Understanding Symptoms and Treatments for Adrenocortical Adenoma
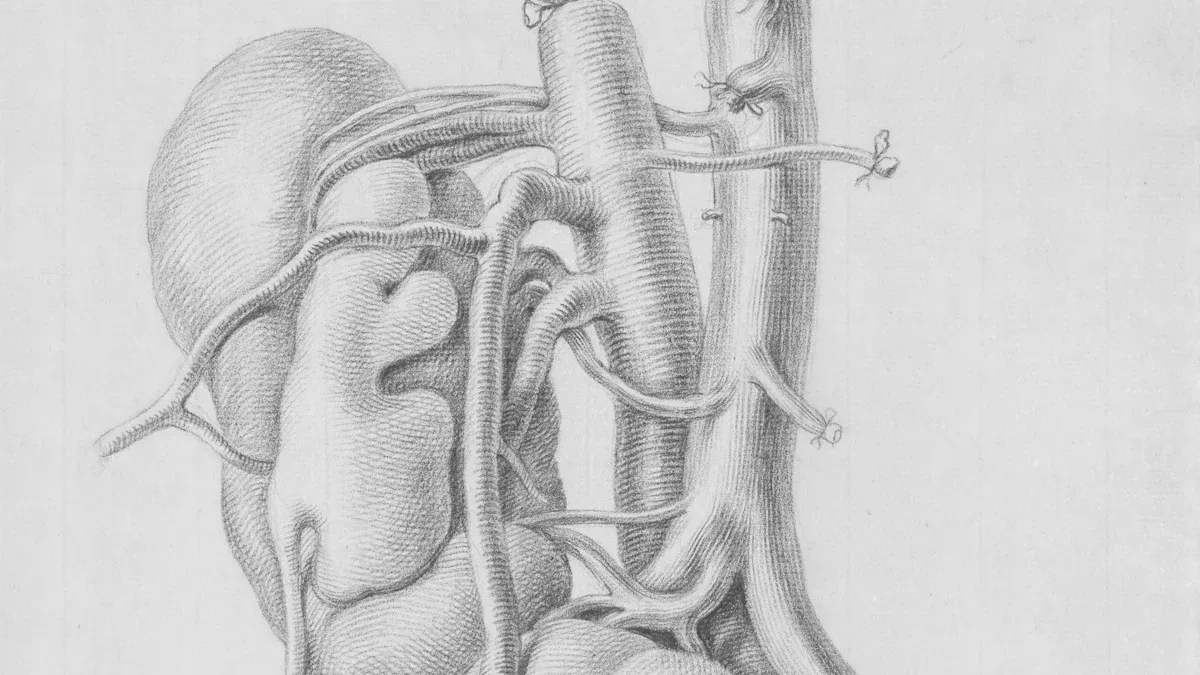
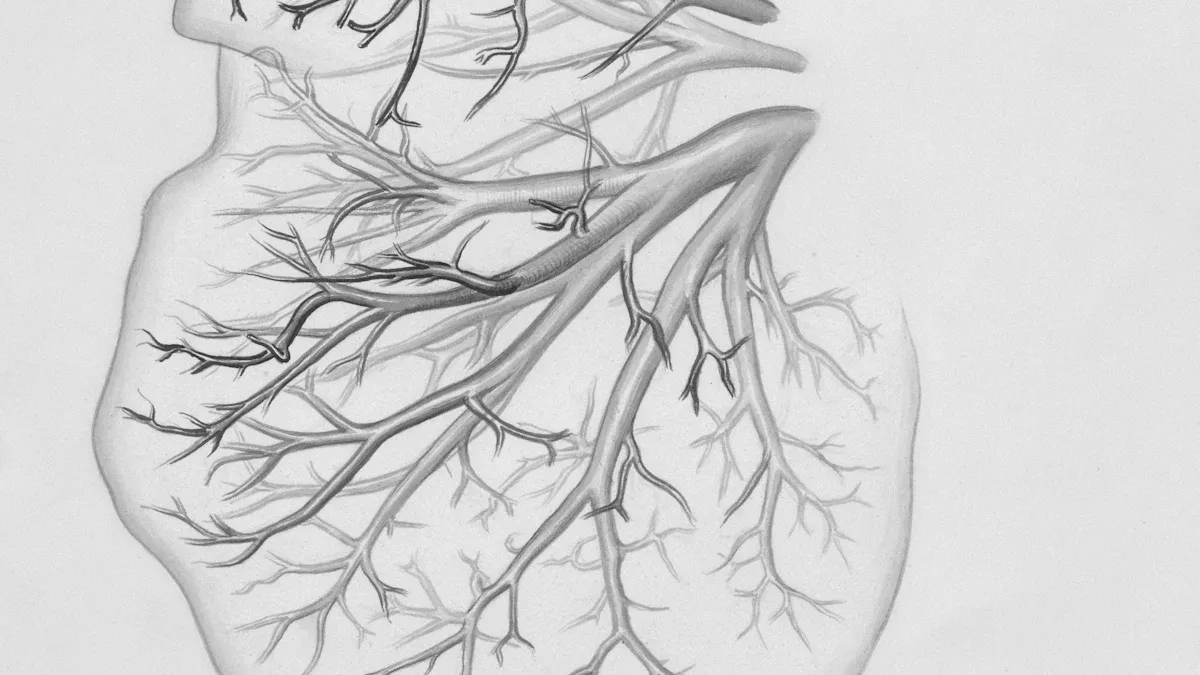
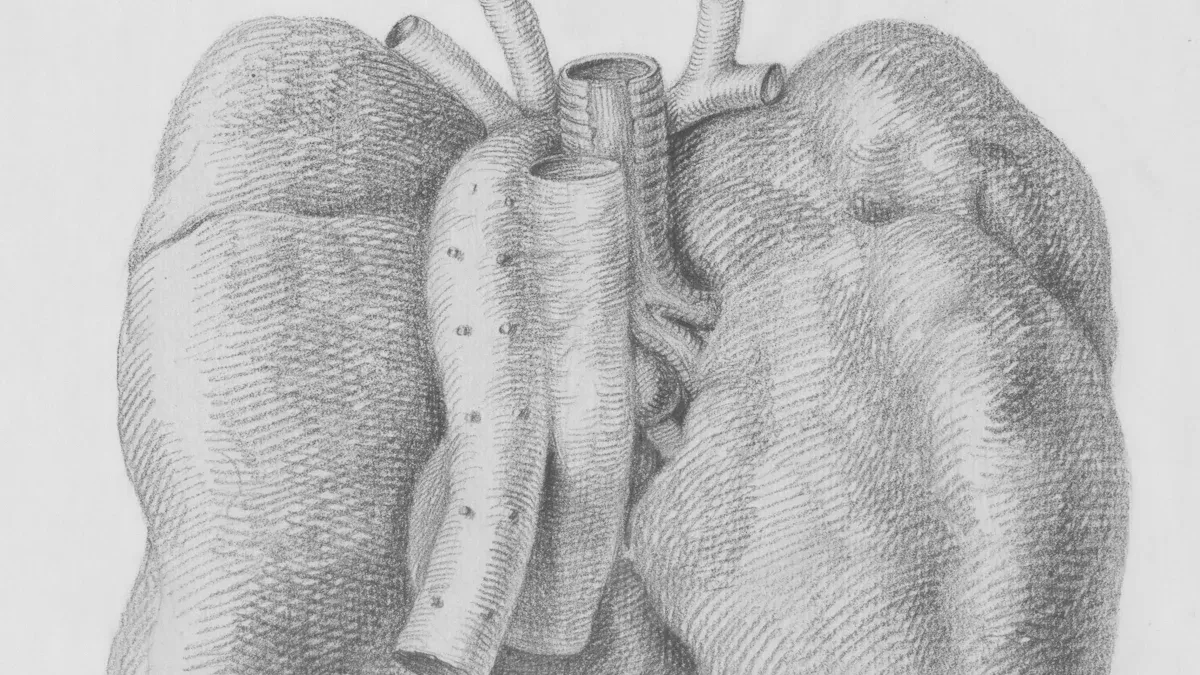
Adrenocortical adenoma is a non-cancerous tumor that develops in your adrenal glands. These glands, located above your kidneys, produce hormones that regulate vital functions like blood pressure, metabolism, and stress response. When this tumor disrupts hormone production, you may experience noticeable symptoms.
