LGL Leukemia: Key Symptoms, Diagnosis & Treatment Tips
Large granular lymphocytic leukemia is a rare blood cancer that affects your immune system. It often goes undiagnosed because symptoms can be mild or absent. This condition is most common in older adults, with an estimated 0.2 to 0.72 cases per million people annually. You may experience health challenges like anemia, chronic neutropenia, or autoimmune diseases such as rheumatoid arthritis. These issues can lead to fatigue, infections, or an enlarged spleen. Recognizing these signs early helps you seek timely medical care and manage the disease effectively.
Key Takeaways
Look for signs like tiredness, infections, and low red blood cells. Finding these early can help you get care quickly.
Learn about the two main kinds of large granular lymphocytic leukemia: T-cell and NK-cell. Knowing your kind helps pick the best treatment.
Eat healthy foods and exercise often. These habits can make you stronger and help your body fight sickness.
Keep learning about your illness and talk to your doctor often. This helps you take better care of yourself.
Think about joining clinical trials to try new treatments. Talk with your doctor about the good and bad sides of it.
What Is Large Granular Lymphocytic Leukemia?
Overview of the Disease
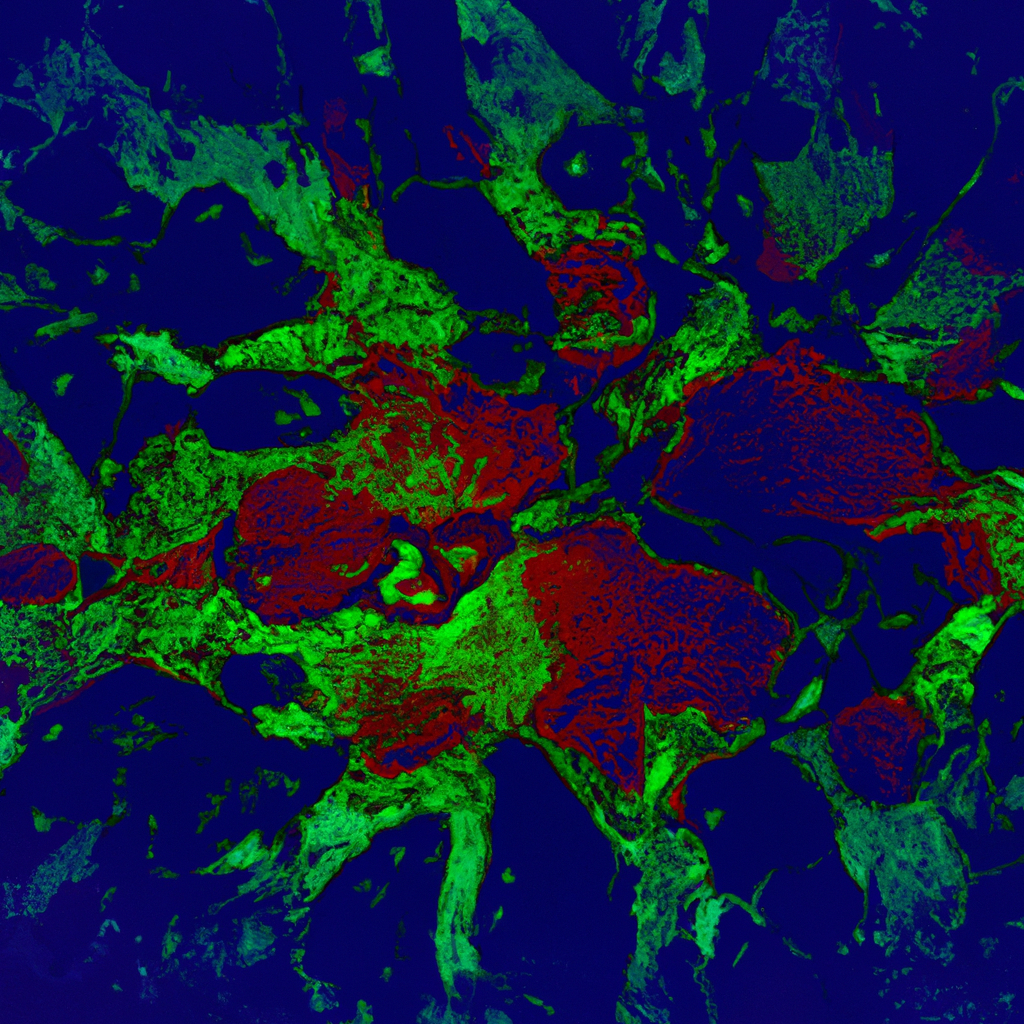
Large granular lymphocytic leukemia is a chronic cancer that affects your blood and bone marrow. It primarily targets mature white blood cells, specifically T-cells and natural killer cells. Under a microscope, these cells appear larger than normal and contain granules, which give the disease its name. This condition often develops in adults over 60 years old and is closely associated with autoimmune disorders. Common symptoms include fatigue, anemia, easy bruising, and frequent infections. Early recognition of these signs can help you seek timely medical care.
