Choroid Plexus Carcinoma-Understanding Symptoms and Treatments
Choroid plexus carcinoma is a rare and aggressive type of brain cancer. It develops in the choroid plexus, the part of your brain responsible for producing cerebrospinal fluid. This tumor affects only about 0.010 people per 100,000 person-years, making it one of the least common brain cancers. For comparison, choroid plexus papilloma occurs at a higher rate of 0.034 per 100,000 person-years, while atypical choroid plexus papilloma is even rarer at 0.005.
Recognizing symptoms early plays a critical role in improving outcomes. Timely detection allows doctors to begin treatment sooner, which can enhance your prognosis. A multidisciplinary approach, involving specialists from different fields, ensures comprehensive care and better management of this challenging condition.
Key Takeaways
Look for early signs like constant headaches, nausea, or blurry vision. Finding the cancer early can make treatments work better.
See a doctor quickly if you notice these symptoms. Tests like scans and biopsies are important to start the right treatment.
Surgery is the main way to treat this cancer. Removing the whole tumor can help you live longer, so talk to your doctor about surgery options.
Learn about new treatments like immunotherapy and targeted medicine. These may work better and cause fewer problems than older treatments.
Use support services like care for comfort and survivor groups. These can help you and your family handle the challenges of this illness.
Symptoms of Choroid Plexus Carcinoma

Common Symptoms
Choroid plexus carcinoma often presents with symptoms that can mimic other conditions. You might notice persistent headaches that worsen over time. Nausea and vomiting, especially in the morning, are also common. Many patients experience extreme fatigue or drowsiness, making it difficult to stay alert during the day. Vision problems, such as blurred or double vision, may occur as the tumor grows. Some individuals report irritability or mood changes, which can be mistaken for stress or other emotional issues. Seizures and weakness in certain parts of the body are additional signs that should not be ignored.
Severe Symptoms
As the tumor progresses, symptoms can become more severe. You may experience meningitis-like symptoms, including a stiff neck and sensitivity to light. Difficulty moving one side of the body or sudden numbness can indicate advanced disease. Seizures may become more frequent or intense. In some cases, the pressure inside the skull increases significantly, leading to confusion, dizziness, or even loss of consciousness. These severe symptoms require immediate medical attention.
Symptoms in Children vs. Adults
Choroid plexus carcinoma affects children and adults differently. In children, symptoms often include irritability, fussiness, and difficulty feeding. Young children may also show developmental delays or regressions. For adults, headaches, nausea, and vision problems are more prominent. Adults might also experience mood disturbances or dizziness. Regardless of age, recognizing these symptoms early can make a significant difference in treatment outcomes.
Causes and Risk Factors
Genetic Mutations
Genetic mutations play a significant role in the development of choroid plexus carcinoma. One of the most common mutations associated with this cancer involves the TP53 gene. This gene is crucial for regulating cell growth and preventing tumors. When it mutates, cells can grow uncontrollably, leading to cancer. Individuals with Li-Fraumeni syndrome, a rare inherited condition, often carry a germline mutation in the TP53 gene. This syndrome increases the likelihood of developing various cancers, including choroid plexus carcinoma.
If you or a loved one has been diagnosed with this condition, genetic testing can provide valuable insights. Testing for TP53 mutations helps doctors understand the genetic basis of the tumor. It also aids in predicting outcomes. Research shows that children with two copies of the mutated TP53 gene in their tumors face a poorer prognosis. This highlights the importance of early detection and tailored treatment plans.
Age and Family History
Age and family history can influence your risk of developing choroid plexus carcinoma. This cancer is more common in children under the age of five. However, it can also occur in adults, though less frequently. While choroid plexus carcinoma itself is not inherited, certain genetic conditions, like Li-Fraumeni syndrome, can increase your risk.
If you have a family history of Li-Fraumeni syndrome, you may be more prone to developing cancers, including this rare brain tumor. However, it’s important to note that choroid plexus carcinoma arises from unknown gene mutations in most cases. This means that having a family history of the condition does not directly increase your risk. Understanding these factors can help you take proactive steps, such as discussing genetic testing with your healthcare provider.
