How Telehealth Expands Healthcare Access for Underserved Communities

You may face challenges when trying to see a doctor, especially if you live far from clinics or lack transportation. Telehealth changes this by letting you connect to healthcare providers from home. In recent years, more people in underserved communities have started using telehealth. For example:
Telehealth visits rose by over 3,800% during the pandemic.
Now, 22% of outpatient visits happen virtually, compared to less than 1% before 2020.
Rural patients reach more specialists thanks to better internet access.
The Role of Telehealth in Reaching Underserved Populations means you can get care without long trips or high costs.
Key Takeaways
Telehealth connects you with healthcare providers from home, making it easier to access care without long trips.
Underserved communities, including rural areas and low-income groups, face significant healthcare challenges, such as provider shortages and transportation issues.
Telehealth reduces costs by eliminating travel expenses and allowing for more affordable virtual visits.
Using telehealth can improve health outcomes by providing regular check-ins for chronic conditions and connecting patients with specialists.
Government support and new policies have made telehealth more accessible, helping to close gaps in healthcare access for vulnerable populations.
Underserved Communities

Who They Are
You may wonder who counts as an underserved community. Health organizations like the CDC and HRSA use clear definitions. The table below shows how they describe these groups:
Definition/Description | Source |
|---|---|
Underserved communities are those that are socially and economically marginalized, often lacking adequate access to medical care. | CDC |
Federally Qualified Health Centers (FQHCs) serve these communities, providing primary care in under-resourced areas. | CDC |
Medically underserved areas/populations are designated by HRSA based on criteria such as too few primary care providers and high poverty rates. | HRSA |
You may belong to one of these groups if you live in a rural area, have a low income, or face other barriers. Here are some examples:
Rural communities
Elderly individuals
Low-literacy populations
Blue-collar workers
Economically disadvantaged groups
Minorities
Individuals with special needs
Homeless individuals
Challenges Faced
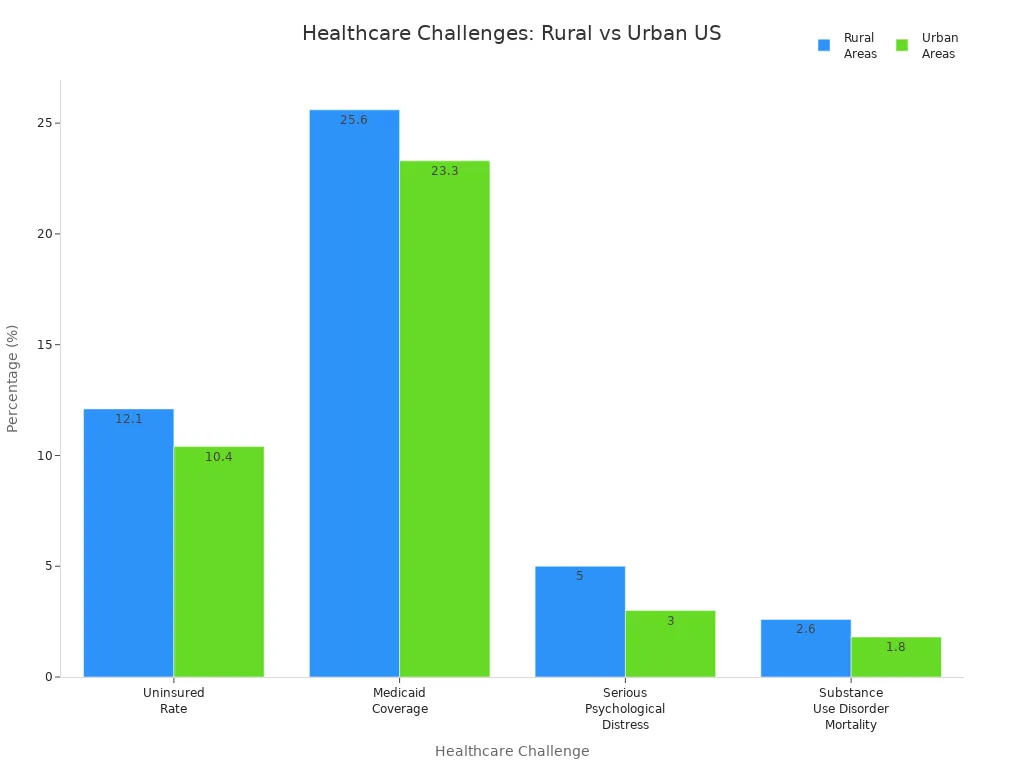
You face many challenges when you try to get healthcare in underserved communities. The table below compares some key issues in rural and urban areas:
Challenge | Rural Areas | Urban Areas |
|---|---|---|
Uninsured Rate | 12.1% | 10.4% |
Medicaid Coverage | 25.6% | 23.3% |
Serious Psychological Distress | 5% (ages 18+) | 3% (ages 18+) |
Substance Use Disorder Mortality | 2.6% (OUD) | 1.8% (OUD) |
Drug Overdose Fatalities Rate | 26.2 per 100,000 population | N/A |
Higher Mortality Rates | Higher for heart disease, cancer | Lower for same conditions |
You may also struggle with language barriers and cultural differences. The table below lists some common challenges:
Challenge | Description |
|---|---|
Socioeconomic Factors | Impact access to healthcare services |
Underfunding of Healthcare | Makes diversity-responsive care difficult |
Language Barriers | Affect communication and access |
Inadequate Cultural Training | Leads to poor communication with patients |
Individual Discrimination | Homophobia or racism can affect patient experiences |
1 in 5 Americans have trouble talking with healthcare providers.