Note: Large granular lymphocytic leukemia differs from other types of leukemia because it affects T-cells or natural killer cells, unlike chronic lymphocytic leukemia, which impacts B-cells.
Types of LGL Leukemia
There are two main types of large granular lymphocytic leukemia:
T-cell Large Granular Lymphocytic Leukemia: This is the most common form and involves T-cells, which play a key role in your immune response.
Natural Killer (NK) Cell Leukemia: This rare type affects natural killer cells, which help your body fight infections and tumors.
Both types share similar symptoms but may require different treatment approaches. Understanding the type of LGL leukemia you have is essential for effective management.
Affected Cells | Notes | |
|---|---|---|
Large Granular Lymphocytic Leukemia (LGL) | T cells or natural killer cells | Distinct from CLL, which affects B cells |
Chronic Lymphocytic Leukemia (CLL) | B cells | Primarily affects lymphocytes called B cells |
Affected Populations
Large granular lymphocytic leukemia primarily affects older adults. The average age at diagnosis is around 66.5 years. Most patients are over 60, and fewer than 25% are younger than 50. This condition rarely occurs in individuals under 30 and almost never in children. Autoimmune disorders, such as rheumatoid arthritis or Sjogren syndrome, are present in about 20% of cases before diagnosis. If you belong to an older age group or have a history of autoimmune diseases, you may face a higher risk of developing this condition.
Symptoms of Large Granular Lymphocytic Leukemia

Common Symptoms
Large granular lymphocytic leukemia often presents with symptoms that can affect your daily life. Fatigue is one of the most frequently reported issues. You may feel tired even after adequate rest. Many patients also experience flu-like symptoms, such as body aches and chills, which can occur even without an infection. Changes in blood cell counts are another hallmark of this condition. A decline in red blood cells, known as anemia, can lead to weakness and pale skin. Chronic neutropenia, or a low concentration of neutrophils, increases your risk of infections.
Other common symptoms include:
Recurrent infections
Fever
Night sweats
Unintended weight loss
Moderate enlargement of the spleen (splenomegaly), which occurs in up to half of patients
These symptoms may develop gradually, making them easy to overlook. Paying attention to these signs can help you seek medical advice early.
Less Common Symptoms
Some symptoms of large granular lymphocytic leukemia occur less frequently but may still impact your health. Autoimmune diseases, such as Sjogren syndrome or Hashimoto’s disease, can develop alongside this condition. In aggressive cases, you may notice an enlargement of the liver or spleen. Swollen lymph nodes are rare but possible.
Symptom | Frequency |
|---|---|
Enlargement of the liver | Rarely occurs |
Swollen lymph nodes | Rarely occurs |
Autoimmune diseases | May include Sjogren syndrome, systemic lupus erythematosus, and Hashimoto’s disease |
If you experience these symptoms, it is important to discuss them with your healthcare provider.
When to Seek Immediate Medical Attention
Certain symptoms require urgent medical attention. Recurrent infections, high fever, and night sweats may indicate a worsening of your condition. Significant changes in blood cell counts, such as severe anemia or neutropenia, can also signal a need for immediate care. Unintended weight loss is another red flag that should not be ignored.
If you notice any of these symptoms, contact your doctor promptly. Early intervention can prevent complications and improve your quality of life.
