Risk of Colorectal Cancer |
|---|---|
Red Meat | 30% |
Processed Meat | 40% |
Low fiber intake
A diet low in fiber can also contribute to colon cancer. Fiber helps maintain healthy digestion and supports the removal of waste from your colon. Without enough fiber, harmful substances may linger in your digestive tract, increasing your risk.
Sedentary lifestyle
A lack of physical activity can further elevate your risk. Regular exercise helps regulate your weight and improves digestion, reducing the likelihood of developing colon cancer.
Medical Conditions
Inflammatory bowel diseases
Chronic conditions like Crohn’s disease or ulcerative colitis can increase your risk of colon cancer. These diseases cause long-term inflammation in your colon, which may lead to abnormal cell growth.
Type 2 diabetes
If you have type 2 diabetes, your risk of colon cancer is higher. This connection may stem from shared risk factors like obesity and insulin resistance.
History of polyps
A history of colon polyps also raises your risk. Polyps are small growths in the colon that can become cancerous over time. Regular screenings can help detect and remove polyps before they develop into colon cancer.
Note: Managing chronic conditions and maintaining a healthy lifestyle can significantly reduce your risk of colon cancer.
Risk Factors for Colon Cancer
Non-Modifiable Risk Factors
Age (over 50)
Age plays a significant role in your risk of developing colon cancer. Most cases occur in individuals over 50, with the average diagnosis age being 68. As you age, your likelihood of developing this cancer increases. Men and African Americans face an even higher risk compared to other groups.
Family history of colon cancer
Your family history can significantly influence your risk. If close relatives, such as parents or siblings, have had colon cancer, your chances of developing it increase. This heightened risk often results from shared genetic mutations or environmental factors within families.
Genetic mutations
Inherited genetic mutations, like Lynch syndrome and familial adenomatous polyposis (FAP), can elevate your risk. These mutations disrupt normal cell growth, making you more susceptible to colon cancer. If you have a family history of these conditions, genetic testing can help assess your risk.
Tip: While you cannot change non-modifiable factors, understanding them can help you take preventive measures, like regular screenings.
Modifiable Risk Factors
Smoking and alcohol consumption
Smoking and high alcohol consumption are significant risk factors. Smoking, especially during early life, increases your risk. Alcohol, when consumed in large amounts, can also contribute, particularly if your diet lacks essential nutrients.
Obesity
Excess body weight is a consistent risk factor for colon cancer. Central deposition of fat, especially around your abdomen, further elevates this risk. Maintaining a healthy weight through diet and exercise can help reduce your chances of developing this disease.
Lack of physical activity
Physical inactivity can increase your risk. Regular exercise helps regulate your weight and improves digestion, both of which lower your chances of colon cancer. Even moderate physical activity, like walking, can make a difference.
Modifiable Risk Factors | Description |
|---|---|
Physical inactivity | Increases risk of colon cancer. |
Excess body weight | Consistent risk factor for colon cancer. |
High alcohol consumption | Likely increases risk, especially with low micronutrient diet. |
Environmental Factors
Limited access to screenings
Limited access to colon cancer screenings can delay diagnosis and treatment. Early detection through screenings like colonoscopies significantly improves outcomes. If you live in areas with fewer healthcare resources, you may face a higher risk due to delayed diagnosis.
Exposure to carcinogens
Exposure to carcinogens, such as those found in tobacco smoke or certain industrial chemicals, can increase your risk. These substances damage your DNA, leading to abnormal cell growth. Reducing exposure to these harmful agents can lower your chances of developing colon cancer.
Note: Modifiable and environmental factors offer opportunities for prevention. By making healthier lifestyle choices and advocating for better access to healthcare, you can reduce your risk.
Prevention Tips for Colon Cancer
Healthy Lifestyle Choices
Eat a diet rich in fruits and vegetables
Eating plenty of fruits, vegetables, and whole grains can lower your risk of colon cancer. These foods are high in fiber, which supports healthy digestion and helps remove waste from your body. A diet rich in plant-based foods also provides antioxidants and nutrients that protect your cells from damage.
Limit red and processed meats
Reducing your intake of red and processed meats is another effective way to prevent colon cancer. Studies show that diets high in these meats increase cancer risk. Instead, choose lean proteins like fish, poultry, or plant-based options such as beans and lentils.