Here are some common symptoms associated with this condition:
Symptom | Description |
|---|---|
Fatigue and achiness | General tiredness and discomfort |
High blood pressure | Elevated blood pressure levels (hypertension) |
High blood sugar levels | Increased blood sugar or diabetes |
Low potassium levels | Decreased potassium in the blood |
Stretch marks on abdomen | Skin changes due to hormonal effects |
Weight gain | Particularly in the upper body |
Mood changes | Anxiety, panic, or depression |
Irregular menstrual cycles | Specific to females |
Increased masculine characteristics | Virilization in females |
Sexual dysfunction | Specific to males |
Treatment depends on the tumor's size and activity. Options include regular monitoring, medications to manage hormone levels, or surgery to remove the tumor. Early diagnosis plays a crucial role in preventing complications and improving your quality of life.
Key Takeaways
Adrenocortical adenoma is a harmless growth in the adrenal glands. It can mess up hormones, causing tiredness, high blood pressure, and weight gain.
Symptoms depend on the type of tumor. Working tumors make extra hormones, leading to more obvious problems.
Doctors check your health history, do exams, and use CT scans to find the tumor.
Treatments include watching small tumors, taking medicine for symptoms, or surgery for big or hormone-making tumors.
Regular check-ups are important to spot changes and stay healthy.
What Is Adrenocortical Adenoma?
Definition
Adrenocortical adenoma refers to a benign tumor that forms in your adrenal glands, which sit above your kidneys. These glands play a vital role in producing hormones that regulate stress, metabolism, and blood pressure. While some of these tumors remain inactive and cause no symptoms, others can produce excess hormones, leading to noticeable health issues. The symptoms you experience depend on whether the tumor is functional or non-functional.
Types
Adrenocortical adenomas are classified into two main types based on their activity:
Functioning Adenomas
Functioning adenomas actively produce hormones, which can disrupt your body's natural balance. These tumors may lead to conditions like Cushing’s syndrome, Conn’s syndrome, or hormonal imbalances involving androgens or estrogens. For example, if the tumor produces too much cortisol, you might notice symptoms such as weight gain, high blood pressure, or muscle weakness. Hormonal overproduction often requires medical intervention to manage the effects.
Nonfunctioning Adenomas
Nonfunctioning adenomas do not produce hormones and are often discovered incidentally during imaging tests for unrelated issues. These tumors typically remain small and harmless, causing no symptoms. In most cases, doctors recommend monitoring them over time to ensure they do not grow or become problematic.
Note: Understanding the type of adrenocortical adenoma you have is crucial for determining the best treatment approach. Functional tumors often require more immediate attention, while nonfunctional ones may only need regular observation.
Symptoms of Adrenocortical Adenoma
Adrenocortical adenoma can cause a variety of symptoms, depending on whether the tumor produces excess hormones. These symptoms fall into two main categories: hormonal and general.
Hormonal Symptoms
Cortisol Overproduction (Cushing’s Syndrome)
When your tumor produces too much cortisol, you may develop Cushing’s syndrome. This condition often leads to weight gain, particularly in the upper body, and visible stretch marks on your abdomen. You might also notice high blood pressure, muscle weakness, and elevated blood sugar levels. These changes can make daily activities more challenging.