Diagnosis of Choroid Plexus Carcinoma
Physical and Neurological Exams
Diagnosing choroid plexus carcinoma begins with a thorough evaluation of your symptoms and overall neurological health. Doctors use several methods to assess brain and nerve function:
A health history and physical exam help identify symptoms, risk factors, and general health concerns.
Tests for vision, hearing, and memory provide additional insights into brain function.
A spinal tap (lumbar puncture) may be performed to analyze cerebrospinal fluid for cancer cells.
These exams provide critical information about how the tumor affects your brain and nervous system. They also guide the next steps in the diagnostic process.
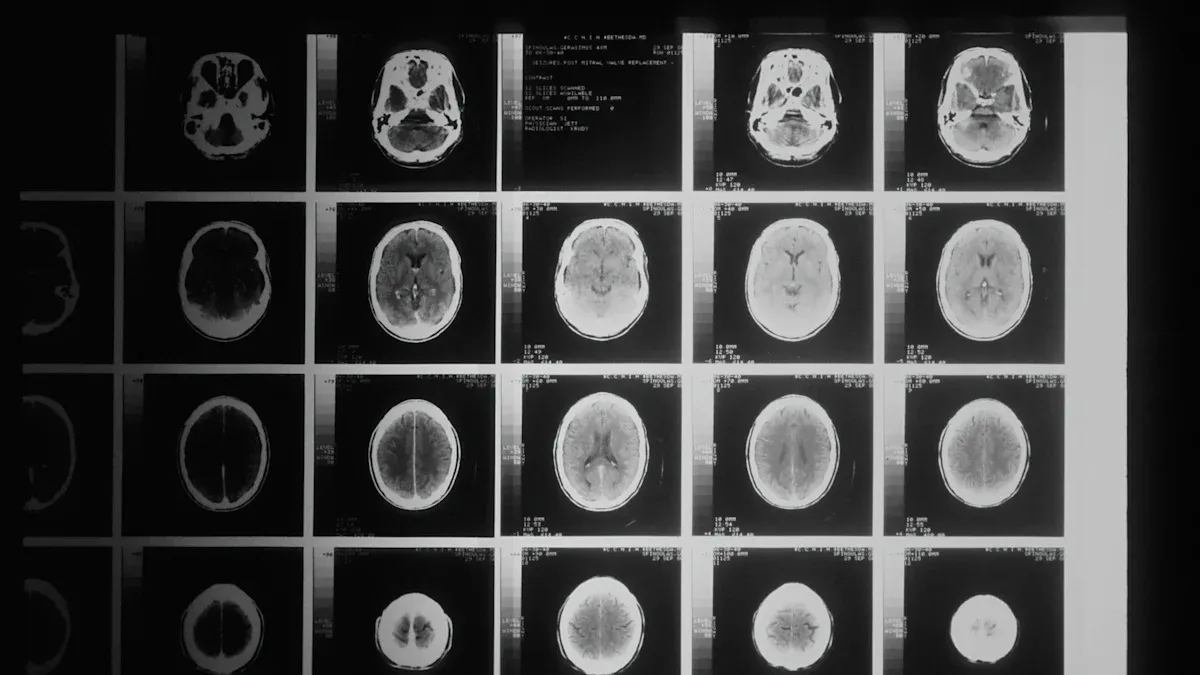
Imaging Tests
Imaging tests play a key role in identifying choroid plexus carcinoma. Doctors often rely on MRI and CT scans to visualize the tumor and its characteristics.
Imaging Test | Characteristics | Findings |
|---|---|---|
MRI | Preferred diagnostic tool; provides detailed, multiplanar images | Reveals well-defined, frondlike intraventricular masses; hypointense on T1-weighted images; hyperintense on T2-weighted images; shows active blood flow and vascularity |
CT | Secondary option; less detailed than MRI | Detects increased intracranial pressure; may show faint calcifications in some cases |
MRI is the test of choice due to its ability to eliminate artifacts and provide clearer images of the tumor's size and location.
Biopsy and Laboratory Analysis
A biopsy is essential for confirming the diagnosis of choroid plexus carcinoma. During this procedure, surgeons remove a small tissue sample from the tumor. Laboratory specialists then examine the sample under a microscope to identify cancer cells. This analysis provides detailed information about the tumor's type and grade, helping doctors develop an effective treatment plan.