Exercise regularly
Regular physical activity plays a key role in prevention. Exercise helps you maintain a healthy weight and improves digestion, both of which reduce your risk. Aim for at least 30 minutes of moderate activity, like walking or cycling, most days of the week.
Tip: Combining a healthy diet with regular exercise can significantly lower your risk of colon cancer.
Regular Screenings
Colonoscopy starting at age 45
A colonoscopy is one of the most effective screening tools. It allows doctors to detect and remove polyps before they become cancerous. Experts recommend starting screenings at age 45 and repeating them every 10 years if results are normal.
Stool-based tests
Stool-based tests, such as the fecal immunochemical test (FIT) or stool DNA tests, are non-invasive options. These tests can detect blood or abnormal DNA in your stool, which may indicate colon cancer. FIT should be done annually, while stool DNA tests are recommended every three years.
Test Type | Frequency |
|---|---|
FIT | Every year |
Stool DNA test | Every 3 years |
Colonoscopy | Every 10 years |
Genetic testing for high-risk individuals
If you have a family history of colon cancer or inherited syndromes like Lynch syndrome, genetic testing can help assess your risk. Early detection through genetic testing allows you to take preventive measures, such as more frequent screenings.
Avoid Risky Behaviors
Quit smoking
Smoking increases your risk of colon cancer by exposing your body to harmful carcinogens. Quitting smoking not only lowers this risk but also improves your overall health.
Limit alcohol consumption
Drinking alcohol in moderation or avoiding it altogether can reduce your risk. Alcohol consumption, especially in large amounts, has been linked to a higher likelihood of developing colon cancer.
Manage chronic conditions
Managing chronic conditions like type 2 diabetes or inflammatory bowel diseases is essential. Proper treatment and regular check-ups can help reduce inflammation and prevent abnormal cell growth in your colon.
Note: Small changes, like quitting smoking or limiting alcohol, can make a big difference in reducing your risk.
Colon cancer is a preventable and treatable disease when detected early. Recognizing symptoms like changes in bowel habits or blood in stool can lead to timely diagnosis. Early detection significantly improves survival rates, with Stage 0 and Stage 1 having a 91% survival rate compared to just 13% for Stage 4.
Colon cancer stage at diagnosis | Survival rate |
|---|---|
Stage 0 and Stage 1 | 91% |
Stage 2 and Stage 3 | 73% |
Stage 4 | 13% |
Overall | 63% |
Understanding the causes and risk factors empowers you to take preventive steps. Recent advancements, such as targeted therapy drugs, have improved treatment outcomes. Adopting a healthy lifestyle and undergoing regular screenings remain the most effective ways to reduce your risk.
Tip: Stay proactive about your health by scheduling regular screenings and maintaining a balanced diet.
FAQ
What are the early symptoms of colon cancer?
Early symptoms include changes in bowel habits, blood in your stool, and unexplained weight loss. You might also feel fatigued or experience abdominal discomfort. These signs often appear subtle, so paying attention to your body is crucial.
Tip: If you notice these symptoms, consult a healthcare provider promptly.
How often should you get screened for colon cancer?
Doctors recommend starting colon cancer screenings at age 45. A colonoscopy is typically done every 10 years if results are normal. Stool-based tests, like FIT, should be done annually.
Note: High-risk individuals may need more frequent screenings.
Can diet affect your risk of colon cancer?
Yes, your diet plays a significant role. Eating red or processed meats increases your risk. A diet rich in fruits, vegetables, and fiber can help lower it.
Foods to Avoid: Processed meats, red meats
Foods to Include: Whole grains, leafy greens, beans
Is colon cancer hereditary?
Colon cancer can run in families. Genetic mutations, like Lynch syndrome or FAP, increase your risk. If you have a family history, genetic testing and early screenings can help you stay proactive.
Can colon cancer be prevented?
You can reduce your risk by maintaining a healthy lifestyle. Eat a balanced diet, exercise regularly, and avoid smoking or excessive alcohol. Regular screenings also play a key role in prevention.
Reminder: Prevention starts with small, consistent changes in your daily habits.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Exploring Breast Cancer: Symptoms and Underlying Causes
Bladder Cancer: Identifying Symptoms and Their Causes
Anal Cancer: Key Symptoms and Contributing Factors