Aldosterone Overproduction (Conn’s Syndrome)
Excess aldosterone production can result in Conn’s syndrome. This condition causes high blood pressure and low potassium levels, which may lead to muscle cramps or weakness. If you experience these symptoms, it’s important to seek medical advice, as untreated Conn’s syndrome can increase the risk of heart and kidney problems.
Androgen or Estrogen Overproduction
Some tumors produce excess androgens or estrogens, leading to hormonal imbalances. Women may notice irregular menstrual cycles or increased masculine characteristics, such as facial hair growth. Men might experience sexual dysfunction or other changes in their reproductive health.
General Symptoms
Fatigue and Muscle Weakness
Feeling tired and weak is a common complaint among individuals with adrenocortical adenoma. These symptoms can occur due to hormonal imbalances or the physical strain caused by the tumor.
High Blood Pressure and Weight Gain
High blood pressure is one of the most frequently reported symptoms. Weight gain, especially in the upper body, is another common issue. These changes often result from hormonal overproduction.
Mood Changes and Other Effects
Hormonal fluctuations can affect your mood, leading to anxiety, depression, or irritability. You might also notice changes in your skin, such as stretch marks, or experience other physical effects like low potassium levels.
Tip: If you experience any of these symptoms, consult a healthcare provider. Early diagnosis of adrenocortical adenoma can help prevent complications and improve your quality of life.
Diagnosing Adrenocortical Adenoma
Medical History and Physical Examination
Diagnosing adrenocortical adenoma begins with a thorough review of your medical history and a physical examination. Your doctor will ask about symptoms like fatigue, high blood pressure, or weight gain. They may also inquire about your family history of adrenal or other cancers. If you are female, they might assess menstrual irregularities or signs of increased masculine traits. For males, they may evaluate sexual dysfunction or other hormonal symptoms.
During the physical exam, your doctor will check your abdomen for any noticeable masses or tumors. Blood and urine tests often follow to detect abnormal hormone levels, which can indicate whether the tumor is functional.
Tip: Keep a record of your symptoms and family medical history. Sharing this information with your doctor can help speed up the diagnostic process.
Imaging Tests
Imaging tests play a crucial role in confirming the presence of an adrenocortical adenoma. These tests provide detailed images of your adrenal glands and help determine the tumor's size, shape, and activity.
Imaging Technique | Description |
|---|---|
CT | The preferred method for identifying adenomas. It shows well-defined mass lesions with specific patterns of enhancement. |
MRI | Useful for further evaluation, though it struggles to characterize lipid-poor adenomas. It requires more complex calculations compared to CT. |
PET | Helps differentiate benign adenomas from malignant tumors. Malignant tumors show increased uptake of specific tracers. |
Your doctor will likely recommend a CT scan first, as it is the most effective tool for diagnosing this condition.
Hormonal Testing
Hormonal tests are essential for determining whether your tumor is functioning or non-functioning. These tests analyze blood or urine samples to measure hormone levels. Excess cortisol may point to Cushing’s syndrome, while elevated aldosterone levels could indicate Conn’s syndrome.
One common test is the Dexamethasone Suppression Test. In this test, you take a dose of dexamethasone, and your cortisol levels are measured afterward. If cortisol remains high, it suggests a functioning tumor.
Note: Hormonal testing helps pinpoint the exact cause of your symptoms, guiding your doctor toward the most effective treatment plan.
Biopsy (When Necessary)
A biopsy is not always the first step in diagnosing adrenocortical adenoma. However, it becomes necessary in specific situations. If imaging tests and hormonal evaluations fail to determine whether a tumor is benign or malignant, your doctor may recommend a biopsy. This procedure helps clarify the nature of the tumor, especially when there is suspicion of cancer.
The most common type of biopsy for adrenal tumors is fine-needle aspiration. During this procedure, a thin needle extracts a small tissue sample from the tumor. A pathologist then examines the sample under a microscope to identify any abnormal or cancerous cells. This process provides critical information that other tests might not reveal.
Tip: A biopsy is typically reserved for cases where the tumor's behavior remains unclear. It is not routinely performed for all adrenal adenomas.