Diagnosing Large Granular Lymphocytic Leukemia
Medical History and Physical Examination
Diagnosing large granular lymphocytic leukemia begins with your doctor reviewing your medical history and performing a physical examination. They will ask about your symptoms, such as fatigue, infections, or weight loss, and check for signs like an enlarged spleen or swollen lymph nodes. If you have a history of autoimmune diseases, such as rheumatoid arthritis, this information can help guide the diagnosis. A thorough physical exam allows your doctor to identify potential warning signs and decide on the next steps for testing.
Blood Tests and Laboratory Work
Blood tests play a critical role in diagnosing large granular lymphocytic leukemia. A complete blood count (CBC) measures the levels of white blood cells, red blood cells, and platelets. Low red blood cell or platelet counts, combined with a high white blood cell count, may indicate this condition. Flow cytometry helps distinguish between T-cell and NK-cell subtypes by analyzing the characteristics of the affected cells. Genetic testing, including T-cell receptor (TCR) gene rearrangement analysis, confirms whether the abnormal cells originated from the same parent cell. These tests not only confirm the diagnosis but also rule out other disorders.
Diagnostic Test | Purpose |
|---|---|
Complete blood count (CBC) with differential | Measures the number of each type of blood cell. |
Peripheral blood smear | Tests for abnormal blood cells. |
Flow cytometry | Analyzes the characteristics of cells. |
Genetic testing | Identifies genetic mutations related to LGL leukemia. |
T-cell receptor (TCR) gene rearrangement analysis | Tests for genetic problems affecting T-cells. |
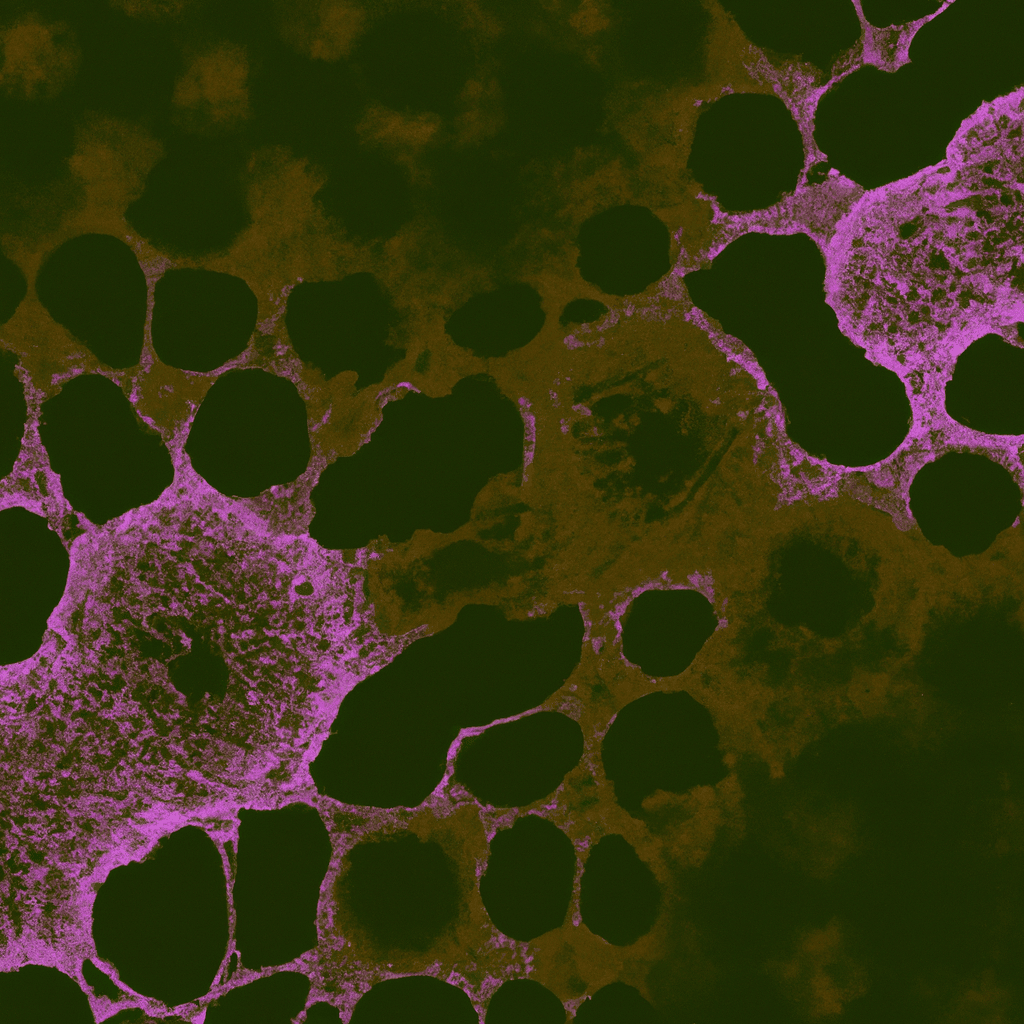
Bone Marrow Biopsy and Other Diagnostic Tools
A bone marrow biopsy may be necessary to confirm the diagnosis or rule out other conditions. During this procedure, your doctor removes a small sample of bone marrow, usually from your hip bone, to examine under a microscope. This test checks for abnormal cells and helps differentiate large granular lymphocytic leukemia from other diseases, such as myelodysplastic syndrome. Although not always required, a bone marrow biopsy is often performed early in the diagnostic process to ensure an accurate diagnosis.
Treatment Options for Large Granular Lymphocytic Leukemia
Immunosuppressive Therapies
Immunosuppressive therapy is often the first line of treatment for large granular lymphocytic leukemia. These therapies work by reducing the activity of your immune system, which helps control the abnormal white blood cells causing symptoms. Commonly used medications include:
Methotrexate: This drug suppresses the immune response and slows the growth of cancer cells. It can lead to partial or complete symptom relief in some patients.