Recent advancements in diagnostic tools, such as molecular markers and liquid biopsy, are improving accuracy. These methods allow doctors to analyze genetic material from the tumor or body fluids, offering insights into potential treatment targets and monitoring progress over time.
Treatment Options for Choroid Plexus Carcinoma
Surgery
Surgery is the cornerstone of treatment for choroid plexus carcinoma. Doctors aim to remove as much of the tumor as possible, as complete removal significantly improves survival rates. Patients who undergo gross total resection (GTR) have an 84% survival rate, compared to just 18% for those with subtotal resection (STR).
Surgical Outcome | Survival Rate (%) |
|---|---|
Gross Total Resection | 84 |
Subtotal Resection | 18 |
If the tumor cannot be fully removed, additional therapies like chemotherapy or radiation may be necessary. Surgery also helps alleviate symptoms caused by increased intracranial pressure, such as headaches and nausea. Your medical team will carefully evaluate the tumor's location and your overall health to determine the best surgical approach.
Radiation Therapy
Radiation therapy can improve survival rates, especially for older patients. It targets and destroys remaining cancer cells after surgery. However, this treatment carries risks, particularly for young children. High doses of radiation can harm the developing brain, potentially causing long-term side effects like learning disabilities or an increased risk of secondary cancers.
For this reason, doctors often avoid radiation therapy in younger children unless absolutely necessary. In older patients, the benefits often outweigh the risks. Your healthcare provider will weigh these factors to create a personalized treatment plan.
Chemotherapy
Chemotherapy is another critical component of treatment, particularly when surgery cannot completely remove the tumor. Aggressive chemotherapy regimens, such as the ICE protocol (ifosfamide, carboplatin, and etoposide), have shown promise in improving outcomes. This approach is especially effective in young children and may be used before a second surgery to shrink the tumor.
Chemotherapy can be combined with radiation therapy to enhance effectiveness.
High-dose chemotherapy with stem cell transplants is sometimes recommended for advanced cases.
Common side effects include fatigue, nausea, and long-term risks like hearing loss or fertility issues.
Your medical team will tailor the chemotherapy plan to your specific needs, balancing effectiveness with potential side effects.
Emerging Therapies
Emerging therapies offer new hope for treating choroid plexus carcinoma. Researchers are exploring innovative approaches that aim to improve outcomes and reduce side effects. These therapies focus on targeting cancer cells more precisely while sparing healthy tissue.
One promising area involves immunotherapy. This treatment boosts your immune system's ability to recognize and attack cancer cells. For example, immune checkpoint inhibitors help your body overcome the defenses that tumors use to evade detection. Although still in experimental stages for this cancer, immunotherapy has shown success in other types of brain tumors.
Targeted therapy is another exciting development. Unlike traditional chemotherapy, targeted drugs focus on specific molecules or pathways that cancer cells rely on to grow. Scientists are studying drugs that inhibit proteins linked to tumor growth in choroid plexus carcinoma. This approach may lead to fewer side effects compared to conventional treatments.
Note: Clinical trials play a crucial role in advancing these therapies. Participating in a trial gives you access to cutting-edge treatments while contributing to medical research.
Gene therapy is also gaining attention. This method involves altering the genetic material within cancer cells to stop their growth. Researchers are investigating how to deliver these therapies safely and effectively.
These emerging treatments represent a shift toward personalized medicine. By tailoring therapies to your tumor's unique characteristics, doctors can offer more effective and less invasive options. Discuss these advancements with your healthcare team to understand if they might benefit you.
Recovery and Prognosis
Post-Treatment Recovery
Recovering from choroid plexus carcinoma treatment involves several factors that influence the timeline and challenges you may face. These include your age, overall health, and the location and number of tumors. Follow-up treatments, such as chemotherapy or radiation, also play a significant role in your recovery process.
You may need frequent brain imaging tests to monitor your healing and detect any signs of recurrence. These tests help your medical team adjust your care plan as needed. Recovery can be physically and emotionally demanding, especially if you experience side effects like fatigue or cognitive changes.