Although a biopsy is a valuable diagnostic tool, it is not without risks. The adrenal glands are located near major blood vessels and other vital structures. This makes the procedure slightly more complex than biopsies in other areas. Your doctor will carefully evaluate the risks and benefits before recommending it.
If your doctor suggests a biopsy, you should feel free to ask questions. Understanding why it is necessary and how it will be performed can help ease any concerns. This step ensures that you receive the most accurate diagnosis and appropriate treatment plan for your condition.
Treatment Options for Adrenocortical Adenoma
Monitoring and Observation
If your adrenocortical adenoma is small and nonfunctioning, your doctor may recommend regular monitoring instead of immediate treatment. This approach involves periodic imaging tests, such as CT scans or MRIs, to track the tumor's size and ensure it remains stable. Hormonal testing may also be part of the follow-up to confirm that the tumor is not producing excess hormones. Monitoring allows you to avoid unnecessary treatments while keeping a close watch on any changes in the tumor's behavior.
Tip: Stick to your follow-up schedule. Early detection of changes can help prevent complications.
Medications
Medications can help manage symptoms caused by hormone-producing tumors. These drugs work by either blocking hormone production or reducing its effects on your body. Commonly prescribed medications include:
Metyrapone: This drug reduces cortisol production. It is often used when surgery is not an option or to control symptoms before surgery. You may notice improvements within weeks.
Mitotane: This medication destroys adrenal cortex cells and lowers hormone levels. While primarily used for adrenal cortical carcinoma, it can also help in advanced cases of adrenal adenomas. However, it may take several months to see its full effect.
Spironolactone: This diuretic blocks aldosterone action and is commonly prescribed for Conn’s syndrome. It can improve symptoms like high blood pressure and low potassium levels within days to weeks.
Your doctor will choose the medication based on your specific symptoms and the type of hormones your tumor produces.
Surgery
Surgery is often the best option for treating functioning tumors or larger nonfunctioning tumors. Removing the tumor can restore hormonal balance and prevent further complications.
Laparoscopic Adrenalectomy
Laparoscopic adrenalectomy is a minimally invasive procedure. Surgeons use small incisions and a camera to remove the tumor. This method offers a quicker recovery time and less postoperative pain compared to open surgery. It is typically recommended for smaller tumors.
Open Surgery (For Larger Tumors)
Open surgery may be necessary if your tumor is large or suspected to be malignant. This procedure involves a larger incision to provide better access to the adrenal gland. While recovery takes longer, it ensures complete removal of the tumor and surrounding tissues if needed.
Note: Your surgeon will decide the best approach based on the tumor's size, location, and activity.
Post-Treatment Care
After treatment for adrenocortical adenoma, taking care of yourself becomes essential for recovery and long-term health. Your body needs time to adjust, especially if you underwent surgery or started hormone therapy. Following your doctor’s advice ensures a smoother recovery process.
Steps to Follow After Treatment
Attend Follow-Up Appointments: Regular check-ups help your doctor monitor your progress. These visits often include imaging tests or blood work to ensure the tumor hasn’t returned and your hormone levels remain stable.
Take Prescribed Medications: If your treatment involved hormone-blocking drugs or replacement therapy, take them exactly as directed. Skipping doses can disrupt your recovery.
Adopt a Healthy Lifestyle: Eating a balanced diet, staying active, and managing stress can improve your overall well-being. These habits also support your adrenal glands as they recover.
Watch for Symptoms: Pay attention to any unusual changes, such as fatigue, weight gain, or mood swings. Report these to your healthcare provider immediately.
Tip: Keep a journal of your symptoms and progress. This can help you track improvements and share detailed information with your doctor during follow-ups.
Why Post-Treatment Care Matters
Post-treatment care helps prevent complications and ensures your adrenal glands function properly. If you had surgery, your remaining adrenal gland may need time to compensate for the loss. Hormonal imbalances can take weeks or months to stabilize. Staying proactive with your care reduces the risk of long-term issues.