Cyclosporine: This medication inhibits specific white blood cells that contribute to the disease.
Cyclophosphamide: In cases where other treatments are less effective, this drug may be used to manage symptoms.
Your doctor will choose the most suitable therapy based on your condition and response to treatment.
Supportive Treatments
Supportive treatments aim to manage symptoms and improve your quality of life. These therapies do not target the disease directly but help address complications caused by it. For example, granulocyte-colony stimulating factor (G-CSF) can increase your neutrophil count, reducing the risk of infections. Steroids like prednisone may support bone marrow function and reduce inflammation.
Other supportive options include:
Blood transfusions to boost red blood cell or platelet levels.
Colony-stimulating factors to enhance immune function.
Vitamin D and folate supplements to support overall health.
These treatments can help you feel better and maintain a more active lifestyle.
Criteria for Starting Treatment
Not all cases of large granular lymphocytic leukemia require immediate treatment. Doctors typically monitor your condition until specific criteria are met. Treatment usually begins if:
Your absolute neutrophil count drops below 0.5 cellsx10E9/L.
Hemoglobin levels fall below 8.0 g/dL, or you need frequent blood transfusions.
Platelet counts decrease to less than 20 cellsx10E9/L.
You may also need treatment if you experience moderate to severe neutropenia, symptomatic anemia, or autoimmune conditions requiring therapy. Regular check-ups with your healthcare provider ensure timely intervention when necessary.
Emerging Therapies and Clinical Trials
Researchers are constantly exploring new treatments for large granular lymphocytic leukemia. Emerging therapies focus on improving outcomes and reducing side effects. These treatments often target the underlying mechanisms of the disease, such as immune system dysfunction or genetic mutations. For example, targeted therapies aim to block specific pathways that allow abnormal cells to grow. Immunotherapy, which enhances your body’s natural defenses, is another promising area of research.
Clinical trials play a vital role in advancing these therapies. These studies test the safety and effectiveness of new treatments in real-world settings. By participating in a clinical trial, you may gain access to cutting-edge therapies that are not yet widely available. Researchers also use these trials to gather valuable data that can improve future treatments.
If you are interested in clinical trials, several resources can help you find opportunities:
Search for studies by disease, terms, or location at ClinicalTrials.gov.
Contact the NIH Patient Recruitment Office at (800) 411-1222 for information about trials at the NIH Clinical Center.
Explore additional trials on the NORD Clinical Trials website.