27% of Asian Americans and 33% of Hispanics face similar problems.
Limited English skills mean fewer doctor visits and less preventive care.
Implicit bias can instill distrust in medicine and dissuade patients of color from accessing care. Negative interactions with the healthcare system can lead to feelings of fear and despair, particularly in underserved communities.
Barriers to Care
Distance and Transportation
You may find it hard to get to a doctor if you live far from clinics or hospitals. Many people in rural areas or low-income neighborhoods do not have easy access to public transportation. If you rely on buses, you might miss or reschedule appointments because of unreliable service. The table below shows how transportation affects healthcare visits:
Study | Findings |
|---|---|
Silver et al. (2012) | 23.5% missed or rescheduled visits due to transportation; 31.6% blamed buses |
Syed et al. (2013) | Transportation barriers prevent low-income and underinsured patients from care |
Kavanagh et al. (1991) | Car ownership helps people attend clinic appointments |
Many patients miss appointments because they cannot get a ride. Some clinics now use ride services like Lyft to help, which has reduced waiting times and costs.
You may also see that studies link transportation problems to missed appointments. If you do not have a car or live far away, getting care becomes even harder.
Provider Shortages
You may notice that your community does not have enough doctors or specialists. This problem is common in underserved areas. Many health centers report that patients need better access to specialty care, such as rheumatology. Some providers feel uncomfortable starting important treatments because they cannot refer patients to specialists.
Provider shortages make it hard for you to get the care you need.
Over half of health center directors say their patients lack access to certain specialists.
You may wait longer or travel farther for care.
Cost and Convenience
Paying for healthcare can be a big challenge. If you have a low income, out-of-pocket costs can add up quickly. The table below shows average costs for families:
Income Level | Average Out-of-Pocket Costs |
|---|---|
Poor and Near-Poor Families | |
Low or Middle-Income Families | $611 |
You may also find it hard to take time off work or arrange childcare for in-person visits. The Role of Telehealth in Reaching Underserved Populations helps by letting you see a doctor from home. Telehealth saves you time, reduces travel, and makes it easier to fit care into your day. If you have trouble moving or lack transportation, telehealth gives you a way to get care without leaving your house.
The Role of Telehealth in Reaching Underserved Populations

Overcoming Distance
You may live in a place where the nearest doctor is hours away. The Role of Telehealth in Reaching Underserved Populations helps you get care without leaving your home. Telemedicine makes it possible for you to talk to a doctor using a phone, tablet, or computer. This is especially helpful if you live in a rural area or a medical desert, where clinics and hospitals are far apart.
Telemedicine brings healthcare to your doorstep, no matter how remote your location.
You can access essential medical services without long travel times.
Patients in isolated communities, such as Native American reservations, now receive specialty care and faster treatment through telehealth.
Here is how telehealth has improved care for Native American and other isolated communities:
Benefit/Challenge | Description |
|---|---|
Access to Specialty Care | Telehealth provides access to specialized medical services that may not be available locally. |
Faster Treatment | You can receive quicker consultations and treatments through telehealth services. |
Consistent Care | Regular follow-ups and ongoing care are easier, improving health outcomes. |
Infrastructural Barriers | Some communities still face challenges with internet and technology for telehealth. |
Acceptance Issues | Not everyone is comfortable using telehealth technology yet. |
Improved Health Outcomes | Studies show better management of chronic diseases among Native Americans using telehealth. |
You may also benefit from telehealth if you have a chronic condition. Telehealth allows you to check in with your doctor regularly, so you can manage diseases like diabetes or high blood pressure. You do not need to travel far for every appointment. This saves you time and helps you stay healthy.
Telehealth provides regular virtual check-ins for chronic conditions.
It eliminates the need for long-distance travel, reducing time and costs.