Recovery is a journey. By following these steps, you can regain your health and maintain a better quality of life. Always communicate openly with your healthcare team to address concerns and adjust your care plan as needed.
Can Adrenocortical Adenoma Become Cancerous?
Risk Factors for Malignancy
Although most adrenocortical adenomas are benign, certain factors can increase the risk of malignancy. Genetic conditions play a significant role. These include Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, multiple endocrine neoplasia (MEN1), familial adenomatous polyposis (FAP), and Lynch syndrome. If you have any of these conditions, your risk of developing adrenocortical carcinoma may be higher.
Lifestyle factors also contribute to the risk. Being overweight, smoking, or leading a sedentary lifestyle can increase the likelihood of complications. While these factors do not guarantee malignancy, they can influence the overall health of your adrenal glands. Maintaining a healthy lifestyle can help reduce these risks.
Tip: If you have a family history of genetic conditions or notice any unusual symptoms, consult your doctor for regular screenings.
Signs of Adrenocortical Carcinoma
Adrenocortical carcinoma, though rare, presents specific warning signs. You might experience abdominal pain, a feeling of fullness, or difficulty eating due to early satiety. Hormonal changes can also occur, leading to weight gain or loss, muscle weakness, or trouble sleeping. Women may notice deepening of the voice or increased facial hair growth.
Other symptoms include high blood pressure, easy bruising, and mood changes. Children with this condition may show signs of early puberty. If you experience persistent back or side pain, appetite changes, or fluid retention, these could also indicate a problem.
Note: These symptoms overlap with other conditions, so it’s essential to seek medical advice for an accurate diagnosis.
Importance of Regular Monitoring
Regular monitoring is crucial for managing adrenocortical adenomas. Research shows that only about 14% of adrenal masses are cancerous. Benign adenomas rarely become malignant, but consistent follow-ups help detect changes early. Imaging tests and hormonal evaluations can track the tumor’s behavior over time.
By staying proactive, you can address potential issues before they escalate. Early detection improves treatment outcomes and helps maintain your overall health.
Tip: Schedule routine check-ups and share any new symptoms with your healthcare provider promptly.
Adrenocortical adenoma is a manageable condition when addressed early. You have access to various treatment options, including monitoring, medications, or surgery, depending on your specific needs. Early detection helps you avoid complications and maintain a better quality of life. If you notice symptoms like fatigue, high blood pressure, or hormonal changes, consult a healthcare provider. Taking action ensures you receive the care you need to protect your adrenal health.
FAQ
What causes adrenocortical adenoma?
Adrenocortical adenomas form due to genetic mutations in adrenal gland cells. These mutations cause abnormal cell growth. Some cases link to inherited conditions like Li-Fraumeni syndrome. Lifestyle factors, such as obesity or smoking, may also contribute.
How is adrenocortical adenoma different from adrenal cancer?
Adrenocortical adenoma is a benign tumor, meaning it doesn’t spread to other parts of your body. Adrenal cancer, or adrenocortical carcinoma, is malignant and can invade nearby tissues. Regular monitoring helps distinguish between the two.
Can adrenocortical adenoma go away on its own?
No, adrenocortical adenomas don’t disappear without treatment. Nonfunctioning adenomas may remain stable and require only monitoring. Functioning adenomas, which produce excess hormones, often need medications or surgery to manage symptoms.
Is surgery always necessary for adrenocortical adenoma?
No, surgery isn’t always required. Small, nonfunctioning adenomas often only need observation. Surgery becomes necessary if the tumor produces hormones, grows larger, or shows signs of malignancy. Your doctor will recommend the best approach.
Can lifestyle changes help manage adrenocortical adenoma?
Lifestyle changes can support overall health but won’t shrink the tumor. Eating a balanced diet, exercising, and managing stress can improve symptoms like high blood pressure. These habits also reduce risks associated with hormonal imbalances.
Tip: Always follow your doctor’s advice for managing this condition effectively.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