Before joining a trial, discuss the potential benefits and risks with your healthcare provider. They can help you decide if a trial is the right choice for your situation. Clinical trials not only offer hope for better treatments but also contribute to the broader understanding of large granular lymphocytic leukemia.
Tip: Staying informed about emerging therapies and clinical trials can empower you to make proactive decisions about your care.
Living with Large Granular Lymphocytic Leukemia
Prognosis and Long-Term Outlook
The prognosis for large granular lymphocytic leukemia is generally positive. Many individuals live for years after their diagnosis. Studies show that the median overall survival is around 9 to 10 years. This means half of the patients live longer than this timeframe. Several factors influence your prognosis, including your age, overall health, and how well you respond to treatment. The presence of conditions like anemia or neutropenia can also affect your outlook. Regular monitoring and timely treatment adjustments can help improve your long-term health.
Tip: Staying informed about your condition and maintaining open communication with your healthcare provider can help you manage your prognosis effectively.
Lifestyle Adjustments
Making lifestyle changes can improve your quality of life with large granular lymphocytic leukemia. A balanced diet rich in fruits, vegetables, and whole grains supports your immune system and overall health. Regular exercise, such as walking or yoga, enhances cardiovascular health and reduces stress. Practicing good hygiene and avoiding environmental toxins can lower your risk of infections. These adjustments not only help you feel better but also support your body in managing the disease.
Here are some practical tips:
Eat nutrient-dense foods to strengthen your immune system.
Stay active with moderate exercise to boost energy levels.
Avoid smoking and limit exposure to harmful chemicals.
Small changes in your daily routine can make a big difference in your well-being.
When to Consult a Healthcare Provider
You should contact your healthcare provider if you notice symptoms that suggest your condition is worsening. These may include increased fatigue, frequent infections, or significant weight loss. If you are already receiving treatment, report any new or worsening symptoms promptly. Early communication with your doctor ensures timely intervention and helps prevent complications.
Note: Regular check-ups are essential even if you feel well. They allow your doctor to monitor your condition and adjust your treatment plan as needed.
Large granular lymphocytic leukemia can feel overwhelming, but you can manage it effectively with the right approach. Focus on these key steps:
Get an accurate diagnosis and attend regular check-ups to monitor your condition.
Follow your prescribed treatment plan, including medications and therapies.
Make lifestyle changes, such as eating a balanced diet and staying active, to support your overall health.
Seek supportive care to address symptoms and improve your quality of life.
By staying proactive and consulting your healthcare provider, you can improve your well-being and live a fulfilling life.
FAQ
What causes large granular lymphocytic leukemia?
The exact cause remains unknown. However, researchers believe genetic mutations and immune system dysfunction play a role. Autoimmune diseases, such as rheumatoid arthritis, may increase your risk. Discussing your medical history with your doctor can help identify potential contributing factors.
Is large granular lymphocytic leukemia curable?
Currently, there is no cure. However, treatments like immunosuppressive therapy and supportive care can manage symptoms effectively. Many patients live for years with proper medical care and regular monitoring.
How often should you see your doctor after diagnosis?
You should schedule regular check-ups every 3 to 6 months. These visits allow your doctor to monitor your condition, adjust treatments, and address any new symptoms. Follow your doctor’s recommendations for the best outcomes.
Can lifestyle changes improve your condition?
Yes, lifestyle changes can help. Eating a balanced diet, staying active, and practicing good hygiene can strengthen your immune system. Avoiding smoking and reducing stress also support your overall health.
Tip: Small adjustments in your daily routine can make a big difference in managing symptoms.
Are clinical trials a good option for treatment?
Clinical trials offer access to new therapies and contribute to medical research. They may benefit you if standard treatments are less effective. Always discuss the risks and benefits with your healthcare provider before enrolling in a trial.
Note: Visit ClinicalTrials.gov to explore available trials.
See Also
A Simple Guide to B-Cell Prolymphocytic Leukemia
Anaplastic Large Cell Lymphoma: Definition and Treatment Options
A Clear Explanation of Diffuse Large B-Cell Lymphoma
Exploring Chronic Lymphocytic Leukemia: Key Facts and Insights
Follicular Lymphoma: Symptoms and Important Information to Know