You get continuous monitoring and follow-up care, which is essential for managing chronic diseases.
If you are an older adult or have trouble moving, telehealth makes it easier to get care. You can talk to your doctor from home, which means you do not have to worry about transportation or stairs at a clinic.
Telemedicine enhances healthcare access for seniors, minimizing the need for in-person visits.
Virtual consultations address transportation and mobility challenges.
Expanding Provider Access
The Role of Telehealth in Reaching Underserved Populations also helps you see more types of doctors. If your local clinic does not have a specialist, telehealth connects you with experts from other places. During the COVID-19 pandemic, telehealth visits increased across many specialties in the United States. This means you can get care for more health problems without waiting months or traveling far.
Findings | Description |
|---|---|
Expansion of Telehealth | The COVID-19 pandemic led to a big increase in telemedicine across various specialties. |
Improved Access | Telehealth removes barriers like transportation and distance, helping underserved populations. |
Demographic Changes | More young people and patients with Medicaid or Medicare used telehealth. |
No-Show Rates | Patients missed fewer appointments with telehealth than with in-person visits. |
You may find that telehealth rooms in clinics or community centers help you connect with specialists. These rooms have the equipment you need for a video visit, even if you do not have internet at home. Telehealth also supports multidisciplinary care. Your primary doctor, a specialist, and even a mental health provider can work together to help you.
Telehealth services reduce travel time and connect you with specialists.
They address healthcare worker shortages in your area.
Telemedicine enables healthcare providers from different specialties to collaborate remotely.
Here are some real-world examples of telehealth making a difference:
Case Study | Location | Key Outcomes |
|---|---|---|
Hope Foundation | Bangladesh | Nearly 500,000 patient contacts; successful telehealth for refugees; government support. |
Precious Gems | Nigeria | Enhanced access for rural patients; successful diagnosis and treatment; local capacity built. |
BORNE Initiative | Ethiopia | Increased stroke treatment rates; new stroke units; training for local providers. |
Improving Affordability
The Role of Telehealth in Reaching Underserved Populations can also help you save money. Telehealth visits usually cost less than in-person visits. You do not have to pay for gas, bus fare, or parking. You also avoid missing work or paying for childcare.
Telehealth resulted in total service cost savings of over $24,000 in just seven months for one program.
The average cost per telehealth visit was $430, compared to $835 for a traditional visit.
Patients save between $19 and $121 per visit, mostly by avoiding unnecessary emergency room trips.
If you have a low income, you are not alone in using telehealth. Many people with lower incomes use telemedicine to get care:
Income Level (FPL) | |
|---|---|
Less than 100% | 33.1 |
100% to less than 200% | 32.1 |
400% or greater | 40.7 |
Government policies and funding also play a big role in making telehealth affordable. During the COVID-19 pandemic, new laws made it easier for you to use telehealth. All states now reimburse for live audio-video telehealth under Medicaid. Federal funds have helped bring high-speed internet to more homes and clinics, making telehealth possible for more people.
The Role of Telehealth in Reaching Underserved Populations does more than save money. It helps you get care that fits your needs, whether you live far from a clinic, need a specialist, or want to avoid high costs. Telehealth gives you more choices and better access to healthcare.
Telehealth gives you more ways to see a doctor and makes healthcare fairer for everyone. You can see this in the table below:
Benefit | Details |
|---|---|
More people from different backgrounds now get care, including older adults and Medicaid patients. | |
Removal of Barriers | You avoid long trips, missed work, and parking problems. |
Support for Vulnerable Groups | Telehealth helps people with chronic illnesses and those who need extra support. |
You can expect even more progress in the future:
Remote monitoring will help manage chronic conditions.
Telehealth will keep closing gaps and bringing better care to your community.
FAQ
What do you need for a telehealth visit?
You need a phone, tablet, or computer with internet. Some clinics offer telehealth rooms if you do not have these at home. You may also need a private space for your call.
Is telehealth safe and private?
Yes, telehealth uses secure technology to protect your information. Doctors follow privacy laws like HIPAA.
Your health details stay safe during virtual visits.
Can you get prescriptions through telehealth?
You can get many prescriptions after a telehealth visit. Doctors can send orders directly to your pharmacy. Some medicines may still require an in-person visit.
Who benefits most from telehealth?
People in rural areas
Older adults
Those with limited transportation
Patients with chronic conditions
You may find telehealth especially helpful if you face barriers to in-person care.
See Also
Recognizing Symptoms and Treatments for Conjunctival Melanoma
Identifying Symptoms and Treatment Options for Choroid Plexus Carcinoma
Join Banish Cancer – A Place of Hope and Resilience
Exploring Symptoms and Treatment Approaches for Duodenal Cancer