Here are some common challenges patients face during recovery:
Managing side effects from chemotherapy or radiation.
Regaining strength and mobility after surgery.
Coping with emotional stress or anxiety about recurrence.
Your healthcare team will guide you through this process, offering support and resources to help you regain your quality of life.
Survival Rates and Long-Term Outcomes
Survival rates for choroid plexus carcinoma vary based on several factors. The average 5-year overall survival rate is 61.3%. However, your prognosis depends on your age, the extent of tumor removal, and whether the cancer has spread.
Factor | Description |
|---|---|
Age | |
Tumor Removal | Complete removal improves chances of survival. |
Tumor Spread | Cancer spreading to other areas decreases survival chances. |
Genetic Mutations | TP53 mutations correlate with decreased survival. |
Treatment Methods | Radiation effects vary based on age and genetics. |
Survival rates also differ by age group:
Age Group | Survival Rate |
|---|---|
Under 4 years | Poorer prognosis |
Older children | Better prognosis |
Overall chance | 50-70% |
While these statistics provide a general outlook, every case is unique. Advances in treatment, such as targeted therapies, continue to improve outcomes. Staying proactive with follow-up care and maintaining a healthy lifestyle can positively impact your long-term recovery.
Understanding choroid plexus carcinoma begins with recognizing its symptoms, such as persistent headaches, nausea, and vision problems. Early diagnosis through imaging tests and biopsies ensures timely treatment, which may include surgery, chemotherapy, or radiation therapy. Emerging therapies like immunotherapy and targeted treatments offer new hope for improving outcomes.
Early detection remains critical. Consulting healthcare professionals promptly can make a significant difference. They provide essential services, such as palliative care, psycho-oncology, and caregiver resources, to support you and your family.
Description | |
|---|---|
Palliative Care | Provides relief from symptoms and stress. |
Survivor Peer Support | Connects patients with others who have survived. |
Nutrition Counseling | Offers dietary guidance to improve health. |
Psycho-oncology | Addresses emotional and psychological needs. |
Caregiver Resources | Provides information and support for caregivers. |
Support Groups | Facilitates sharing experiences among families. |
You are not alone in this journey. Resources like survivorship programs, caregiver support, and educational webinars can help you navigate the challenges. Stay informed, ask questions, and lean on your support network to face this condition with strength and hope.
FAQ
What is the difference between choroid plexus carcinoma and papilloma?
Choroid plexus carcinoma is malignant and grows aggressively, while papilloma is benign and grows slowly. Carcinomas often spread to other areas, requiring intensive treatment. Papillomas usually have a better prognosis and may only need surgical removal.
Can choroid plexus carcinoma be cured?
Treatment can lead to remission, especially with early detection and complete tumor removal. However, the prognosis depends on factors like age, tumor spread, and genetic mutations. Regular follow-ups are essential to monitor for recurrence.
Are there any lifestyle changes that can help during recovery?
Yes, maintaining a healthy diet, staying physically active, and managing stress can support recovery. Joining support groups or seeking counseling can also help you cope emotionally. Always follow your doctor’s recommendations for post-treatment care.
How can I support a loved one with choroid plexus carcinoma?
Offer emotional support by listening and being present. Help with daily tasks and attend medical appointments if possible. Encourage them to join support groups or seek professional counseling. Educate yourself about the condition to better understand their needs.
Is genetic testing necessary for choroid plexus carcinoma?
Genetic testing can provide valuable insights, especially if you have a family history of Li-Fraumeni syndrome. It helps doctors tailor treatment plans and predict outcomes. Discuss this option with your healthcare provider to determine if it’s right for you.
---
ℹ️ Explore more: Read our Comprehensive Guide to All Known Cancer Types for symptoms, causes, and treatments.
See Also
Exploring Adrenocortical Adenoma: Symptoms And Treatment Options
Anal Cancer: Key Symptoms And Causes You Should Know
Carcinoid Syndrome: Symptoms And Key Information Explained
Essential Insights About Carcinoid Tumors And Their Impact
Adrenocortical Carcinoma: Recognizing Symptoms And Important Facts

